Understanding Medicaid Home and Community Services: A Primer 2010 Edition
2010 Edition
U.S. Department of Health and Human Services
Office of the Assistant Secretary for Planning and Evaluation
U.S. Department of Health and Human Services
Office of the Assistant Secretary for Planning and Evaluation
200 Independence Avenue, Washington, DC 20201
Understanding Medicaid
Home and Community Services:
A Primer
Oce of the Assistant Secretary for Planning and Evaluation
The Oce of the Assistant Secretary for Planning and Evaluation (ASPE) is the principal advisor to the Secre-
tary of the Department of Health and Human Services (HHS) on policy development issues, and is responsible
for major activities in the areas of legislative and budget development, strategic planning, policy research and
evaluation, and economic analysis.
ASPE develops or reviews issues from the viewpoint of the Secretary, providing a perspective that is broader
in scope than the specic focus of the various operating agencies. ASPE also works closely with the HHS
operating divisions. It assists these agencies in developing policies, and planning policy research, evaluation
and data collection within broad HHS and administration initiatives. ASPE often serves a coordinating role for
crosscutting policy and administrative activities.
ASPE plans and conducts evaluations and research—both in-house and through support of projects by ex-
ternal researchers—of current and proposed programs and topics of particular interest to the Secretary, the
Administration and the Congress.
Oce of Disability, Aging and Long-Term Care Policy
The Oce of Disability, Aging and Long-Term Care Policy (DALTCP), within ASPE, is responsible for the develop-
ment, coordination, analysis, research and evaluation of HHS policies and programs which support the inde-
pendence, health and long-term care of persons with disabilities—children, working aging adults, and older
persons. DALTCP is also responsible for policy coordination and research to promote the economic and social
well-being of the elderly.
In particular, DALTCP addresses policies concerning: nursing home and community-based services, informal
caregiving, the integration of acute and long-term care, Medicare post-acute services and home care, man-
aged care for people with disabilities, long-term rehabilitation services, children’s disability, and linkages
between employment and health policies. These activities are carried out through policy planning, policy and
program analysis, regulatory reviews, formulation of legislative proposals, policy research, evaluation and data
planning.
This report was prepared under contract #HHS-100-03-0025 between HHS’s ASPE/DALTCP and RTI International.
For additional information about this subject,
you can visit the DALTCP home page at
http://aspe.hhs.gov/_/oce_specic/daltcp.cfm
or contact the ASPE Project Ocer,
Emily Roseno, at HHS/ASPE/DALTCP
Room 424E, H.H. Humphrey Building,
200 Independence Avenue, S.W., Washington, D.C. 20201
Her e-mail address is: Emily.Roseno@hhs.gov
Understanding Medicaid
Home and Community Services: A Primer
2010 Edition
Project Director
Janet O’Keee
Co-Authors
Janet O’Keee
Paul Saucier
Beth Jackson
Robin Cooper
Ernest McKenney
Suzanne Crisp
Charles Moseley
Managing Editor
Christine O’Keee
ASPE Project Ocer
Emily Roseno
Dear Reader,
We are pleased to present this updated version of the Medicaid Home and Community
Services Primer. Over the past 10 years, the Primer has fullled its primary purpose of in-
forming key stakeholders about the statutes and regulations governing the nancing and
provision of Medicaid home and community services. Specically the Primer was designed:
• To explain how the Medicaid program can be used to expand access to a broad range
of home and community services and supports for people of all ages with disabilities,
and to promote consumer authority and control over their services; and
• To encourage a fundamental approach to the support of people with disabilities that
minimizes reliance on institutions and maximizes community integration in the most
cost-eective manner.
Medicaid policy has continued to evolve over the last 10 years to better support options
for community living by people of all ages with disabilities and/or chronic health condi-
tions. The Decit Reduction Act of 2005 and the Patient Protection and Aordable Care
Act of 2010 both created new options for states to provide home and community services
without having to secure a federal waiver. In addition, the Centers for Medicare & Medicaid
Services (CMS) has made numerous changes to the program to make it easier for individu-
als to live in the community, such as authorizing coverage of one-time transition expenses
for home and community-based services (HCBS) waiver participants.
The current edition of the Primer has been updated to include all relevant statutory, regula-
tory and other policy changes that have occurred in the last 10 years. Given the signicance
of the recent changes in Medicaid, I believe the Primer will be an ever more useful tool for
all those working to ensure that people with disabilities can live in the most integrated set-
tings appropriate to their needs.
This updated version of the Primer would not have been possible without the commitment
and hard work of many people. In particular I want to recognize and thank the CMS sta
who took time out of their busy schedules to review each chapter of the Primer to ensure
that the content was accurate and consistent with current policy.
As the Medicaid program continues to evolve to better meet the needs of its beneciaries,
new policy and clarications of existing policy will be made subsequent to the publication
of the Primer. Information about policy changes will be disseminated through State Medic-
aid Director Letters, the Federal Register, and the State Medicaid Manual, which are avail-
able on the CMS website.
Richard Frank
Deputy Assistant Secretary for Planning and Evaluation
Disability, Aging, and Long-Term Care Policy
DEPARTMENT OF HEALTH & HUMAN SERVICES Oce of the Secretary
Washington, D.C. 20201

Acknowledgments
ASPE acknowledges with gratitude the assistance
of the Centers for Medicare & Medicaid Services
in completing the revised Primer. In particular, we
would like to thank CMS sta who reviewed each
chapter to ensure technical accuracy and consis-
tency: Mary Sowers, Roy Trudel, Dan Timmel, Kathy
Poisal, Carey Appold, Peggy Clark, Carrie Smith, El-
len Blackwell, Melissa Harris, Anita Yuskauskas, and
Kenya J. Cantwell. We also thank CMS for funding
the development of the appendix on quality man-
agement systems.

Table of Contents
Introduction
The 2010 Edition of the Primer ........................................................................................................................ 13
Chapter 1
Medicaid Coverage of Home and Community Services: Overview ................................................... 19
Chapter 2
Financial Eligibility Rules and Options .......................................................................................................... 37
Chapter 3
Determining Service Eligibility ........................................................................................................................ 63
Chapter 4
Options for Designing Service Coverage: General Considerations .................................................... 85
Chapter 5
Providing Medicaid Services in Community Residential Settings ....................................................123
Chapter 6
Transitioning People from Institutions to the Community .................................................................151
Chapter 7
Participant-Directed Services and Supports ............................................................................................175
Chapter 8
Medicaid Authorities for Delivering Home and Community
Services through Risk-Based Managed Care Systems ..........................................................................211
Appendix:
Medicaid HCBS Quality ....................................................................................................................................231

11
Introduction to the 2010 Edition of the Primer
Dedication
Gary Smith, the principal author of the original Primer,
died in November 2007.
Gary was the preeminent expert on Medicaid Policy and
was a resource to hundreds of people all over the country:
researchers, policymakers, Centers for Medicare & Medic-
aid Services sta, state sta, and advocates. He was always
generous with his time and his expertise and never let a
request for help go unanswered. He is greatly missed—as
a colleague and a friend.
Although millions of people with disabilities have never
heard his name, his work in public policy has made an
ongoing positive dierence in their lives.
We dedicate this edition of the Primer to his memory.
13
Introduction to the 2010 Edition of the Primer
Introduction to the 2010 Edition of the Primer
The Primer was rst published in 2000—one year after the Supreme Court decision in Olmstead v. L.C. af-
rmed the right of persons with disabilities to live in the most integrated setting (see Box).
1
A major purpose of
the original Primer was to provide information about how the Medicaid program could be used to assist states
in meeting the principles set out in the Olmstead decision.
In the 10 years since the Primer was published, Medicaid policy regarding the provision of home and commu-
nity services has evolved considerably. During this period, the Centers for Medicare & Medicaid Services (CMS)
awarded hundreds of grants to support states’ eorts to improve access to—and the availability and quality
of—home and community services. The grants were also aimed at increasing Medicaid participants’ control
over their services and supports.
2
The Olmstead Decision
3
The Supreme Court ruled that “Unjustied isolation . . . is properly regarded as discrimination based on disability.”
It observed that (a)“institutional placement of persons who can handle and benet from community settings
perpetuates unwarranted assumptions that persons so isolated are incapable or unworthy of participating in
community life,” and (b)“connement in an institution severely diminishes the everyday life activities of individu-
als, including family relations, social contacts, work options, economic independence, educational advancement,
and cultural enrichment.”
Under the Court’s decision, states are required to provide community-based services for persons with disabilities
who would otherwise be entitled to institutional services when (a)the state’s treatment professionals reason-
ably determine that such placement is appropriate; (b)the aected persons do not oppose such treatment; and
(c)the placement can be reasonably accommodated, taking into account the resources available to the state and
the needs of others who are receiving state-supported disability services. The Court cautioned, however, that
nothing in the Americans with Disabilities Act (ADA) condones termination of institutional settings for persons
unable to handle or benet from community settings. Moreover, the state’s responsibility, once it provides
community-based treatment to qualied persons with disabilities, is not unlimited.
Under the ADA, states are obliged to “make reasonable modications in policies, practices, or procedures when
the modications are necessary to avoid discrimination on the basis of disability, unless the public entity can
demonstrate that making the modications would fundamentally alter the nature of the service, program or ac-
tivity.” The Supreme Court indicated that the test as to whether a modication entails “fundamental alteration” of
a program takes into account three factors: the cost of providing services to the individual in the most integrated
setting appropriate, the resources available to the state, and how the provision of services aects the ability of
the state to meet the needs of others with disabilities.
The rst edition of the Primer emphasized that people of all ages with disabilities want the same opportunities
that every American wants: to thrive, not just survive. They want to live in their own homes and make deci-
sions about daily activities; they want to go to school, attend church services, work, and participate fully in
recreational and other community activities. People with disabilities have not always been allowed this birth-
right; society has too often focused on their disabilities rather than their abilities.
Over the past 2 decades, and particularly since the Olmstead decision, progress has been made. People with
disabilities are now recognized as being able to live in their own homes and other community settings, and to
14 Understanding Medicaid Home and Community Services: A Primer
lead satisfying and productive lives when provided
with appropriate services and supports. Much re-
mains to be done to enable all persons with disabili-
ties to do so.
Medicaid: An Evolving Program
with Considerable State Flexibility
Medicaid is the major source of public funding for
long-term services and supports provided in home
and community settings. Medicaid was enacted
in 1965 as a companion program to Medicare.
4
It
was designed as a joint Federal-state entitlement
providing primarily medical care to low-income
Americans.
5
When rst enacted, Federal Medicaid
funding for meeting long-term care needs was
available mainly when individuals were placed in an
institution (e.g., a nursing home), with few avenues
for supporting them in their homes and communi-
ties. State funds were used to pay for “home care”
programs, but only on a limited basis.
6
In the 45 years since its enactment, Medicaid’s “insti-
tutional bias” has been steadily diminished through
numerous amendments to Federal laws and policy.
Since the early 1980s, there has been a steady
increase in the options available to states to secure
Federal Medicaid funding for comprehensive home
and community services. The Decit Reduction Act
of 2005 (DRA-2005) authorized a new optional State
Plan authority for states to provide home and com-
munity-based services (HCBS) without a waiver, and
most recently, the Patient Protection and Aordable
Care Act (hereafter referred to as the Aordable
Care Act), enacted in 2010, authorized an additional
optional State Plan authority to provide “Communi-
ty-based Attendant Services and Supports”—called
the Community First Choice Option.
Over the past two decades, states have greatly
expanded the availability of home and community
services. The portion of Medicaid long-term care
spending directed to home and community ser-
vices has been increasing steadily by one to three
percentage points each year as states continue to
invest more resources in alternatives to institutional
care. In 2009, home and community services ac-
counted for 45 percent of total Medi caid long-term
care spending.
7
Many states are using innovative
and scally responsible methods to enable more
persons with disabilities to receive necessary ser-
vices in their communities instead of in institutions.
The Medicaid program provides many options to
increase the availability of home and community
services while controlling costs. As states work
toward the goal of integrating people of all ages
with all types of disabilities into their communities,
they may need to go through a process of funda-
mentally rethinking how programs serving people
with disabilities are structured and how resources
are allocated.
The chapters in this Primer stress that when de-
ciding how best to use the Medicaid program to
expand the provision of home and community
services, states need to consider their unique needs,
resources, and social, political, and economic envi-
ronments. Additionally, all of these factors must be
considered in the context of the technological and
demographic changes driving the need for publicly
funded long-term care services and supports.
Key among these changes are advances in medical
technology that have enabled increasing numbers
of people with congenital and acquired disabili-
ties to both survive and live longer lives. A second
change is that the nation’s population is aging. The
group most likely to need long-term care—people
over age 85—is estimated to grow from 5.3 million
in 2006 to nearly 21 million by 2050.
8
Moreover, the aging population includes individuals
who have spent their lives providing informal care
for adult children with intellectual disabilities and
other developmental disabilities (ID/DD, hereafter
referred to as developmental disabilities). Now that
many individuals with developmental disabilities
are outliving their parents, an increase in the num-
ber needing services and support is expected in the
coming years.
10
Finally, most assistance to people
with disabilities is provided by informal caregivers,
typically women. However, continued reliance on
this support in the coming years may be unrealistic,
given high rates of women’s labor force participa-
tion, smaller families, and geographic mobility.
15
Introduction to the 2010 Edition of the Primer
Terminology and Denitions
In this Primer, the term “persons with disabilities” includes persons of all ages—young children, adolescents,
and working age or older adults—with all types of disabilities due to physical and mental impairments and/or
chronic illnesses. Because the Primer’s focus is on Medicaid home and community services, the term “people with
disabilities” refers primarily to those individuals who need long-term care services. However, not all persons with
disabilities need these services.
The service systems for dierent disability groups use dierent terms for the same or similar services. For exam-
ple, the service system for older adults uses long-term care or long-term care services, whereas the service sys-
tem for people with developmental disabilities uses long-term services and supports or just supports. States also
vary in their use of terms: personal care is also called personal assistance or attendant care, which is provided by
personal care providers, personal assistants, personal attendants, and direct care workers, among other names.
To eliminate confusion, the Primer uses terms consistently in all chapters and specically notes when terms are
used interchangeably. When discussing a particular state’s service system, or Federal statutes and regulations,
the Primer uses the specic terms they use. For example, the term home and community-based services is used
only when referring to Federal statutes, regulations, or programs that use this term. In general, the Primer uses
the term home and community services or just services and supports.
A law enacted in October 2010 amended provisions of Federal law to substitute the term “an intellectual disabil-
ity” for “‘mental retardation,” and “individuals with intellectual disabilities” for “the mentally retarded” or “indi-
viduals who are mentally retarded.”
9
Intermediate Care Facilities for Persons with Intellectual Disabilities (ICF/
ID) is the new title for the program formerly known as Intermediate Care Facilities for the Mentally Retarded. The
Primer uses these new terms, except when the former terms are used in the titles of previously published books,
reports, and articles.
To ensure brevity without excessive use of acronyms when referring to systems of care, the Primer generally uses
the shortest term (e.g., long-term care rather than long-term care services and supports).
Finally, many of the Medicaid provisions discussed in the Primer were enacted when the Centers for Medicare &
Medicaid Services was known as the Health Care Financing Administration (HCFA). Throughout the Primer, the
current name—CMS—will be used, even when referring to actions the agency made when it was named HCFA.
16 Understanding Medicaid Home and Community Services: A Primer
Purpose, Audience, and
Organization of the Primer
Medicaid oers a complex and varied set of home
and community service options—with similarly
complex rules and regulations—that can be bewil-
dering for policymakers, state ocials, advocates,
and consumers. Even people who have spent years
working in Medicaid state agencies do not always
understand its many provisions. The extensive
exibility states have to combine these options has
resulted in considerable variation among states’
Medicaid programs. As some wit has put it, “What
state Medicaid programs have most in common is
that they are all dierent.”
The Primer is designed to encourage states to use
the Medicaid program to minimize reliance on
institutions and maximize community integra-
tion for people with disabilities in a cost-eective
manner. Its intended audience is policymakers,
state Medicaid sta, and all stakeholders who wish
to understand how Medicaid can be used—and is
being used—to expand access to a broad range of
home and community services and supports. In ad-
dition to providing comprehensive explanations of
Medicaid home and community service options, the
Primer presents examples of states that have used
them to promote greater community integration of
people with disabilities.
The service options reviewed address program
modications that states can implement as a State
Plan option (without a special waiver of Federal
law), as well as those for which Federal waiver ap-
proval must be obtained. While each chapter has
been written to cover a specic topic, and as such,
can be read independently of the rest of the Primer,
it also assumes an understanding of basic Medicaid
terms and provisions, such as comparability and
statewideness, mandatory and optional services,
State Plan and waiver services. Those unfamiliar
with these basic terms should rst read Chapter 1.
When a topic is covered in depth in one chapter,
that chapter will be referenced in other chapters
that address the topic.
Chapter 1 provides a brief overview of the legisla-
tive and regulatory history of Medi caid’s cover-
age of home and community services and current
spending on these services.
The next two chapters describe the basic elements
of Medicaid’s nancial and service eligibility criteria.
Chapter 2 provides an explanation of Medi caid’s
nancial eligibility criteria, a complex area of Med-
icaid law. It rst discusses the general eligibility
criteria that all Medicaid beneciaries must meet. It
then focuses on the nancial eligibility provisions
most important for receiving services in home and
community settings. The chapter also reviews the
options states can select to ensure that people with
disabilities can support themselves in home and
community settings.
Chapter 3 focuses on Medicaid provisions related
to the health and functional criteria states use to
determine eligibility for State Plan home health
services, State Plan personal care services, State Plan
home and community-based services, and HCBS
waiver programs. The chapter also discusses how
states can design service criteria to ensure that they
appropriately and adequately measure the need
for services and supports among heterogeneous
populations.
Chapters 4 and 5 describe service coverage options.
Chapter 4 presents the major service options for
providing home and community services to people
with disabilities. The factors states need to consider
when choosing among the various options are also
discussed.
Chapter 5 describes coverage options for providing
services in a wide range of residential care settings
that are provider-owned and/or operated, including
foster care, group homes, and assisted living.
Chapters 6 and 7 focus on key policy goals related
to coverage of home and community services.
Chapter 6 discusses factors states need to consider
when developing initiatives to transition institu-
tional residents to home and community settings. It
also presents ways in which Medicaid can be used
to facilitate transitions.

17
Introduction to the 2010 Edition of the Primer
Chapter 7 describes Medicaid options to increase
participants’ choice and control of home and com-
munity services.
Chapter 8 describes options for states to provide
Medicaid home and community services through
managed care delivery systems.
An appendix provides an overview of CMS require-
ments for quality management and improvement
systems for HCBS waivers.
To make the Primer as useful as possible, each chap-
ter includes a Resources section that provides infor-
mation about key publications and links to websites
from which the reader can obtain more detailed
information about the chapter’s topic. The endnotes
for each chapter include not just source citations,
but additional technical information and—in many
cases—web links to these citations and information.
Thus, while the Primer can be read either in hard
copy or online, the online version enables readers to
access a considerable amount of additional infor-
mation.
This Primer has been prepared by the Oce of the
Assistant Secretary for Planning and Evaluation in
the U.S. Department of Health and Human Services,
and reviewed for accuracy by CMS sta. Designed
to serve as a reference guide, it is written in easily
understood language, but with sucient annota-
tion of source material to fulll its technical support
function.
18 Understanding Medicaid Home and Community Services: A Primer
Endnotes
Citations, Additional Information, and Web Addresses
1
Olmstead v. L. C., 119 S.Ct. 2176 (1999).
2
The grants were implemented through several programs, primarily the Systems Change Grants for Commu-
nity Living program.
3
The Olmstead decision interpreted Title II of the ADA and its implementing regulations, which oblige states
to administer their services, programs, and activities “in the most integrated setting appropriate to the needs
of qualied individuals with disabilities” (28 CFR 35.130(d)). Information about the application of the Olm-
stead decision to the Medicaid program is available from the CMS website in State Medicaid Director Letters.
Available at http://www.cms.hhs.gov/SMDL/SMD/list.asp#TopOfPage. Use the word Olmstead to nd the
relevant letters.
4
P.L. 89-97, Title XIX of the Social Security Act.
5
The Federal Government provides matching funds on an open-ended basis for every dollar a state chooses
to spend on Medicaid services.
6
Federal funding through specic programs was sometimes available.
7
Citation: Eiken, S., Sredl, K., Burwell, B., and Gold, L. (2010). Medicaid Long-Term Care Expenditures in FY 2009.
Cambridge, MA: Thomson Reuters. Available at http://www.hcbs.org/moreInfo.php/doc/3326.
8
U.S. Agency on Aging. Statistics available at http://www.aoa.gov/agingstatsdotnet/Main_Site/Data/2008_
Documents/Population.aspx.
9
Called Rosa’s Law (Bill S.2781), signed October 5, 2010, by President Barack Obama.
10
Hubert, J., and Hollins, S. (2002). People with Intellectual Disabilities and Their Elderly Caregivers.
Available at http://www.intellectualdisability.info/life-stages/people-with-intellectual-disabilities-and-their-
elderly-carers/?searchterm=People%20with%20Intellectual%20Disabilities%20and%20Their%20Elderly%20-
Caregivers.

Chapter 1: Medicaid Coverage of Home and Community Services: Overview
19
Guide to Chapter 1
Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 21
Program Evolution and Current Spending Allocations . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 21
Major Features of Medicaid’s Provisions for Home and Community Services . . . . . . . . . . . . . . 23
Mandatory State Plan Services: Home Health . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 23
Mandatory State Plan Services: EPSDT . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 25
Optional State Plan Services: Personal Care . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 25
Optional State Plan Services: Targeted Case Management . . . . . . . . . . . . . . . . . . . . . . . 26
Optional State Plan Home and Community-Based Services . . . . . . . . . . . . . . . . . . . . . . 27
Optional State Plan Services: Community Choice Option . . . . . . . . . . . . . . . . . . . . . . . . .27
Other Optional State Plan Home and Community Services . . . . . . . . . . . . . . . . . . . . . . . 27
The HCBS Waiver Authority . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 28
The Katie Beckett Provision . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 29
The Program of All-Inclusive Care for the Elderly (PACE) . . . . . . . . . . . . . . . . . . . . . . . . . . 30
Resources. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .31
Endnotes: Citations, Additional Information, and Web Addresses . . . . . . . . . . . . . . . . . . . . . . . . 35
21
Chapter 1: Medicaid Coverage of Home and Community Services: Overview
Chapter 1
Medicaid Coverage of Home and Community Services: Overview
Long-term care includes a broad range of health and health-related services, personal care, social and
supportive services, and individual supports. These services can be provided in institutions, an individual’s
home, or in community settings. This chapter recounts the legislative, regulatory, and policy history of
Medicaid coverage of long-term care services and supports. Both institutional care and home and com-
munity services are described, with the latter in greater detail.
1
Introduction
Medicaid is a needs-based, entitlement program that is designed to help states meet the costs of necessary
health care for low-income and medically needy populations. When a Medicaid State Plan is approved by the
Centers for Medicare & Medicaid Services (CMS), states qualify to receive Federal matching funds to nance
Medicaid services (see Box). States have substantial exibility to design their programs within broad Federal
requirements related to eligibility, services, program administration, and provider compensation.
Federal Medical Assistance Percentage (FMAP)
The Federal government’s share of medical assistance expenditures under each state’s Medicaid program, known
as the Federal medical assistance percentage, is determined annually by a formula that compares
the state’s average per capita income level with the national average. States with higher per capita incomes are
reimbursed smaller shares of their costs. By law, FMAP cannot be lower than 50 percent or higher than 83 per-
cent. States are also reimbursed for 50 percent of administrative costs. For scal year 2009, the
FMAP ranged from 50 percent in California and several other states to 75.84 percent in Mississippi.
2
Program Evolution and Current Spending Allocations
When enacted, Medicaid was the medical care extension of Federally-funded programs providing cash assis-
tance for the poor, with an emphasis on dependent children and their mothers, elderly persons, and persons
with disabilities. Legislation in the 1980s expanded Medicaid coverage of low-income pregnant women and
poor children, and extended coverage to some low-income Medicare beneciaries who were not eligible for
cash assistance. From its beginnings as a health care nancing program primarily for welfare recipients, the
Medicaid program has been amended and expanded to cover a wide range of populations and services.
When rst enacted, Medicaid’s main purpose was to cover primary and acute health care services, such as doc-
tor visits and hospital stays. Mandatory coverage for long-term care was limited to skilled nursing facility (SNF)
services for people age 21 or older. States were given the option to cover home health services and private
duty nursing services. In response to the high costs of nursing facility care, combined with criticism of Med-
icaid’s institutional bias, states and the Federal government began to look for ways to provide long-term care
in less restrictive, more cost-eective ways. In 1970, home health services for those entitled to nursing home
care became mandatory. Since that date, Medicaid has evolved into a program that allows states considerable
exibility to cover virtually all long-term care services and supports that people with disabilities need to live

22 Understanding Medicaid Home and Community Services: A Primer
independently in their homes and in a wide range
of community residential care settings.
The Federal Medicaid statute (Title XIX of the Social
Security Act) generally requires states to specify the
amount, duration, and scope of each service they
provide, which must be sucient to reasonably
achieve its purposes. States may not place limits on
services or arbitrarily deny or reduce coverage of
required services solely because of diagnosis, type
of illness, or condition—called the comparability
requirement.
Generally, a State Plan must be in eect throughout
an entire state (i.e., the amount, duration, and scope
of coverage must be the same statewide—called
the “statewideness” requirement). The Social Se-
curity Act has some exceptions, notably (1)states
operating Section (§)1915(c) home and community-
based services (HCBS) waiver programs (hereafter
called HCBS waiver programs) are permitted to
target services by age and diagnosis and can oer
them on a less than statewide basis, and (2)target-
ed case management services oered as an option-
al benet under the State Plan are not subject to the
statewideness requirement. (§1115 Research and
Demonstration waivers can also operate on a less
than statewide basis.)
By 1999, the year of the Olmstead decision, every
state was providing home and community servi ces
under one or more of the available options except
for §1915(i) (which did not become eective until
2007). By then, Medicaid had become the nation’s
major public nancing program for long-term care
for low-income persons of all ages with all types of
physical and mental disabilities.
3
Since 1988, Medicaid spending for home and com-
munity services has increased dramatically. In that
year, expenditures for all long-term care services
totaled $23 billion. Nearly 90 percent of those dol-
lars paid for institutional services in nursing facilities
and intermediate care facilities for persons with in-
tellectual disabilities (ICFs/ID). Only 10 percent was
spent on home and community services (i.e., HCBS
waivers, personal care, home health, and targeted
case management).
4
In 2008, total Medicaid spending for all long-term
care services had increased to $106.4 billion. Insti-
tutional spending had dropped to 57.3 percent and
HCBS spending increased to 42.7 percent. The latter
percentage, however, masks large variations among
states in the share of spending devoted to home
and community services and among dierent popu-
lations. For example, in 2008 only 10 states spent
50 percent or more of their long-term care budgets
on home and community services. New Mexico and
Oregon ranked at the top with over 70 percent; Mis-
sissippi was at the bottom with 13.9 percent.
5
Expansion of home and community services relative
to institutional services has been particularly pro-
nounced for individuals with intellectual disabilities
and other developmental disabilities (ID/DD, hereaf-
ter called developmental disabilities). In 2008, only
four states (New Mexico, Washington, Oregon, and
California) spent more than 50 percent of their Med-
icaid long-term care budgets on home and commu-
nity services for the aged and disabled population,
while 42 states spent at least half of their Medicaid
long-term care budgets on home and community
services for individuals with developmental disabili-
ties. As an example, Oregon’s spending on home
and community services for the ID/DD population
was 100 percent compared with 53.6 percent for the
aged and disabled population.
Nationally, in 2008, 35.5 percent of Medicaid’s total
long-term care expenditures for persons with devel-
opmental disabilities were allocated to institutional
services and 64.5 percent to home and community
services. The allocation for elderly persons and
younger persons with physical disabilities was the
opposite—68.4 percent of total long-term care
expenditures for institutional services and 31.6 per-
cent for home and community services.
6
23
Chapter 1: Medicaid Coverage of Home and Community Services: Overview
Major Features of Medicaid’s Provisions
for Home and Community Services
The remainder of this chapter presents a brief over-
view of the Medicaid law, regulations, and policies
that give states the exibility to create comprehen-
sive home and community service systems for peo-
ple of all ages with all types of physical and mental
impairments and/or chronic health conditions. To
provide context for the discussion, Table 1-1 lists
the major relevant provisions of Medicaid law. This
chronological summary illustrates the historical
expansion of Medicaid long-term care services away
from a primary focus on institutional care.
Key benets for providing home and community
services include both mandatory services such as
Home Health and optional services such as Personal
Care and Rehabilitation. Additional Medicaid provi-
sions, such as the HCBS waiver authority, enable
states to oer a comprehensive range of home and
community services.
Mandatory State Plan Services:
Home Health
Since 1970, services under the Home Health benet
have been mandatory for people entitled to nursing
facility care.
7
States are mandated to cover nursing
home care for categorically eligible persons age 21
or older. This mandate entitles persons age 21 or
older to nursing facility care. States have the op-
tion to cover nursing home care for other Medicaid
beneciaries as well, such as persons under age 21.
If a state chooses to cover persons under age 21,
they would also be entitled to nursing home care.
However, being entitled to nursing home care does
not mean that one is eligible for nursing home care.
In order to receive Medicaid-covered nursing home
care, entitled persons must also meet nursing home
eligibility criteria—called level-of-care criteria.
8
(See
Chapter 3 for additional information about eligibil-
ity for services under the Home Health benet.)
Federal regulations require that Home Health ser-
vices include nursing, home health aides, medical
supplies, medical equipment, and appliances suit-
able for use in the home. States have the option of
providing additional therapeutic services under the
Home Health benet—including physical therapy,
occupational therapy, and speech pathology and
audiology services.
9
States may establish reasonable
standards for determining the extent of such cover-
age using criteria based on medical necessity or
utilization control.
10
In doing so, a state must ensure
that the amount, duration, and scope of coverage
are reasonably sucient to achieve the purpose
of the service.
11
All Home Health services must be
medically necessary and authorized by a physician’s
order as part of a written plan of care.
In 1998, following the ruling of the U.S. Court of
Appeals for the Second Circuit in DeSario v. Thomas,
CMS sent a letter to State Medicaid Directors clarify-
ing that states may develop a list of pre-approved
items of medical equipment as an administrative
convenience but must provide a reasonable and
meaningful procedure for beneciaries to request
items that do not appear on such a list.
12
Home
Health services are dened in Federal regulation
as services provided at an individual’s place of
residence. In 1997, however, the Federal Court of
Appeals for the Second Circuit ruled in Skubel v.
Fuoroli that home health nursing services may be
provided outside the home, as long as they do not
exceed the hours of nursing care that would have
been provided in the home.
13
(See Chapter 3 for ad-
ditional information on this ruling.)
24 Understanding Medicaid Home and Community Services: A Primer
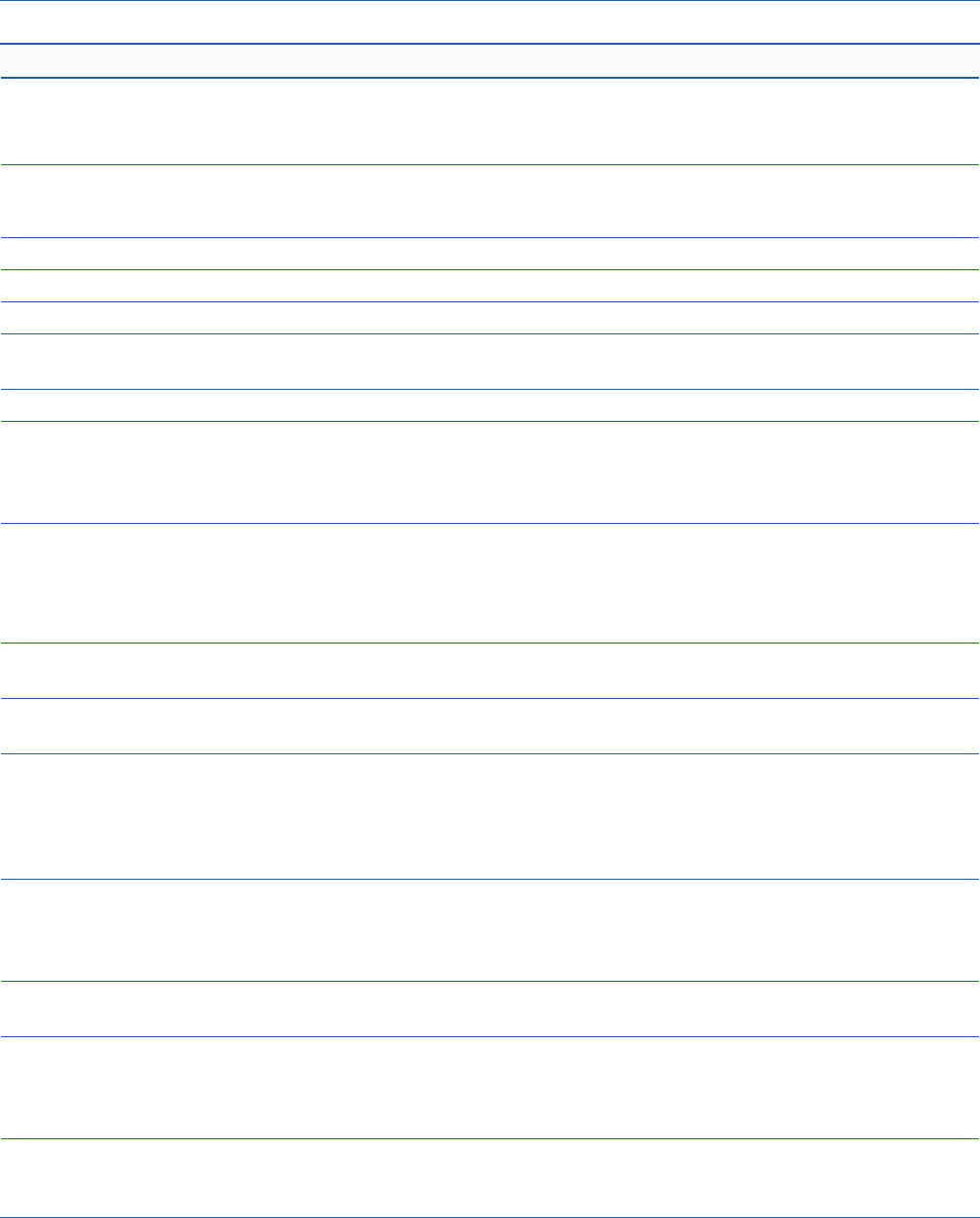
TABLE 1-1 Medicaid’s Legislative Provisions Regarding Long-Term Care Services
1965 Establishment of Medicaid
14
• Mandatory coverage of SNFs for categorically eligible persons age 21 or older.
• Optional coverage of Home Health services and Rehabilitation services.
1967 Early and Periodic Screening, Diagnosis, and Treatment (EPSDT) mandate for children under age 21.
15
States given the option to provide services not covered by their State Plans under EPSDT.
1970 Mandatory coverage of Home Health services for those entitled to SNF services.
1
6
1971 Optional coverage of intermediate care nursing facilities and ICFs/ID.
17
1972 Optional coverage of children under age 21 in psychiatric hospitals.
1
8
1973 Option to allow people receiving supplemental security income (SSI) to return to work and maintain
their Medicaid benets.
1
9
1981 Establishment of HCBS waiver authority.
2
0
1982 Option to allow states to extend Medicaid coverage to certain children with disabilities who live at home
but who, until this 1982 provision, were eligible for Medicaid only if they were in a hospital, nursing facil-
ity, or ICF/ID. Also known as the Katie Beckett or Tax Equity and Fiscal Responsibility Act (TEFRA) provi-
sion.
2
1
1986 Option to cover targeted case management (TCM). States are allowed to cover TCM services without
regard to statewideness and comparability requirements.
22
Option to oer supported employment services through HCBS waiver programs to individuals who had
been institutionalized some time prior to entering the HCBS waiver program.
23
1988 Establishment of special nancial eligibility rules for institutionalized persons whose spouse remains in
the community, to prevent spousal impoverishment.
2
4
1989 EPSDT mandate amended to require states to cover any service a child needs, even if it is not covered
under the State Plan.
25
1993/94 Removal of requirements for physician authorization and nurse supervision for personal care services
provided under the State Plan. States explicitly authorized to provide personal care services outside the
individual’s home.
26
Personal Care added to the statutory list of Medicaid services. (Personal Care was an
option since the mid-1970s, when it was established administratively under the Secretary of Health and
Human Services’ authority.)
1997 Removal, under the Balanced Budget Act of 1997, of the “prior institutionalization” test as a requirement
for receiving supported employment services through an HCBS waiver program. Addition of rst oppor-
tunity for states to create a Medicaid “buy-in” for people with disabilities. Establishment of the Program
of All Inclusive Care for the Elderly (PACE) as a State Plan option.
1999 Additional options under the Ticket to Work and Work Incentives Act for states to create a buy-in pro-
gram for people with disabilities and to remove employment barriers.
27
2005 Establishment of a new Medicaid State Plan authority for providing HCBS under §1915(i) of the Social
Security Act, under the Decit Reduction Act of 2005 (DRA-2005), eective 2007. The DRA-2005 also
expands options for Medicaid participants to direct their services under HCBS waivers and State Plan
Personal Care programs, through §1915(j) of the Social Security Act.
2010 Establishment, under the Aordable Care Act of 2010, of a new authority under §1915(k) of the Social
Security Act, eective October 2011. This authority allows states to provide “Community-based Atten-
dant Services and Supports” under the Community First Choice Option.

25
Chapter 1: Medicaid Coverage of Home and Community Services: Overview
Mandatory State Plan Services: EPSDT
The Federally mandated Early and Periodic Screen-
ing, Diagnosis, and Treatment (EPSDT) program for
children from birth until they turn age 21 entitles
Medicaid-eligible children to services found nec-
essary to diagnose, treat, or ameliorate a defect,
physical or mental illness, or a condition identied
by an EPSDT screen. The original 1967 legislation
gave states the option to cover treatment services
not covered under the Medicaid State Plan. In
1989, Congress strengthened the EPSDT mandate
by requiring states to cover all treatment services
dened under §1905(a), regardless of whether or
not those services are covered in their Medicaid
State Plan.
28
As a result, EPSDT programs now cover
the broadest possible array of Medicaid services,
including personal care and other services provided
in the home.
Optional State Plan Services:
Personal Care
Since the mid-1970s, states have had the option
to oer personal care services under the Medicaid
State Plan. This option was rst established adminis-
tratively under the Secretary’s authority to add cov-
erages over and above those spelled out in §1905
of the Social Security Act, if such services would
further the Social Security Act’s purposes. In 1993,
Congress took the formal step of adding personal
care to the list of services spelled out in the Medic-
aid statute.
29
(See Chapter 4 for more information
about the State Plan Personal Care benet.)
When the Personal Care benet option was created,
it had a decidedly medical orientation. The services
had to be prescribed by a physician, supervised by a
registered nurse, and delivered in accordance with
a service plan. Moreover, they could be provided
only in a person’s place of residence. Generally, the
personal care services a state oered were for assist-
ing individuals to perform activities of daily living
(ADLs)—bathing, dressing, eating, toileting, and
transferring (e.g., from a bed to a chair). Personal
care workers could provide other forms of assis-
tance (e.g., housekeeping and laundry) only on a
limited basis and only if they were incidental to the
delivery of personal care services.
Starting in the late 1980s, some states sought to
broaden the scope of personal care services and
provide them outside the individual’s home in order
to enable beneciaries to participate in community
activities. In 1993, when Congress formally incor-
porated personal care into Federal Medicaid law, it
gave states explicit authorization to provide per-
sonal care outside an individual’s home.
30
Congress
went even a step further in 1994, allowing states
to (1)use means other than nurse supervision to
oversee the provision of personal care services, and
(2)establish means other than physician prescrip-
tion for authorizing such services. In November
1997, CMS issued new regulations concerning
optional Medicaid State Plan personal care services
to reect these statutory changes.
31
In January 1999, CMS released a State Medicaid
Manual Transmittal that thoroughly revised and
updated guidelines concerning coverage of per-
sonal care services. (See the Resources section of
this chapter for web links to the Medicaid Manual.)
New Manual materials make clear that personal care
services may include assistance not only with ADLs
but also with instrumental activities of daily living
(IADLs), such as personal hygiene, light housework,
laundry, meal preparation, transportation, grocery
shopping, using the telephone, medication man-
agement, and money management. Additionally,
the guidelines claried that all relatives except
“legally responsible relatives” (i.e., spouses, and par-
ents of minor children) could be paid for providing
personal care services to beneciaries.
The Manual further claried that, for persons with
cognitive impairments, personal care may include
“cueing along with supervision to ensure the indi-
vidual performs the task properly.” It also explicitly
recognized that the provision of personal care ser-
vices may be directed by the people receiving them.
Direction by participants includes training and
supervising personal care attendants. The ability of
participants to direct their personal care services
has been a feature of many personal assistance
programs for many years (both under Medicaid and
in programs funded only with state dollars). For ex-
ample, participant direction was built into the Mas-
sachusetts Medicaid Personal Care program from its
inception. Taken together, these ground-breaking

26 Understanding Medicaid Home and Community Services: A Primer
changes in Federal policy can help pave the way
for a state to broaden coverage of these services. In
order to take advantage of these changes, a state
must amend its State Plan. Neither the statutory
provisions nor the revised Federal regulations and
State Medicaid Manual guidelines dictate that a
state must change the scope of its pre-1993 per-
sonal care coverage.
In 2005, 36 states covered personal care services
under their Medicaid State Plans.
32
The most likely
explanation for this less than national coverage is
that some states have elected to cover personal
care services through more exible and easy to
target HCBS waiver programs instead of adding the
benet to their State Plan. (See Chapter 4 for a dis-
cussion of the various options for covering personal
care, including their advantages and drawbacks.)
The §1915(j) Authority. The DRA-2005 added
§1915(j) to the Social Security Act, eective January
2007.
33
This authority permits a state to institute an
option for participants to have individual budgets
to purchase non-traditional goods and services
other than personal care to the extent that expendi-
tures would otherwise be made for human assis-
tance. It also allows states the option to disburse
cash prospectively to participants who direct their
services under the State Plan Personal Care benet
or an HCBS waiver program. Participants may also
determine rates of pay for their workers, accumulate
funds earmarked for the purchase of a specic item
designed to increase independence or substitute for
human assistance, and work with a scal intermedi-
ary to perform payroll and tax functions—called the
“budget authority.” Absent the §1915(j) authority,
participant direction of Medicaid State Plan per-
sonal care services is limited to hiring, supervising,
and dismissing (if needed) their workers—called the
“employer authority.”
States may use the §1915(j) authority only in pro-
grams already oered under its Medicaid State Plan
or an HCBS waiver (i.e., states may not oer the spe-
cic participant-directed services options under the
§1915(j) authority except in an existing State Plan
Personal Care program or HCBS waiver program).
(See Chapter 7 for a detailed description of this new
authority and a discussion of participant-directed
service options—also called self- or consumer-di-
rected—that can be oered under several Medicaid
authorities.)
Optional State Plan Services:
Targeted Case Management
Until 1986, the only practical avenue available for a
state to secure Medicaid funding for free standing
case management services (i.e., case management
services not delivered as part of some other service
or conducted in conjunction with the state’s opera-
tion of its Medicaid program) was through an HCBS
waiver program. Coverage of case management ser-
vices in HCBS waiver programs was nearly universal
at that time.
In 1986, Congress created an option for states to
cover what were termed “targeted case manage-
ment” services under their State Plan.
34
The ex-
pressed statutory purpose of targeted case man-
agement is to assist Medicaid recipients in “gaining
access to needed medical, social, educational, and
other services.” This optional benet is exempt from
the comparability requirement to make services
available to all recipients. A state is permitted to
amend its State Plan to cover case management
services for one or more specied groups of Medic-
aid recipients (hence the term targeted). It may also
oer these services on a less-than-statewide basis
(through a State Plan amendment instead of secur-
ing a waiver).
35
Given the expressed statutory purpose of the ben-
et—to assist individuals to obtain services from a
wide variety of public and private programs—the
scope of services a state may furnish through the
targeted case management option is relatively
broad. In addition to assessment and service/
support planning, referrals, and monitoring the
delivery of services and supports to ensure they are
meeting a beneciary’s needs, covered activities
include assistance in obtaining food stamps, emer-
gency housing, or legal services. (See Chapter 4 for
more information about this benet.)

27
Chapter 1: Medicaid Coverage of Home and Community Services: Overview
Optional State Plan Home and
Community-Based Services
36
The DRA-2005 added §1915(i) to the Social Security
Act, which was amended by the Patient Responsibil-
ity and Aordable Care Act of 2010. The §1915(i) au-
thority gives states the option to oer a wide range
of home and community-based services without
having to secure Federal approval of a waiver. The
§1915(i) authority provides states an opportunity to
oer services and supports before individuals need
institutional care, and also provides a mechanism to
provide State Plan HCBS to individuals with mental
health and substance use disorders.
Unlike other State Plan services, under §1915(i),
states may design service packages without regard
to comparability.
37
States may oer HCBS to specic,
targeted populations and oer servi ces that dier in
amount, duration, and scope to specic population
groups, including eligibility groups as authorized
under §1915(i)(6)(c), either through one or multiple
§1915(i) service packages. Services must be avail-
able statewide.
Optional State Plan Services:
Community Choice Option
38
The Aordable Care Act added §1915(k) to the
Social Security Act, eective October 2011, which
allows states to provide “Community-based At-
tendant Services and Supports”—called the Com-
munity First Choice Option. Under §1915(k), states
that provide home and commu nity-based atten-
dant services and supports through their State
Plans under this option will receive a six percentage
points higher Federal match. Individuals must be
eligible for Medicaid under the State Plan and have
an income that does not exceed 150 percent of the
Federal Poverty Level, or, if their income is greater,
they must meet institutional level-of-care criteria.
CMS plans to issue a Notice of Proposed Rule Mak-
ing related to this provision of the Aordable Care
Act in early 2011.
Other Optional State
Plan Home and Community Services
When Medicaid was enacted, states were given the
option of covering a wide range of services, several
of which can be provided in home and/or commu-
nity settings. They include rehabilitation services,
private duty nursing, physical and occupational
therapy, and transportation services. In 2000, every
state provided at least one optional service.
The Rehabilitation option, in particular, oers states
the means to provide a range of supportive services
to people in home and community settings. Med-
icaid denes rehabilitation services as any medical
or remedial services recommended by a physician
or other licensed practitioner of the healing arts for
maximum reduction of physical or mental disabil-
ity, and restoration of a recipient to his or her best
possible functional level.
39
Rehabilitation services
can be provided to people with either physical or
mental disabilities.
The Rehabilitation option is a very exible benet,
because services may be furnished either in the
person’s residence or elsewhere in the commu-
nity. Many states cover psychosocial rehabilitation
services, which—when combined with personal
care and targeted case management servi ces—can
meet a wide range of service and support needs for
persons who have a serious mental illness. In 2005,
46 states used the Rehabilitation option to provide
services for persons with a serious mental illness;
33 states used the Rehabilitation option to provide
other services.
40
28 Understanding Medicaid Home and Community Services: A Primer
Optional Institutional Services
The 1971 addition of the option to cover ser-
vices provided by intermediate care nursing
facilities, called intermediate care facilities (ICFs),
and ICFs/ID, moved the Medicaid program into
nancing additional nursing home care and
institutional services for the ID/DD population.
States adding optional institutional coverage of
ICFs/ID could receive Federal matching funds to
help nance services for persons with develop-
mental disabilities, which had previously been
supportable only with state funds.
Likewise, states adding optional coverage of
ICFs could receive Federal matching funds to
help nance a non-skilled level of nursing care
(which had previously been supportable only
with state funds). Over the next few years, every
state and the District of Columbia chose to cover
ICFs and ICFs/ID in their State Plan.
The option to cover nursing ICFs and ICF/IDs as-
sumed greater importance after 1981, when the
waiver authority was created. This was because
§1915(c) waiver services can be provided only
insofar as they provide an alternative to institu-
tional care.
41
(In 1987, Congress abolished the
distinction between SNFs and ICFs. Nursing fa-
cilities were mandated to provide both a skilled
and intermediate level of care.)
The Rehabilitation option is not generally used
to furnish long-term care to individuals with dis-
abilities or chronic health conditions other than
mental illness. During the 1970s and 1980s, a few
states secured approval to cover daytime services
for persons with developmental disabilities under
either the Clinic or the Rehabilitation option. How-
ever, CMS ultimately ruled that the services being
furnished were habilitative rather than rehabilita-
tive and consequently could not be covered under
either option by additional states. The main basis for
the ruling was that habilitative services could only
be furnished to residents of ICFs/ID under the Med-
icaid State Plan or through an HCBS waiver program
for individuals otherwise eligible for ICF/ID services.
States with existing programs serving individuals
with intellectual disabilities and other develop-
mental disabilities were grandfathered under the
Omnibus Reconciliation Act (OBRA) of 1989.
A few states have maintained their State Plan cover-
age of these services; others have terminated them
in favor of oering similar services through an HCBS
waiver program.
42
With the creation of the new
HCBS State Plan option under the §1915(i) author-
ity, states may now cover habilitation as a home and
community-based service under the State Plan.
The HCBS Waiver Authority
In 1981, Congress authorized the waiver of certain
Federal requirements to enable states to provide
home and community services (but not room and
board) to individuals who would otherwise require
institutional services reimbursable by Medicaid (i.e.,
services in a skilled nursing facility, an intermedi-
ate care nursing facility, or an ICF/ID). The waiver
programs are often called §1915(c) waivers (named
after the section of the Social Security Act that
authorized them), but are also called HCBS waivers,
the term used in this Primer.
43
Under the §1915(c) waiver authority, states can
provide services not usually covered by the
Medicaid program, as long as these services are
required to prevent institutionalization. Services
covered under waiver programs include case man-
agement, homemaker, home health aide, personal
care, adult day health, habilitation, respite care, and
“such other services requested by the state as the
Secretary of Health and Human Services (HHS) may
approve.” Services for individuals with a chronic
mental illness were added in the late 1980s: “day
treatment or other partial hospitalization services,
psychosocial rehabilitation services, and clinic ser-
vices (whether or not furnished in a facility).”
Neither the statute itself nor CMS regulations
further specify or dene the scope of the listed
services. However, the law that created the waiver
program expressly permits the Secretary of HHS to
approve services beyond those specically spelled
out in the law, as long as they are necessary to avoid
institutionalization and are cost-eective. In the
29 years since the waiver author ity became avail-
able, CMS has approved a wide range of additional
services.

29
Chapter 1: Medicaid Coverage of Home and Community Services: Overview
In the early 1990s, CMS rst issued a standard HCBS
waiver application format for states to submit
requests to operate an HCBS waiver program. The
standard format included denitions of services
states commonly cover in their HCBS waiver pro-
grams. The services listed in the standard format ap-
pear there because they are included in the listing
contained in the statute, or are additional services
that states frequently oer.
In 2005, CMS extensively modied its standard
§1915(c) application to obtain greater detail about
how the proposed program would operate. States
must now provide specic information about how
their programs comply with Federal standards, as
well as detailed information about their quality im-
provement systems. Beginning in 2006, CMS began
oering a web-based version of the application. The
conversion to a web-based application streamlines
the preparation of waiver applications and amend-
ments, and improves communication between
states and CMS about waiver requests.
The Waiver Application Instructions represent the
most current guidance related to HCBS waivers. The
instructions provide CMS-suggested denitions
of services that states may cover under their HCBS
waiver programs—identied as Core Service Deni-
tions. The services a state may oer are by no means
limited to those that appear in the standard format,
nor are the proposed denitions required. (See the
Resources section of this chapter for a link to all ap-
proved HCBS waivers and a link to the online waiver
application and technical guidance document.)
During Federal scal year (FFY) 2008, 48 states and
the District of Columbia operated 314 HCBS waiver
programs. This number includes waivers that CMS
had approved but that had not yet been imple-
mented as of September 30, 2008. The two states
that did not have HCBS waivers—Arizona and Ver-
mont—provided similar services as part of Research
and Demonstration waivers authorized by §1115 of
the Social Security Act.
44
Expenditures for waiver services totaled $30 bil-
lion in 2008 and roughly three-fourths was used to
purchase services and supports for persons with
developmental disabilities, including persons with
autism spectrum disorders or intellectual disabili-
ties.
45
Almost all other waiver expenditures in the
same year were for older adults and younger adults
with physical disabilities; a few smaller population
groups accounted for the remaining waiver expen-
ditures.
46
The Katie Beckett Provision
The Katie Beckett provision is in a statute—the
Tax Equity and Fiscal Responsibility Act 134—and
was added to Medicaid in 1982. Katie Beckett is
the name of the child whose parents petitioned
the Federal Government for her to receive Medic-
aid services at home instead of in a hospi tal, and
whose plight led the Reagan Administration to urge
Congress to enact the provision. Prior to enactment,
if a child with disabilities lived at home, the parents’
income and resources were automatically counted
(deemed) as available for medical expenses. How-
ever, if the same child was institutionalized for 30
days or more, only the child’s own income and re-
sources were count ed in the deeming calculation—
substantially increasing the likelihood that a child
could qualify for Medicaid. This sharp divergence in
methods of counting income often forced families
to institutionalize their children simply to obtain
medical care for them.
TEFRA 134 amended the Medicaid statute to give
states the option to waive the deeming (i.e., count-
ing) of parental income and resources for children
under 18 years old who were living at home but
would otherwise be eligible for Medi caid-funded
institutional care. Not counting parental income en-
ables these children to receive Medicaid services at
home or in other community settings. Many states
use this option, which requires them to determine
that (1)the child needs the level of care provided
in an institution, (2)it is appropriate to provide care
outside a facility, and (3)the cost of care at home is
no more than the cost of institutional care. In states
that use this option, parents may choose either
institutional or community care for their Medicaid-
eligible children.

30 Understanding Medicaid Home and Community Services: A Primer
The Program of All-Inclusive Care
for the Elderly (PACE)
The Program of All-Inclusive Care for the Elderly—
authorized by the Balanced Budget Act of 1997
(BBA-97)—is a capitated program that features a
comprehensive service delivery system that in-
tegrates Medicare and Medicaid nancing. The
BBA-97 established the PACE model of care as a
permanent method for organizing service delivery
within the Medicare program, and enables states
to provide PACE services to Medicaid beneciaries.
Participants must be at least 55 years old, eligible
for Medicare or Medicaid or both, and certied as
meeting a state’s nursing home level-of-care criteria.
For most participants, the comprehensive service
package permits them to continue living at home
rather than be admitted to an institution.
In 2009, 72 PACE programs were operating in 30
states. The State Plan must include PACE as a Med-
icaid benet before the state and the Secretary of
HHS can enter into program agreements with PACE
providers. Participants must be at least 55 years old,
live in the PACE service area, and be certied as eli-
gible for nursing home care by the appropriate state
agency. The PACE program becomes the sole source
of services for persons dually eligible for Medicare
and Medicaid who choose to enroll.
An interdisciplinary team, consisting of professional
and paraprofessional sta, assesses participants’
needs, develops service plans, and delivers all
services (including primary and acute health care
services, home and community services, and when
necessary, nursing facility services). Financing for
these services is integrated to promote a seamless
system of care. PACE programs provide social and
medical services primarily in an adult day health
center, supplemented by in-home and other ser-
vices in accordance with participants’ needs. The
PACE service package must include all Medicare
and Medicaid covered services, and other services
determined necessary by the interdisciplinary team
for the care of the PACE participant. (See Chapter 8
for more information about the PACE program and
other Medicaid managed care options.)
This brief overview of Medicaid’s statutory, regula-
tory, and other policy provisions related to home
and community services provides a context for
more detailed discussions in the chapters to come.
Some of the institutional bias that remains in the
program can be changed only by Congressional
amendment of Medicaid law (e.g., changing home
and community-based services from an optional to
a mandatory benet). But numerous provisions give
state policymakers considerable freedom in design-
ing their home and community service system to t
their state’s particular needs. They have the option,
in particular, to eliminate use of more restrictive
nancial criteria for waiver services than for institu-
tional care. They also have considerable exibility to
create consumer-responsive systems that facilitate
home and community living.
In the next several decades, as already noted, the
U.S. population will age dramatically. Even if dis-
ability rates among older persons decline, more
people will need long-term care services than at any
other time in our nation’s history. Institutional care
is costly. Given the projected demand for long-term
care, it is advisable for states to continue working
to create comprehensive long-term care service
systems that will enable people with disabilities
and/or chronic health conditions—whatever their
age or the severity of their condition—to live in
their homes and community settings rather than in
institutions.
The Medicaid program can be the centerpiece of
such a system—allowing states numerous options
to provide home and community services that
keep costs under control at the same time that they
enable people of all ages with disabilities and/or
chronic health conditions to retain their indepen-
dence and dignity.
31
Chapter 1: Medicaid Coverage of Home and Community Services: Overview
Resources
Since the Primer was rst published in 2000, numerous reports and other resources have become available
on the Internet. This section includes key publications and Internet resources regarding Medicaid long-
term care generally and home and community services specically. Most of the publications cite addition-
al resources, and the websites also have links to other sources of information.
Publications
Houser, A., Fox-Grage, W., and Gibson, M. (2009). Across the States 2009:
Proles of Long-Term Care and Independent Living. Washington, DC: AARP Public Policy Institute.
This report is the eighth edition of the AARP Public Policy Institute’s state long-term care reference report.
Published approximately every 2 years, the Across the States series was developed to help inform policy dis-
cussions among public and private sector leaders in long-term care throughout the United States. Across the
States 2009 presents comparable state-level and national data for more than 140 indicators, drawn together
from a wide variety of sources into a single convenient reference. This publication presents the most up-to-
date data available at the time of production, and is displayed in easy-to-use maps, graphics, tables, and state
proles.
Available at http://www.hcbs.org/moreInfo.php/doc/2536
Centers for Medicare & Medicaid Services. (2008). Application for a §1915(c) Home and Community-Based
Waiver [Version 3.5]: Instructions, Technical Guide and Review Criteria. Baltimore, MD: USDHHS.
This publication contains extensive information concerning Federal policies that apply to the operation of an
HCBS waiver as well as technical guidance for completing the application.
Available at https://www.hcbswaivers.net/CMS/faces/portal.jsp under links and downloads, entitled §1915(c)
Waiver Application and Accompanying Materials.
CMS State Medicaid Director Letter (November 19, 2009). Implementation of §6087 of the Decit Reduction
Act of 2005 Regarding §1915(j) of the Social Security Act.
This letter provides guidance on the implementation of §6087 of the Decit Reduction Act of 2005, Public
Law Number 109-171. Section 6087, the “Optional Choice of Self-Directed Personal Assistance Services (Cash
32 Understanding Medicaid Home and Community Services: A Primer
and Counseling),” amended §1915 of the Social Security Act by adding a new subsection (j). The guidance also
applies to §1915(c) HCBS waiver programs when states oer a self-direction option and permit participants to
purchase “individual directed goods and services.” The letter oers information on (1)Background, (2)Medic-
aid Authorities, (3)Criteria, (4)Support and Monitoring, and (5)Compliance with the Guidance.
Available at http://www.cms.hhs.gov/SMDL/SMD/ItemDetail.asp?ItemID=CMS1230894
The Kaiser Commission on Medicaid and the Uninsured. (2009). Medicaid Home and Community-Based Ser-
vice Programs: Data Update. Washington, DC: Kaiser Family Foundation.
This report presents a summary of the main trends to emerge from an analysis of the 2006 expenditures and
participant data for the three main Medicaid home and community service programs: optional §1915(c) HCBS
waivers, the mandatory Home Health benet, and the optional State Plan Personal Care benet. It also pres-
ents survey ndings about various features of the three programs, such as eligibility criteria, waiting lists, and
provider reimbursement rates for the Home Health benet and the Personal Care benet.
Available at http://www.k.org/medicaid/7720.cfm
National Association of State Medicaid Directors. (2007). State Perspectives on Emerging Medicaid Long-
Term Care Policies and Practices. Washington, DC: American Public Human Services Association.
The purpose of this survey analysis is to provide states with an overview of state implementation of the DRA-
2005 options and other long-term care policies and practices. Findings address a range of issues, including
eligibility, Children with Disabilities, Money Follows the Person, HCBS State Plan Amendments, Transition from
Institutions, Managed Care, State Plan Amendment for Personal Care Services, Cash & Counseling, Care Coordi-
nation, Disease Management, and Long-Term Care Reform.
Available at http://www.hcbs.org/moreInfo.php/doc/2094
33
Chapter 1: Medicaid Coverage of Home and Community Services: Overview
Websites
The following websites provide information about Medicaid, long-term care services and supports, or home
and community services. This list is not inclusive of all the resources available on the Internet, but provides a
good starting point for nding information.
Federal Government
Centers for Medicare & Medicaid
General: Links to Programs and Information
Web address: http://www.cms.hhs.gov/default.asp
Specic: Links to Regulations and Guidance
1. Program transmittals are used to communicate new or changed policies and/or procedures that are
being incorporated into a specic CMS program manual. The cover page (or transmittal page) summa-
rizes the new changed material, specifying what is changed.
Available at http://www.cms.hhs.gov/Transmittals/
2. The CMS Online Manual System is used by CMS programs, partners, contractors, and State Survey
Agencies to administer CMS programs. It oers day-to-day operating instructions, policies, procedures
based on statutes and regulations, guidelines, models, and directives. In 2003, CMS transformed the
CMS Program Manuals into a web user-friendly presentation and renamed it the CMS Online Manual
System.
Available at http://www.cms.hhs.gov/Manuals/01_Overview.asp
3. Paper-based manuals are CMS manuals that were ocially released in hardcopy. The majority of these
manuals were transferred into the Internet-only manual or retired from the manual. The State Medic-
aid Manual is still an active paper-based manual.
Available at http://www.cms.hhs.gov/Manuals/PBM/itemdetail.asp?lterType=none<er
ByDID=-99&sortByDID=1&sortOrder=ascending&itemID=CMS021927&intNumPerPage=10
4. The State Medicaid Director and State Health Ocial letters are used to provide states with guidance
and clarication on current information pertaining to Medicaid policy, Medicaid data issues, and State
Children’s Health Insurance Program policy. The intent of these letters is not to establish policy, but to
ensure consistency and better serve the states.
Available at http://www.cms.hhs.gov/SMDL/
5. CMS maintains a database of every state’s approved waiver applications under various authorities, for
example, §1915(c), §1915(b), and §1115. Users can access fact sheets, copies of proposals, approval
letters, and other documents related to specic programs.
Available at http://www.cms.hhs.gov/MedicaidStWaivProgDemoPGI/%2008_WavMap.asp
34 Understanding Medicaid Home and Community Services: A Primer
Administration on Aging, Home & Community Based Long-Term Care
Web address: http://www.aoa.gov/AoARoot/AoA_Programs/HCLTC/index.aspx
Oce of the Assistant Secretary for Planning & Evaluation,
Oce of Disability, Aging, and Long-Term Care Policy
Web address: http://aspe.hhs.gov/_/oce_specic/daltcp.cfm
State Associations, Other Associations, and Foundations
American Public Human Services Association
Web address: http://www.aphsa.org/Home/home_news.asp
Kaiser Family Foundation
Web address: http://www.k.org
National Academy for State Health Policy
Web address: http://www.nashp.org/
National Association of State Medicaid Directors
Web address: http://www.nasmd.org/Home/home_news.asp
National Association of State Mental Health Directors
Web address: http://www.nasmhpd.org/
National Association of State Directors of Developmental Disabilities Services
Web address: http://www.nasddds.org/index.shtml
National Conference of State Legislatures
Web address: http://www.ncsl.org/default.aspx?tabid=14489
Robert Wood Johnson Foundation
Web address: http://www.rwjf.org/
State and Local Governments on the Web
Web address: http://www.statelocalgov.net/
The Clearinghouse for Home and Community Based Services promotes the development and expansion of
home and community services by gathering resources and tools for research, policymaking, and program de-
velopment into this one-stop website. The site has over 2,000 resources that users can browse using the site’s
search engine.
Web address: http://www.hcbs.org
35
Chapter 1: Medicaid Coverage of Home and Community Services: Overview
Endnotes: Citations, Additional Information,
and Web Addresses
1
Gary Smith and Janet O’Keee co-authored the original chapter. Janet O’Keee updated the chapter. In
addition to the sources noted in the citations, a major source of historical information for this chapter is the
Medicaid Source Book: Background Data and Analysis (1993). Washington, DC: U.S. Government Printing Of-
ce.
2
Overall, the Federal Government nances an average of 57 percent of all Medicaid costs annually. National
Health Policy Forum. (January 2009). The Basics, FMAP: The Federal Share of Medicaid Costs. Available at
http://www.nhpf.org/library/the-basics/Basics_FMAP_01-15-09.pdf.
3
The Olmstead Supreme Court decision increased state responsibility to provide a range of home and com-
munity service options. The Court ruled that states must provide services in the most integrated setting
appropriate to the needs and wishes of people with disabilities. Failure to do so could constitute discrimina-
tion under the Americans with Disabilities Act. Information about the application of the Olmstead decision
to the Medicaid program is available from the CMS website in State Medicaid Director Letters. Use the word
Olmstead to nd the relevant letters. Available at http://www.cms.hhs.gov/SMDL/SMD/list.asp#TopOfPage.
4
Burwell, B. (2000). Memorandum: Medicaid Long-Term Care Expenditures in FY 1999. Cambridge, MA: The
MEDSTAT Group.
5
Burwell, B., Sredl, K., and Eiken, S. (2009). Medicaid Long-Term Care Expenditures in FY 2008. Cambridge, MA:
Thomson Reuters. Available at http://www.hcbs.org/moreInfo.php/doc/2793.
6
Eiken, S., and Burwell, B. (2009). Medicaid HCBS Waiver Expenditures: FY 2003 through FY2008. Cambridge,
MA: Thomson Reuters. Available at http://www.hcbs.org/moreInfo.php/doc/2795.
7
Section 1902(a)(10)(d) of the Social Security Act. If a state chooses to cover nursing facility care for the medi-
cally needy, Home Health services become mandatory for this group as well.
8
The coverage criterion for Home Health services is often misunderstood because it is linked to the coverage
criterion for nursing homes. The confusion has arisen because the term entitled to nursing facility care has
sometimes been erroneously interpreted to mean that people must be eligible for nursing facility care—that
is, they must meet a state’s nursing facility level-of-care criteria in order to receive the Home Health benet.
This erroneous interpretation has persisted, notwithstanding its conict with Federal Home Health regula-
tions prohibiting a state from conditioning eligibility for Home Health services on the need for or discharge
from institutional care (42CFR 441.15(c)).
9
42 CFR 440.70(b).
10
42 CFR 440.230(d).
11
42 CFR 440.230(b)
12
Health Care Financing Administration. (September 4, 1998). Letter to State Medicaid Directors. Available at
http://www.cms.hhs.gov/smdl/downloads/SMD090498.pdf.
13
Skubel v. Fuoroli. (No. 96-6201). United States Court of Appeals, Second Circuit. Decided May 13, 1997.

36 Understanding Medicaid Home and Community Services: A Primer
14
Social Security Amendments of 1965 (P.L. 89-97).
15
Social Security Amendments of 1967 (P.L. 90-248).
16
P.L. 90-248, eective July 1970.
17
Act of December 14, 1971 (P.L. 92-223).
18
Social Security Amendments of 1972 (P.L. 92-603). This institutional coverage provides the “institutional alter-
native” for waiver services for this group.
19
Section 1619 P.L. 96-265 of the Social Security Act.
20
Omnibus Budget Reconciliation Act of 1981 (OBRA 81, P.L. 97-35).
21
P.L. 103-66. Section 13601 (a1/5)8. Section 134 of TEFRA contains the amendment.
22
Consolidated Omnibus Reconciliation Act of 1985 (P.L. 99-272). The provision became eective April 1986.
23
Ibid.
24
Medicare Catastrophic Coverage Act of 1988 (P.L. 100-360).
25
Omnibus Reconciliation Act of 1989.
26
Omnibus Reconciliation Act of 1993. Section 13601 (a1/5)8 (P.L. 103-66). The changes took eect on Octo-
ber 1, 1994. In November 1997, CMS issued new regulations (42 CFR 440.167) concerning optional Medicaid
State Plan personal care services to reect these statutory changes.
27
P.L. 106-170.
28
Omnibus Reconciliation Act of 1989.
29
The Omnibus Budget Reconciliation Act of 1993 (§13601(a)(5)); Social Security Act (§1905(a)(24)).
30
Individuals who reside in institutions—nursing facilities, ICFs/ID, hospitals, and institutions for mental dis-
ease—cannot receive personal care services through the Personal Care benet.
31
42 CFR 440.167.
Chapter 2: Financial Eligibility Rules and Options
37
Guide to Chapter 2
Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 39
Overview of Medicaid Financial Eligibility . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 39
Medicaid for SSI Beneciaries . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 41
General Rule . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 42
Exceptions to the General Rule . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 43
State 209(b) Option . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 43
Medicaid Exceptions to SSI Countable Income and Resources Rules . . . . . . . . . . . . . . . . . . . . . . 44
Eligibility Expansion Options Including, but Not Specic to,
Home and Community Services . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 44
100 Percent of Poverty Option . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 45
Medically Needy Option . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 45
Eligibility Expansion Options That Can Be Targeted to
Persons Needing Home and Community Services . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 46
State Supplemental Payments (SSPs) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 46
300 Percent of SSI Income Option . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 47
Preventing Spousal Impoverishment . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 50
Income Protection . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 50
Resource Protection . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 51
Provisions Specic to Children with Disabilities. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 51
Zebley Kids . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 52
Katie Beckett Option . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 52
Reducing Financial Barriers to Employment for Persons with Disabilities . . . . . . . . . . . . . . . . . 53
Federal Provisions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 53
State Options . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 53
Asset/Resource Transfers: Permissions and Penalties. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 54
Structure of the Penalty . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .54
Permissible Transfers . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 54
Estate Recoveries . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 56
Disqualication for Long-Term Care Medicaid Coverage for Individuals with Substantial
Home Equity . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 56
Resources. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .57
Endnotes: Citations, Additional Information, and Web Addresses . . . . . . . . . . . . . . . . . . . . . . . . 60
39
Chapter 2: Financial Eligibility Rules and Options
Chapter 2
Financial Eligibility Rules and Options
This chapter describes Federal requirements and state options regarding nancial eligibility for Medicaid,
with a focus on eligibility for long-term care services and supports.
1
Introduction
As originally conceived, the Medicaid program was to have served primarily the very poor and near poor who
qualied or were close to qualifying for cash welfare programs. It was to have functioned much like private
health insurance, with service coverage focused on primary and acute health care needs. Over time, Federal
and state actions have expanded Medicaid’s authority, the scope of its coverage of long-term care services,
and its eligibility options for beneciaries who do not meet the traditional welfare-based denition of “poor.”
By the end of its rst decade, Medicaid had become a major source of public funding for institutional long-
term care. By the end of its third decade, it had become the major public funder of home and community
long-term care services as well.
Medicaid’s role in nancing long-term care has developed in sporadic increments—often in reaction to prob-
lems occupying center stage at a particular time. As a result of incremental policymaking combined with vast
variations in how states cover long-term care, the various facets of Medicaid’s nancial eligibility provisions
may appear to be disjointed. In particular, there are many provisions with major eligibility discontinuities—
wherein a slight change in individuals’ personal circumstances can result in huge dierences in the kinds (and
levels) of benets they are eligible for. As a result, individuals in similar circumstances can be treated dier-
ently. The purpose of this chapter is to present the relevant provisions in a way that is most useful to state
policymakers and advocates.
Overview of Medicaid Financial Eligibility
Medicaid nancial eligibility provisions are deeply rooted in two Federally nanced cash assistance programs
to help support low-income individuals and families: the former Aid to Families with Dependent Children
(AFDC) program, which provided income support for low-income families with children, and the Supplemental
Security Income (SSI) program for the “Aged, Blind, and Disabled.”
2
(In 1996, welfare reform legislation replaced
AFDC with a new program, Temporary Assistance for Needy Families [TANF].)
Like AFDC/TANF and SSI, Medicaid is a means-tested entitlement program. That is, anyone qualies for Med-
icaid if (a)their income and assets do not exceed the state thresholds specic to their eligibility group, and
(b)they meet all other relevant eligibility criteria. Medicaid eligibility rules fall into two basic sets: categorical
and nancial. The categorical set denes particular categories of persons for whom Federal law permits cover-
age. Individuals needing long-term care services generally fall into one of three Medicaid categories: aged 65
or older, blind, or under age 65 with a disability.
40 Understanding Medicaid Home and Community Services: A Primer
Services for Medicaid-Eligible Persons
The highlights of Medicaid benets listed here provide a general context for the nancial eligibility discussion in
this chapter. (For a more detailed discussion, see Chapter 4 and Chapter 5.)
• Once determined eligible for Medicaid, beneciaries are entitled to the full range of health and long-term
care Medicaid services covered in their state. To receive long-term care services, however, they must also
meet service eligibility criteria.
• Medicaid health care coverage (e.g., hospital, physician, or prescription drug services) can be extremely
important to persons who need long-term care services, especially if they do not have Medicare or private
health insurance to cover these expenses.
• Medicaid services for children can be more extensive than Medicaid services for adults or than services typi-
cally covered under private insurance policies.
• Medicare and Medicaid cover many of the same health services (e.g., hospital, physician, and home health
services). Medicare beneciaries eligible under any of their state-dened Medicaid eligibility groups typically
receive Medicaid coverage of Medicare cost-sharing requirements, including premiums, deductibles, and
coinsurance. They also receive Medicaid services covered by Medicaid but not Medicare. The most notable
examples are more extensive coverage of mental health services, long-term care institutional services, and
personal care services, as well as home health services with a less intense medical orientation than services
covered under the Medicare Home Health benet.
3
• Nursing facility services are Federally mandated under Medicaid. States may provide other long-term care
services at their option, which may be provided either to all eligibles under the Medicaid State Plan or to se-
lected groups under a home and community-based services (HCBS) waiver. Under an HCBS waiver program,
states can provide services not viewed as strictly medical (e.g., home modications, habilitation, and respite
care) if the services are required to prevent institutionalization.
Medicaid criteria for determining who is blind or has a disability are generally the same as those used by the
Social Security Administration for SSI. To qualify in a disability category, a person must have a long-lasting,
severe, medically determinable physical or mental impairment. The person must also be unable to work—de-
ned in 2010 in part as earning less than $1,000 per month (net of income-related work expenses), a level of
earning considered by regulation as evidence of one’s ability to engage in Substantial Gainful Activity (SGA).
4
Anyone not meeting these criteria cannot receive Medicaid through the disability eligibility category, even if
they have extensive medical needs or high medical bills. (Special exceptions—allowing Medicaid eligibility for
certain former child beneciaries of SSI disability benets and for persons who do not meet one or more of the
usual SSI disability criteria because they earn more than $1,000 per month—are discussed later in this chap-
ter.)
Although Medicaid’s nancial eligibility rules for people who are elderly or have disabilities are built on a
foundation of SSI rules, many exceptions and variations enacted over the years make them work better for
low-income persons who need health care but not cash assistance.
41
Chapter 2: Financial Eligibility Rules and Options
Medicaid for SSI Beneciaries
SSI is the Federally-administered program that ensures a nationally uniform income oor for persons who are
elderly, blind, or have other disabilities. To be eligible, both income and assets must be low. Thirty-nine states
and the District of Columbia provide Medicaid to all individuals in any month in which they receive an SSI
payment. Of these, 33 do so automatically, based on a list of SSI beneciaries compiled by the Federal Social
Security Administration. The other 7 require SSI beneciaries to le a separate application with the state for
Medicaid benets. The remaining 11 states follow what is known as the 209(b) exception option that allows
them to provide Medicaid to SSI beneciaries only if they meet the state’s eligibility criteria, which may be
more restrictive than those for SSI. (The 209(b) option is discussed in more detail below.
New Eligibility Group Established by the Aordable Care Act of 2010
5
Section (§)2001 of the Patient Protection and Aordable Care Act of 2010 (hereafter, Aordable Care Act) amend-
ed the Medicaid statute to create a new eligibility group that all states participating in Medicaid must cover as of
January 2014. For the rst time since the Medicaid program was established, states will receive Federal Medicaid
payments to provide coverage for the lowest income adults in their states, without regard to disability, parental
status, or most other categorical limitations, under their Medicaid State Plans.
For this new eligibility group, the Aordable Care Act raises the income eligibility threshold to 133 percent of
the poverty line and eliminates the assets test. All rules applicable under the Medicaid program in general apply
to this new eligibility group, including rules relating to cost sharing. States can phase in eligibility by income
level, but if they do, they must cover individuals with lower incomes before covering those with higher incomes.
Parents of children who could be covered under Medicaid but are not cannot be covered under this new group
unless their children are also enrolled in Medicaid.
The new group lls in the gaps in existing Medicaid eligibility coverage by making eligible very low-income
individuals who are not otherwise eligible under mandatory eligibility categories. Thus, the law describes the
individuals eligible under the new group as those who are not
• Age 65 or older,
• Pregnant,
• Entitled to or enrolled in benets under Medicare Part A,
• Enrolled under Medicare Part B,
• Receiving SSI benets, or
• Described in any of the other mandatory groups in the statute.
6
The medical assistance provided to an individual in the new eligibility group must consist of benchmark cov-
erage described in §1937(b)(1) of the Aordable Care Act or benchmark-equivalent coverage described in
§1937(b)(2)
7
unless the individual is exempt from mandatory enrollment in a benchmark benet plan.
8
Certain states—depending on their income eligibility standards prior to the enactment of the Aordable Care
Act—will receive enhanced Federal Financial Participation for services provided for newly eligible individuals:
100 percent in 2014, 2015, and 2016; 95 percent in 2017; 94 percent in 2018; 93 percent in 2019; and 90 percent
thereafter.
For more detailed information about this new eligibility group, see the State Medicaid Director Letter issued April
9, 2010 at http://www.cms.gov/smdl/downloads/SMD10005.PDF.
The Centers for Medicare & Medicaid Services (CMS) will be issuing additional guidance on other provisions con-
tained in §2001 of the Aordable Care Act at a later date.
42 Understanding Medicaid Home and Community Services: A Primer
General Rule
Neither SSI nor Medicaid determine eligibility by
comparing a person’s total income and resources to
the dollar thresholds that apply in the person’s eligi-
bility category. Rather, they count only certain types
and amounts. (This practice has a close counterpart
in income tax rules, which exempt certain types or
amounts of income from taxation and allow certain
types or amounts to be deducted from otherwise
taxable income.) For this reason, an individual can
have total income or resources higher than the
nominal eligibility limits (i.e., higher than $674 per
month in total income or $2,000 in total resources
for SSI) and still qualify for benets.
The general income rule for SSI species the level of
“countable income” at or below which an individual
is nancially eligible for benets. Countable income
includes cash income plus certain in-kind goods
or services that an individual receives in a given
month, minus certain types of exempted income
(discussed more fully below). In the year 2010,
the maximum monthly SSI benet paid to people
with no other income is $674 for an individual and
$1,011 for a couple. Persons with income from other
sources (e.g., Social Security or a pension) receive
a lesser amount—equal to the dierence between
the full SSI benet rate and the amount of their
countable income from other sources after adjust-
ments for income exclusions. For example, the SSI
benet for an individual with Social Security or pen-
sion income of $600 a month would be only $94 per
month ($600 minus a $20 disregard on unearned
income equals $580, which is deducted from the SSI
maximum monthly benet of $674).
Basic Medicaid Eligibility Rules
• Categorical criteria—Eligible persons must
• be age 65 or older, or
• be blind, or
• be under age 65 and have disabilities
(using the same criteria as for disability
in SSI).
• Income and resources—Eligible per-
sons must have incomes that are low or
severely reduced by medical expenses. In
addition,
• thresholds vary by eligibility category
and family size;
• some thresholds are established by
Federal law, some by states within
broad Federal guidelines; and
• thresholds must apply statewide ex-
cept under certain waivers.
• Legal status, residence, and eligibility re-
determination—Eligible persons must
• be a citizen or in appropriate immigra-
tion status;
• be a resident of the state or, if not, eli-
gible under an interstate compact; and
• report changes in circumstances and
have eligibility periodically re-deter-
mined by the state.
SSI rules reduce a person’s gross income to get
countable income in three important ways. First,
SSI disregards the rst $20 of every applicant/re-
cipient’s unearned income. Second—and of great
signicance to people with disabilities who work—
SSI provides a disregard of earnings from work,
amounting to the rst $65 ($85 if the person has
no other income in a month) plus one-half of the
remaining earnings amount.
8
However, if earnings
exceed $1,000 a month in 2010 then the individual
is considered to be engaging in Substantial Gain-
ful Activity, and thus does not meet the statutory
denition of being disabled.
9
Since the individual is
not considered to be disabled, he or she will prob-
ably have their SSI eligibility denied or terminated.
However, there are exceptions to this rule, which are

43
Chapter 2: Financial Eligibility Rules and Options
discussed below under “Reducing Employment Bar-
riers for Persons with Disabilities.”
Third, spouses or children with disabilities in fami-
lies with other members who are ineligible can
qualify for SSI at higher gross amounts of family
income, because SSI counts only the portion of the
non-disabled spouse’s or parent’s income that is
left after SSI subtracts amounts used to pay for the
basic needs of non-disabled family members. (SSI
may apply several other special-purpose reductions
also.)
The general rule denes countable resources as
cash or other property, including real property, that
(a)were acquired some time in the past, (b)the
individual has the right to access, and (c)could be
converted to cash and used to pay for current basic
living needs. Individuals with up to $2,000 ($3,000
for a couple) in countable resources can qualify for
SSI. When determining whether resources are below
the SSI $2,000/
$3,000 thresholds, SSI rules reduce gross resources
by exempting the home (regardless of value) and
(within limits) such things as an automobile, house-
hold goods, surrender value of life insurance, burial
funds, and property essential to self-support. States
often use SSI resource limits when determining
eligibility for Medicaid.
Exceptions to the General Rule
There are two major exceptions to the general rule:
the 209(b) option and protection for certain former
SSI beneciaries. (Mandatory Medicaid protection
for certain children with disabilities and certain
working persons with disabilities is discussed later
in this chapter.)
State 209(b) Option
Medicaid for the “Aged, Blind, and Disabled” had
historically always been linked to receipt of cash
assistance benets. When SSI replaced state-only
programs of aid for elderly persons and persons
with disabilities, it was expected to lead to large
increases in the numbers of SSI beneciaries. The
209(b) option was enacted along with SSI in 1972
to enable states to avoid similarly large increases in
Medicaid enrollment and costs.
Many Medicaid eligibility rules in 209(b) states fol-
low SSI. But states may choose, instead, to use some
or all of the more restrictive Medicaid rules in eect
in their state on January 1, 1972, shortly before SSI
was enacted. Eleven states have retained at least
some of their pre-SSI rules on countable income or
resources, and some use more stringent criteria for
determining blindness or disability.
To counterbalance the potential negative eects of
the 209(b) option on SSI beneciaries, Federal rules
require 209(b) states to allow any residents who are
elderly, blind, or have disabilities—including those
with too much income for SSI—to spend down to
the state’s Medicaid income standard if their ex-
penses for medical and remedial services so erode
their income that their “net” remaining income
would be less than a standard set by the state. This
requirement creates a medically needy-like program
for this population, even in states that have not cho-
sen specically to cover the medically needy as an
option. Spend-down rules for 209(b) states are virtu-
ally identical to spend-down rules for the Medicaid
medically needy category (discussed below).
Medicaid Protection for
Certain Former SSI Beneciaries
Federal law requires all states, including 209(b)
states, to provide Medicaid to former SSI bene-
ciaries who would, but for increases in their Social
Security benets, continue to be eligible for SSI.
Congress passed this provision to ensure that Social
Security increases, intended to improve people’s
lives, did not instead harm this group by causing
them to lose Medicaid as well as SSI. Most of the
individuals aected have incomes just marginally
44 Understanding Medicaid Home and Community Services: A Primer
above the income levels at which they might qualify
for SSI/Medicaid combined benets. In fact, many
people who could qualify for Medicaid under these
provisions do not apply for the program, most likely
because they are not aware of them. Improved
understanding of these protections could possibly
increase Medicaid enrollment of this group.
Former SSI Beneciary Groups
with Medicaid Protection
• People who lost SSI when they received au-
tomatic cost-of-living adjustments (COLAs)
in Social Security (sometimes nicknamed
“Pickle people” after Congressman Pickle,
one of the sponsors of the original COLA
legislation).
• Adult children with disabilities who lose
SSI because they become entitled to Social
Security benets based on a parent’s Social
Security entitlement.
• Individuals ages 60–64 who lose SSI due
to receipt of Social Security benets for
widows and widowers with disabilities.
Medicaid Exceptions to SSI Countable Income
and Resources Rules
In general, states use SSI rules in determining what
is countable income and resources for
Medicaid eligibility. However, states have the option
to liberalize their Medicaid rules regarding count-
able income or assets in such a way that the eligi-
bility limits specied in law, while still theoretically
required, can be greatly exceeded.
11
It is important to note that this exibility comes
with certain restrictions. First, the dierent count-
ing methods must not disadvantage anyone, even
if relatively more people would benet than would
be disadvantaged. Second, although a state may
restrict its more liberal counting method to one or
more eligibility groups, those selected must be one
of those specically dened in the part of the Med-
icaid law that authorizes the use of this option—for
example, working persons with disabilities, poverty-
related groups, or the medically needy (all of which
are discussed more fully below). Thus, states are
not permitted to carve out a subgroup of their own
denition (e.g., one based on medical diagnosis or
place of residence, such as residential care facilities).
Examples of Provisions That Can Reduce
Countable Income or Resources
• Allow more than the standard SSI income
disregard of $20.
• Disregard higher amounts of work earn-
ings.
• Disregard all or part of certain types of
resources that are limited under SSI; for
example, income-producing property
essential to self-support, burial funds, and
the cash value of life insurance.
Third, exibility in counting income is highly limited
for medically needy eligibility groups (described
below), because Federal law imposes a ceiling on
medically needy income levels (133
1
/
3
percent of the
highest amount paid to an AFDC family of the same
size). States are not permitted to exceed this ceiling,
which limits opportunities for states with medically
needy income levels at or close to the ceiling.
12
While Federal rules give states broad exibility to
expand eligibility, actual adoption of more gener-
ous alternative methods must, of course, conform to
a state’s budget considerations and political deci-
sions.
Eligibility Expansion Options
Including, but Not Specic to,
Home and Community Services
Certain state Medicaid options for across-the-board
eligibility expansions capture anyone who meets
the criteria, including but not limited to persons
needing long-term care services. Because these
options cannot be targeted, their cost implications
make them unlikely choices for states looking for
limited HCBS expansions. However, states may be

45
Chapter 2: Financial Eligibility Rules and Options
encouraged to adopt these eligibility expansions for
other sensible reasons. For example, people eligible
under any of these expansion options receive the
full range of health and long-term care services cov-
ered under the State Plan. In addition, if they meet
the state’s criteria for HCBS waiver participation
(e.g., level of care, diagnosis, or place of residence)
they can receive waiver services.
100 Percent of Poverty Option
States have the option of raising the income eligibil-
ity level for persons over age 65 and persons under
age 65 with disabilities as high as 100 percent of
the Federal poverty level ($10,830 for one person
in calendar year 2010, increasing incrementally for
additional family members).
13
The state’s eligibility
limits on countable resources must be at the SSI
levels ($2,000 for one person, $3,000 for a couple),
or at the state’s option, its medically needy resource
levels if they are higher than SSI levels.
It bears repeating here that what is compared
to these eligibility levels is countable (not total)
income and assets. At the very least, states must
disregard the same kinds and amounts of income
and resources that SSI disregards.
14
Medically Needy Option
States can cover people with too much income to
meet nancial eligibility criteria through the medi-
cally needy option. There is no specied ceiling
on how much income a person can have and still
potentially qualify if their medical bills are high
enough. However, a number of requirements limit
the attractiveness of the medically needy option
for higher income people needing long-term care,
especially home and community services, relative
to the more narrowly targeted options discussed in
the next section. Requirements include the follow-
ing:
• Individuals must t into one of the Medicaid
categories for coverage—for example, be age
65 or older or meet the Social Security Ad-
ministration criteria for disability. If not, they
cannot qualify as medically needy no matter
how low their incomes or how extensive their
medical need.
• At a minimum, states choosing this option
must rst cover medically needy pregnant
women and children. Most states that cover
the medically needy also extend coverage to
elderly persons or persons with disabilities.
• States may not restrict eligibility based on
medical condition, type of services needed, or
place of residence.
• Eligibility limits on resources are typically the
same as for SSI.
15
• States must use a single eligibility level for
income and resources for all medically needy
groups they elect to cover. In the case of
income levels, this single level may not exceed
133
1
/
3
percent of the state’s pre-welfare re form
AFDC payment levels. Where these are very
low, the medically needy income levels may be
less than the SSI level.
• Medically needy people with incomes above
the state’s threshold must spend down before
becoming eligible for Medicaid benets.
This last, the spend-down requirement, can be a
major impediment for higher income people who
wish to qualify for home and community services
through the medically needy provision. The rea-
son is that medically needy people with incomes
above the state’s Medicaid income threshold must
spend down to that threshold on a periodic basis in
order to remain eligible for Medicaid funding of the
services they need.
16
Until their spend-down limit is
reached, they are responsible for their own medical
expenses.
46 Understanding Medicaid Home and Community Services: A Primer
General Eligibility Expansion Options
100 percent of the Federal poverty level
• Allows states to provide full Medicaid
benets to all elderly persons or persons
with disabilities with countable income up
to the Federal poverty level and assets at
or below state limits.
Medically needy
• Allows eligibility for those who would
qualify except for income.
• Higher income persons must spend down
their income to Medicaid eligibility levels.
• States may not cover medically needy who
are elderly or have disabilities without
also covering medically needy pregnant
women and children.
There is no Federal or state requirement that indi-
viduals spending down actually pay their bills. But
as a practical matter, providers are unlikely to con-
tinue serving them if they fail to pay. Alternatively,
states can oer people the opportunity to meet
their spend-down obligation by paying it directly
to the state in exchange for immediate coverage of
all their medical expenses. In either case, however,
people with incomes well above the state threshold
may have a spend-down liability that leaves them
insucient income to cover all their expenses at
their current living standards.
Hypothetical Spend-Down Situation
Assume the state’s medically needy income
level for an individual is $450 per month. For
individuals with monthly countable income of
$950, spend-down liability is $950 minus $450
(= $500), which may be a manageable amount
for those with high time-limited medical needs
or those in nursing homes who do not need
income to maintain a home and pay other com-
munity living expenses.
Because of these limitations, spend-down works
best for people in three kinds of situations: (a)they
have a one-time, short-term need for assistance;
(b)they are permanently in an institution and no
longer need income to maintain community resi-
dence; or (c)their income is low enough to result
in a spend-down liability that is aordable to them.
(Spend-down is discussed in Chapter 5 as it relates
to payment of room and board in residential care
facilities.)
Eligibility Expansion Options That Can Be
Targeted to Persons Needing Home and
Community Services
This section discusses options states can use to ap-
ply income standards that allow people with higher
incomes to qualify—and can be targeted more nar-
rowly to people needing long-term care services in
a variety of home and community settings.
State Supplemental Payments (SSPs)
Many states supplement the basic SSI payment and
pair these supplementary payments with automatic
Medicaid eligibility. This combination of benets en-
ables beneciaries to obtain the services they need
in a range of community settings.
The maximum monthly Federal SSI benet ($674
in 2010) is assumed to be minimally sucient to
enable recipients to pay for a basic level of ordinary
living expenses (food, shelter, clothing). Many states
have elected to spend state-only funds to supple-
ment the basic SSI benet in circumstances where
they have determined that rate to be insucient
to cover living expenses necessary for minimally
adequate living standards. These state supplements
are state-determined and vary widely.
17
Some indi-
viduals have too much income to qualify for SSI but
may qualify for an SSP benet only. States can elect
to make such persons automatically eligible for
Medicaid, just as they can for SSI beneciaries.
47
Chapter 2: Financial Eligibility Rules and Options
State Supplemental Payments
• States can supplement the basic SSI pay-
ment.
• States can pay across-the-board SSPs to all
elderly persons or persons with disabilities
in the state, or they can target them to
persons in supported living settings.
• States can provide Medicaid to people
receiving an SSP who are not eligible for
SSI.
Few states provide across-the-board state supple-
ments to SSI. Most target them specically to
persons who are unable to live independently but
do not need an institutional level of care. The state
supplement can be used to help pay for services
provided in residential care settings such as foster
care, group homes, assisted living, and other set-
tings dened by the state. Services in these settings
can vary widely—consisting of as little as house-
keeping or general supervision, to various levels of
assistance with activities of daily living.
Automatic Medicaid eligibility for state supplement
beneciaries provides an additional measure of
assistance in paying for needed medical services.
States have broad exibility with respect to not
only the level of SSP support but also the kinds of
settings to be supported, quality standards, and
oversight. States can pay SSPs for as many dierent
types of supported living settings as they wish.
How a State Supplemental Payment
Might Work
In the year 2010, the Federal SSI monthly benet
rate is $674 for an individual. Assume a state sets
its supplemental benet at $200 (making the
SSP benet $874). Then,
• a person receiving Federal SSI would re-
ceive an additional SSP of $200 per month.
• a person with countable income of
$774—from, say, Social Security or a pen-
sion—would have $80 ($100 minus $20
disregard) too much income to qualify
for SSI, but would still qualify for a $100
SSP benet, and at the state’s option, for
Medicaid.
As with many other Medicaid options, the option
states have to provide Medicaid to SSP beneciaries
not eligible for SSI is subject to certain conditions.
The SSP must be based on need, and the state must
pay the SSP on a regular basis to anyone in the sup-
ported living setting to which the SSP applies who,
but for income, would qualify for SSI. There is no
rule obligating the state to establish such settings
throughout the state. If the particular type of living
setting supported by a state’s SSP happens to exist
only in limited areas of a state, the state is permitted
to pay SSPs just to persons in those settings.
300 Percent of SSI Income Option
The 300 percent of SSI income option (hereafter
called the 300 percent option) was originally cre-
ated so that states not wishing to cover the entire
category of medically needy could at least cover
higher income persons residing in a medical insti-
tution. States electing this option may establish a
special income threshold, applicable to a person’s
gross income (all income, not just countable in-
come), as high as 300 percent of the maximum SSI
benet—$2,022 per month and $24,264 per year in
2010. Persons who qualify based on income must
also have resources within Medicaid eligibility limits.
States typically use the same asset limits as SSI, but
they may use more liberal Medicaid exemption
rules.
18
48 Understanding Medicaid Home and Community Services: A Primer
Overview of the 300 Percent of SSI In-
come Rule
• Allows eligibility for persons with gross
incomes at or below 300 percent of the
current SSI benet—$2,022 per month in
2010.
• Allows states to use the option for persons
residing in institutions, such as a nursing
home or intermediate care facility for per-
sons with intellectual disabilities (ICF/ID).
If they do so, states can also extend the
300 percent of income rule to eligibility for
HCBS waiver applicants.
• Allows states to provide waiver services to
children without regard to their parents’
income or assets and to married indi-
viduals without regard to their spouse’s
income.
• Requires states to impose a post-eligibility
cost-sharing requirement (discussed fur-
ther below).
• When the 300 percent rule is a state’s only
option for providing Medicaid to higher
income persons in institutions (i.e., the
state does not have a medically needy pro-
gram), allows persons to become eligible
by diverting excess income into a Miller
trust (discussed below).
When originally created, the 300 percent option was
limited to persons in institutions, because home
and community service alternatives to nursing
homes were extremely limited. However, when the
HCBS waiver authority was enacted in 1981, states
were allowed to extend the 300 percent option to
waiver applicants. The goal was laudable: to enable
states to neutralize incentives for individuals to
choose a nursing home over home and community
services simply because of Medicaid nancial eligi-
bility rules.
However, the eectiveness of the 300 percent op-
tion in increasing access to home and community
services is limited by two important factors. First, it
can be used only for HCBS waiver participants, not
for those receiving personal care or home and com-
munity-based services under the State Plan. Second,
individuals eligible under this option, whether in an
institutional setting or in an HCBS waiver program,
are subject to a post-eligibility share-of-cost obliga-
tion (described below).
Miller Trusts
In states where the eligibility of higher income
persons is limited to those qualifying under the 300
percent option, individuals with too much income
to qualify for Medicaid even under this rule may still
qualify by diverting their income into what is known
as a Miller trust. Miller trusts are not limited to per-
sons needing Medicaid for nursing home care or for
services provided under an HCBS waiver. State Med-
icaid agencies may choose, but are not required, to
play a role in helping establish these trusts.
To qualify as a Miller trust, contributions must
consist solely of the individual’s funds (income such
as monthly Social Security or pension benets,
but not resources) and must be used solely for the
benet of the individual. There are no limits on how
much income can be placed in the trust. However,
if amounts paid out of the trust exceed the fair
market value of goods and services on behalf of
the individual, then the individual may be at risk
of a penalty for an uncompensated asset transfer,
resulting in loss of Medicaid coverage for needed
services. Additionally, amounts paid out of the trust
may count as income—whether paid directly to the
beneciary or paid to purchase something on their
behalf (other than medical care).
19
This “income”
must be under the eligibility level in the state and is
subject to post-eligibility share-of-cost rules. Finally,
the trust must specify that the state will receive any
amounts remaining after the person’s death, up to
the amount the state paid in Medicaid benets for
the Miller trust owner.
20

49
Chapter 2: Financial Eligibility Rules and Options
Protected Amounts in Calculating
Post-Eligibility Share-of-Cost Obligation
(an obligation that applies only to
certain beneciary groups)
21
People who become eligible for Medicaid under
the 300 percent option, whether in a nursing home
or an HCBS waiver program, are typically expected
to pay a share of their income toward the cost of
their care, which they pay providers directly.
22
This
post-eligibility share-of-cost obligation can be quite
high, depending on the individual’s circumstances
and the options the state has chosen. However, un-
like nursing home care, which requires beneciaries
to contribute all but a personal needs allowance
and other amounts described below, state waiver
programs have greater exibility to determine how
much income HCBS waiver participants can retain;
some states require little or no cost sharing. As with
the medically needy spend-down provision, Federal
rules do not require the individual to actually pay
the share-of-cost amount but service providers can
ensure payment through their usual bill collection
policies.
The share-of-cost calculation is made by subtracting
from total income certain amounts that are protect-
ed for the individual’s personal use. The remaining
income is the individual’s share-of-cost obligation.
The Medicaid program reduces the amount it pays
for Medicaid services by the amount the individual
is expected to pay. Protected amounts include
Amounts to cover basic needs. States must allow
persons in nursing facilities and ICFs/
ID to keep a minimum of $30 per month to cover
personal needs. States also have the option to
establish a higher amount across the board, or to
establish higher amounts for reasonable groups.
The personal needs allowance is set at a low level
because the institution provides for most of the in-
dividual’s basic living needs. The institution receives
Medicaid payment for services it provides as part of
its daily payment rate.
States establish higher allowance amounts for
people eligible under the 300 percent option in
HCBS waiver programs, because waiver participants
must have sucient funds to cover their community
living expenses. A state can set the allowances for
this group equal to the income eligibility thresholds
that apply to other Medicaid eligibility groups in
the state (e.g., at the SSI or medically needy income
levels). The most generous HCBS waiver programs
allow eligible individuals to retain all their income
for personal use, thereby eectively eliminating any
beneciary liability for a share of cost and making
Medicaid pay the entire cost of covered services.
State decisions depend in part on budget concerns,
because the less beneciaries spend as their share
of cost, the more the state must contribute.
Allowance for a spouse or other dependents. States
must deduct income to provide for a spouse of
an individual in an institution. The amounts pro-
tected for spouses of institutionalized persons are
governed by the rules designed to protect against
spousal impoverishment. States have the option to
implement spousal impoverishment protections
when one spouse is an HCBS waiver program (dis-
cussed in the next section).
Home maintenance allowance (at state option).
Persons in an institution can, at state option, retain
an additional amount for up to 6 months if needed
for maintenance of a home. This allowance is limited
to those who can reasonably be expected to return
to their homes. This optional allowance is not avail-
able to individuals receiving waiver services since
their basic needs allowance (discussed above) is
intended to include maintenance of a home.
Amounts to cover other medical expenses. States
must allow nursing home and ICF/ID residents, as
well as HCBS waiver participants, to retain enough
income to pay for additional medical costs they
incur that are not paid for by Medicare, Medicaid,
or any other payer. Long-term care expenses (e.g.,
home health aides, personal assistants, and adult
day care) can be counted toward required medically
needy spend-down amounts as long as the indi-
vidual rather than some third party is responsible
for paying the expense.
50 Understanding Medicaid Home and Community Services: A Primer
Preventing Spousal Impoverishment
In 1988, Congress mandated that states allow mar-
ried couples separated by the institutionalization
of one spouse to protect a certain amount of assets
and income for the non-institutionalized spouse.
This mandate applies regardless of how the institu-
tionalized person establishes eligibility. Prior to this
law, states protected no assets, and the amounts
of income they protected for the support of the at-
home spouse were at welfare-like levels—a devas-
tating event for middle-class couples facing, per-
haps for the rst time in their lives, a need for public
assistance because of the high cost of nursing home
care.
States have the option to implement spousal
impoverishment protections when one spouse is
an HCBS waiver program. Doing so enables states
to protect the income and assets of the spouses of
waiver participants to the same extent they do for
spouses of Medicaid residents in institutions.
How spousal impoverishment protection works
is described here for states that wish to use it for
HCBS waiver participants. There are two decisions
states make within the Federal limits: (a)how much
income to protect, and (b)what amount of assets
(resources) to protect.
Income Protection
Income is protected for the spouse after the person
needing long-term care has been determined eligi-
ble for Medicaid. The minimum monthly protected
spousal income amount is $1,821 in the year 2010
(see Table 2-1). Additional amounts, up to a maxi-
mum of $2,739, are protected if the spouse has un-
usually high housing costs or if the state has chosen
to protect more than the mini-mum amount for all
spouses. If income belonging to the spouse is less
than the protected level, the Medicaid beneciary
can transfer his or her own income to the spouse to
make up the shortfall. States count any remaining
income of the Medicaid beneciary, less the allow-
ance for the spouse, in calculating the share of the
Medicaid service costs for which the beneciary is
responsible.
Temporary Expansion of Spousal
Impoverishment Protections
23
The Aordable Care Act amended the spousal
impoverishment statute to mandate that states
include spousal impoverishment protections in
their HCBS waiver programs; all spouses of HCBS
waiver participants, including those who qualify
as medically needy, are covered. The mandate
also extends to the spouses of participants
in the HCBS State Plan benet, as well as the
new Community First Choice Option State Plan
benet (eective October 2011). The mandate
will be eective from January 1, 2014 through
December 31, 2019, at which point the current
language of the statute will become eective
again (i.e., spousal protections will be optional
for spouses of HCBS waiver, HCBS State Plan, and
Community First Choice Option participants).
Spousal impoverishment protections, at least as
they pertain to income, are generally part of the
unique Federal post-eligibility income treatment
rules applicable to Medicaid-enrolled nursing
facility residents and HCBS waiver participants.
When applying these rules, states allocate spe-
cic portions of an enrollee’s monthly income
between a personal maintenance allowance, a
community spouse maintenance allowance, and
the enrollee’s share of the cost of the covered
services. However, Medicaid enrollees not in a
nursing facility or HCBS waiver but receiving
other State Plan services, may have co-pays for
services they receive but will not be subject to
the same income allocations as nursing facil-
ity or HCBS waiver participants. Thus, CMS will
have to provide guidance to states for applying
spousal protections for the spouses of State Plan
service recipients.
51
Chapter 2: Financial Eligibility Rules and Options
Table 2-1. Examples of Spousal Income Protection
Assume the minimum protection allowance ($1,821) applies
Example 1:
Beneciary’s income
Spouse’s income
Beneciary income protected for spouse
Beneciary income for calculating share-of-cost obligation
$2,000
None
$1,821
$179 ($2,000 – $1,821)
Example 2:
Beneciary’s income
Spouse’s income
Beneciary income protected for spouse
Beneciary income for calculating share-of-cost obligation
$2,000
$1,000
$821 ($1,821 – $1,000)
$1,179 ($2,000 – $821)
Example 3:
Beneciary’s income
Spouse’s income
Beneciary income protected for spouse
Beneciary income for calculating share-of-cost obligation
$2,000
$2,000
None
$2,000
Resource Protection
The resource amount protected for the spouse is determined as part of the process of determining Medic-
aid eligibility of the person needing services. Countable resources belonging to either or both spouses are
combined and divided in half. The amount protected for the spouse is either that half, or the level the state
has chosen to protect, whichever is higher. In 2010, the amount protected is subject to a Federal minimum
($21,912) and maximum ($109,560).
Any resources not protected for the spouse are considered available to the person needing care, who is not
eligible until such resources are within Medicaid eligibility limits.
Minimum and maximum amounts of both income and resources increase every year based on the cost-of-liv-
ing increase as published by the Department of Health and Human Services. In addition, Federal law requires
states to have administrative and judicial procedures in place that allow petitioners to seek higher protected
amounts of the spouse’s assets. For example, spouses can petition for higher protected assets if the income
those assets produce is needed for their reasonable living expenses.
Provisions Specic to Children with Disabilities
Two eligibility provisions—one mandatory and the other at states’ option—were enacted specically to serve
children with disabilities. The mandatory provision—sometimes called Zebley Kids or 4913 Children—relates
to children rendered no longer eligible by a 1996 change in the SSI denition of disability for children. The Ze-
bley designation comes from a court case, contesting the 1996 change.
24
The optional provision—some-times
called the Katie Beckett or Tax Equity and Fiscal Responsibility Act (TEFRA) option—allows for eligibility for a
child with severe disabilities living at home, regardless of the nancial circumstances of the child’s parents.

52 Understanding Medicaid Home and Community Services: A Primer
Zebley Kids
The welfare reform legislation of 1996 made it
more dicult for children to qualify as disabled SSI
beneciaries by changing the denition of disabil-
ity for children. The major impact of this change
was on children with mental disorders. In 1997, a
new Federal requirement was enacted protecting
Medicaid eligibility for former child beneciaries of
SSI who lost it due to this denitional change. This
protection is retroactive to the original SSI change
in 1996. However, it cannot produce actual eligi-
bility changes unless both state and family follow
through and take all necessary administrative steps
to get the child enrolled specically in the state’s
Medicaid program. It is important to note that
children who apply for SSI for the rst time and are
found ineligible might still qualify for Medicaid or
for their state’s Children’s Health Insurance Program,
based on the family’s income.
Katie Beckett Option
States typically follow Federal SSI rules on whether
or not to count (deem) the income and resources
of a parent in determining a minor child’s nancial
eligibility.
25
These rules impart a substantial institu-
tional bias by ignoring parental income/resources
when assessing eligibility for long-term care ser-
vices if a minor child is living in an institution, but
counting them if the minor child lives at home.
26
These dierent deeming rules make it much more
likely that a minor child will meet Medicaid’s nan-
cial eligibility test when living in an institution than
at home. Thus, families considering how to get
long-term care services for a minor child with dis-
abilities may nd that these deeming rules leave no
realistic alternative to institutionalization.
States can overcome this institutional bias through
two options. The rst, the Katie Beckett or TEFRA
option, was enacted permanently into law in 1982.
This option enables states to provide Medicaid to
certain children with disabilities living at home who
need extensive care but who would, without the
option, be unable to qualify because their parents’
income or resource levels put them above the nan-
cial eligibility cuto.
27
Before this option became available, children with
disabilities were typically eligible for SSI—and, thus,
Medicaid—only if they lived in institutional settings.
This was because of deeming rules discussed above.
Most state Medicaid programs followed SSI deem-
ing rules on how income and resources are counted.
Under these rules, institutionalized children were
not considered part of their parents’ households.
Parental income and assets were therefore ignored,
regardless of their magnitude. But children liv-
ing with their parents were considered part of the
parental household, making parental income and
assets deemed available to the children, and sub-
stantially reducing the likelihood that children with
disabilities would be eligible for Medicaid services,
no matter how great the children’s service needs
might have been. This arrangement made it possi-
ble for children with disabilities in non-poor families
to get Medicaid for institutional care but not for
equivalent care provided at home.
The TEFRA option, which was enacted to create
equity between the two settings with regard to
nancial eligibility, is limited in the following ways.
First, home care for the child must be appropriate.
Second, the estimated cost of community services
for the child may not exceed the cost of institu-
tional care. Third, the child must require the level
of care normally provided in an institution, making
the TEFRA option unavailable for children whose
disabilities do not require this level of care. In states
that use the TEFRA option, parents may choose
either institutional or community care for their
Medicaid-eligible children, subject to the above
requirements.
Alternatively, states can elect to use institutional eli-
gibility rules when determining a minor’s eligibility
for an HCBS waiver program. Using institutional eli-
gibility rules means, among other things, choosing
not to deem the income and resources of parents
available to minor children eligible under an HCBS
waiver program. Doing so provides access to home
and community services on the same nancial basis
as long-term care services provided in an institu-
tion.
States need to consider the following points when
choosing between the TEFRA option and the HCBS
waiver option for covering children with disabilities.
53
Chapter 2: Financial Eligibility Rules and Options
First, states may not impose enrollment caps under
the TEFRA option, as they can under the HCBS
waiver option. If elected, the TEFRA option must
be available to anyone who qualies anywhere in
the state. Second, states must provide to children
eligible under both the TEFRA option and the HCBS
waiver option the same Early, Periodic, Screening,
Diagnosis, and Treatment benets provided to
all other Medicaid children in the state. However,
the HCBS option allows states to oer additional
services of a non-medical nature. Finally, states may
impose a share-of-cost obligation on children in an
HCBS waiver program but not on children eligible
under the TEFRA option.
Reducing Financial Barriers to Employ-
ment for Persons with Disabilities
Any benet program that uses an income cuto to
determine eligibility contains a major disincentive
for beneciaries to work, if the earnings from that
work would put them above the nancial eligibility
level for benets. To the extent that Medicaid cover-
age is needed for essential health care, the problem
becomes an absolute barrier to employment rather
than simply a “disincentive.”
In order to preserve the incentive for persons with
disabilities to work as much as they are able with-
out fear that doing so will cause them to lose their
medical coverage, Federal law mandates states to
disregard certain earnings amounts in determining
eligibility for Medicaid. States have additional op-
tions to protect the earnings of people with disabili-
ties who have higher earning potential.
Federal Provisions
28
Since 1982, certain SSI disability beneciaries
who are able to work and earn more than the SGA
amount ($1,000 per month for 2010) have been
permitted to keep their SSI and Medicaid benets,
provided their countable income is within SSI quali-
fying limits. Under this provision, individuals with
earnings up to $1,433 per month in 2010 are typi-
cally able to continue receiving SSI cash benets.
29
Former SSI beneciaries with even higher earnings
may continue to qualify for Medicaid, as long as
their earnings are below a state-specied level that
is roughly equivalent to the value of the total SSI
and Medicaid benets they would receive if they did
not work.
30
The Medicaid component of this amount
is the average amount spent by Medicaid for bene-
ciaries with disabilities in the relevant state. States
must provide Medicaid to individuals with earnings
above even this level, if they can show that their
medical expenses are higher than the state aver-
age used to establish the cuto. The Social Security
Administration administers both provisions.
Little use was made of these protections at rst
because they were not widely understood. Thus, the
number of working persons with disabilities whose
earnings were protected in this manner in 1982,
the rst full year of implementation, was just under
6,000. By September 1999, however, the number
had risen to nearly 100,000.
31
In December 2008,
there were 355,762 SSI disabled beneciaries who
were working—only 5.5 percent of the total SSI
blind and disabled case load—with average earn-
ings of $605 a month; 23 percent earned $65 or less
per month.
32
State Options
Advocates for persons with disabilities argue that
the work incentive provisions have not been widely
used for several reasons. First, receipt of SSI benets
is the gateway to Medicaid—both for health and
long-term care services. Because there is an abso-
lute income cap for Medicaid eligibility—however
high that limit may be—there is an absolute drop-
o point at which increased additional earning will
result in a loss of Medicaid. Second, low asset limits
mean that working persons with disabilities are un-
able to increase their savings without jeopardizing
their Medicaid eligibility.
Congress addressed some of these Medicaid access
problems with laws enacted in 1997 and in 1999.
33
The 1997 provision allows states the option of ex-
panding eligibility for persons with disabilities who
have countable income from all sources up to 250
percent of the Federal poverty level—$27,075 for
an individual, $55,125 for a family of four in the year
54 Understanding Medicaid Home and Community Services: A Primer
2010. These individuals need not ever have received
SSI but they must—except for the level of their
work earnings—meet SSI disability criteria.
The 1999 provision gives states the option to cover
individuals with disabilities who currently work
without regard to their earnings, and to raise or
even eliminate eligibility limits on income from
other sources and/or limits on assets. States that
have elected this option can also elect to continue
coverage for persons (eligible under this option)
whose disability remains severe—but whose medi-
cal condition has improved to a point that they no
longer meet the usual Medicaid eligibility criteria
dening disability. For these higher income enroll-
ees, states have the option to impose a monthly
premium or other cost-sharing obligations for their
Medicaid benets using a sliding scale based on in-
come. States choosing the 1999 option are required
to charge 100 percent of the premium for those
with an adjusted gross income (AGI) greater than
$75,000 (AGI as dened for Federal income tax pur-
poses).
34
The term “buy-in” is used to describe these
options. The state, not the Social Security Adminis-
tration, makes the eligibility determination for these
state work incentive options.
Asset/Resource Transfers: Permissions
and Penalties
Federal law imposes a penalty on persons who give
away savings or transfer ownership of their assets
for less than fair market value (termed uncompen-
sated transfers) in order to meet Medi caid’s nancial
eligibility criteria. The penalty applies to all eligibil-
ity groups in all states.
35
The purpose of the penalty
is to preclude the payment of benets to individuals
who can aord to pay for them. States must apply
this penalty to people seeking Medicaid coverage
for nursing homes, other institutions, and HCBS
waiver programs for individuals eligible under what
are known as “institutional” rules. The penalty is
mandatory for individuals in institutions and those
eligible for HCBS waivers under institutional rules,
but is optional for those eligible under community
rules.
Structure of the Penalty
Both SSI and Medicaid deny benets for people
making uncompensated asset transfers. The nature
and eective duration of the penalty, however,
dier between the two programs.
36
The following
discussion relates to the Medicaid provisions.
Terminology
The terms “assets” and “resources” are used
interchangeably to refer to savings, stocks and
bonds, and other property. However, Medicaid
law specically related to asset transfers in-
cludes “income” in the denition of assets.
The general Medicaid rule is that states must deter-
mine whether an applicant, beneciary, or someone
acting on their behalf transferred assets (including
the home) at any time during the 36 months prior
to applying for Medicaid.
37
For assets transferred af-
ter February 2006, the Decit Reduction Act of 2005
(DRA-2005) extended the timeframe to 60 months.
If a person did not receive fair market compensa-
tion, then states presume the transfer was made
to qualify for Medicaid. States are required to have
procedures in place that allow applicants to chal-
lenge that presumption.
Permissible Transfers
Certain transfers can be made without penalty:
Transfers made to a spouse or a third party for the
spouse’s benet.
Transfers of a home to a minor child or child with
disabilities, or siblings or adult children who have
lived in the home before the beneciary was admit-
ted to an institution or the waiver program, and
who meet certain other conditions.
38
Transfers by Medicaid applicants/recipients to their
blind children or children with disabilities or to a
trust for those children’s benet, regardless of the
child’s age.
55
Chapter 2: Financial Eligibility Rules and Options
Assets transferred into a trust solely for the benet
of a person under age 65 with a disability. Eligible
trusts include special needs trusts and pooled trusts
established by a nonprot association that manages
multiple accounts.
39
These trusts are not counted in
Medicaid’s resource eligibility determination.
When a state has determined that an impermissible
transfer has taken place, it must deny coverage for
long-term care services in an institution or through
an HCBS waiver program. Coverage may also be de-
nied at state option for long-term care services such
as home health or personal care provided through
the State Plan for individuals who are not residing in
institutions. For the most part, such penalties do not
aect the person’s eligibility to receive any other
services under the Medicaid State Plan.
States calculate the duration of the penalty based
on private pay nursing facility rates—whether the
person who has transferred assets is actually in a
nursing home or seeking home and community
services—even though the monthly cost of services
in the community is likely to be substantially lower.
The duration of the penalty is calculated by dividing
the uncompensated value of the transferred assets
by the monthly cost of care in a private nursing fa-
cility. The same formula is used for people applying
for services through an HCBS waiver program.
The penalty calculation is the same regardless of
(a)whether the person was living at home or in a
facility at the time of transfer, and (b)whether the
person was actually using or paying for services.
However, Federal law requires that states make
exceptions in cases of undue hardship.
Prior to February 2006, the rule regarding the pen-
alty start date—the month the transfer occurred—
reduced or eliminated the eect of the penalty,
depending on the amount of the transfer and the
amount of time that passed between the date of
the transfer and the date of application to Medicaid.
Thus, if a transfer was modest and occurred rela-
tively early in the 3-year look-back period before
the individual applied for Medicaid, it often had no
eect.
To correct this situation, the DRA-2005 changed
the start date for the penalty period for all transfers
made after February 2006 and extended the look-
back period from 3 to 5 years. A penalty for transfers
made after February 2006 now begins the month an
individual becomes eligible for
Medicaid and is in a nursing facility or other institu-
tion or who is eligible for an HCBS waiver based on
institutional rules.
40
Eect of Transfer on Benet Loss:
Example for Transfers
• A person withdrew $20,000 from savings
and gave it to an adult child on January 1,
2005.
• The person is receiving an institutional level
of care—that is, she is either in a nursing
home or is eligible for waiver services based
on institutional rules—on April 1, 2009.
• The monthly cost of nursing facility services
is $4,000.
• The penalty period is 5 months ($20,000
divided by $4,000).
• The 5-month penalty period begins
on the date the person is eligible for Med-
icaid; in this example, from April 1 through
August 31, 2009. During the 5-month penal-
ty period, a person who is eligible for Med-
icaid can receive services other than long-
term care services. Once the penalty period
is no longer in eect (beginning September
1), the person can receive coverage for
long-term care as well as other services.
41
56 Understanding Medicaid Home and Community Services: A Primer
Estate Recoveries
Federal law requires all states to recover assets from
the estates of two groups of Medicaid beneciaries
after their deaths: those who were age 55 or older
when they received Medicaid benets, and those
who received Medicaid nursing facility or ICF/ID
benets regardless of age. At a minimum, states
must use the same denition of estate used under
their probate laws. They are permitted to use a
broader, state-established denition that captures
additional assets.
States are mandated to recover any amounts they
have paid on the individual’s behalf for any type of
long-term care services, as well as any hospital costs
and prescription drug benets related to the condi-
tion requiring long-term care services. They also
have the option of recovering all amounts spent on
other Medicaid benets. But state recovery actions
must be delayed if there is a surviving spouse or, in
certain cases, a child or sibling living in the home.
States have the option of not pursuing recovery in
the case of very small estates, if the cost of doing
so is likely to exceed the amount that can be re-
covered. (See the Resources section of this chapter
for links to several publications about states’ estate
recovery policies.)
Disqualication for Long-Term Care
Medicaid Coverage for Individuals with
Substantial Home Equity
Under Medicaid, an applicant’s home, regardless of
its value, is generally an exempt resource for eli-
gibility purposes. The DRA-2005 does not change
this basic rule, but for applications led on or after
January 1, 2006, it limits the exemption to individu-
als whose equity interest in their homes is $500,000
or less, or at state option, a higher amount not to
exceed $750,000. For those with home equity above
the amount the state has set, the state must deny
Medicaid payment for long-term care services (in-
cluding those provided through HCBS waiver pro-
grams). States that choose to use an amount higher
than $500,000 need not use this amount on a state-
wide basis, recognizing potentially wide variations
in the cost of housing statewide. Also, states need
not apply the higher amount to all eligibility groups.
The new limits on home equity do not apply to an
individual if the individual’s spouse, child under age
21, or blind or disabled child is living in the individu-
al’s home. If the home equity exceeds the maximum
amount, individuals may use reverse mortgages or
home equity loans to reduce their total equity inter-
est in the home. Beginning in 2011, the limits on
equity will increase from year to year based on the
percentage increase in the consumer price index for
urban areas, rounded to the nearest $1,000.
57
Chapter 2: Financial Eligibility Rules and Options
Resources
Since the Primer was rst published in 2000, numerous reports and other resources have become available
on the Internet. This section includes key resources relevant to nancial eligibility for Medicaid generally
and for long-term care services specically. Most of the publications cite additional resources, and the
websites also have links to other sources of information.
Publications
Herz, E.J. (2007). CRS Report for Congress, Medicaid: A Primer. Washington, DC: Congressional Research
Service.
This report describes the basic elements of Medicaid, focusing on Federal rules governing who is eligible; what
services are covered; how the program is nanced and how beneciaries share in the cost; how providers are
paid; and the role of special waivers in expanding eligibility and modifying benets. The Decit Reduction Act
of 2005, as amended by the Tax Relief and Health Care Act of 2006, includes many provisions aecting Med-
icaid. The DRA-2005 provides states with opportunities to make fundamental changes in Medicaid program
design, including covered benets and beneciary cost-sharing. This report summarizes these and other major
DRA-2005 changes.
Available at http://aging.senate.gov/crs/medicaid1.pdf
Wood, E.F., and Klem, E.M. (2007). Protections in Medicaid Estate Recovery: Findings, Promising Practices, and
Model Notices. Washington, DC: AARP, Public Policy Institute; American Bar Association; ABA Commission
on Law and Aging.
Concentrating primarily on current state practices for clarifying Medicaid beneciary protections, this study fo-
cuses attention on promising practices and model notications that can be replicated throughout the country
for the benet of both estate recovery programs and the people aected by them. The site includes both the
full version and a brief summary of the report.
Available at http://www.aarp.org/health/medicare-insurance/info-2007/2007_07_medicaid.html
58 Understanding Medicaid Home and Community Services: A Primer
Hearne, J. (2005). CRS Report for Congress: Medicaid Eligibility for Adults and Children. Washington, DC: Con-
gressional Research Service.
This report describes Federal Medicaid eligibility rules for children and adults under age 65 but does not ad-
dress eligibility pathways for individuals qualifying on the basis of having a disability or for persons who are
age 65 or older. Also, the eligibility provisions pertain to eligibility for all Medicaid benets, not just home and
community services.
Available at http://www.chn.org/pdf/crsmedicaid.pdf
Thomson/MEDSTAT (2005). Medicaid Estate Recovery. Washington, DC: U.S. Department of Health and Hu-
man Services (HHS), Oce of Assistant Secretary for Planning and Evaluation.
This policy brief—one of six commissioned by HHS—provides an overview of state Medicaid Estate Recovery
programs, which enable states to recoup public spending from the estates of Medicaid long-term care recipi-
ents after their death. The other briefs address the following topics: Medicaid Treatment of the Home, Spouses
of Medicaid Long-Term Care Recipients, Medicaid Liens, Medicaid Estate Recovery Collections, and a case
study of the Massachusetts Medicaid Estate Recovery Program. These are available through links at the end of
the document.
Available at http://aspe.hhs.gov/daltcp/reports/estaterec.pdf
Stone, J.L. (2002). CRS Report for Congress: Medicaid Eligibility for the Aged and Disabled. Washington, DC:
Congressional Research Service.
This report describes Medicaid eligibility rules for persons with disabilities. Many in this group become eligible
because they cannot work and are dependent on welfare assistance from SSI. However, Medicaid provides
incentives for other disabled persons to work and retain Medicaid coverage.
Available at http://assets.opencrs.com/rpts/RL31413_20020705.pdf
Websites
Centers for Medicare & Medicaid Services
This site provides an overview of Medicaid eligibility (e.g., income and resource guidelines, spousal impover-
ishment, estate recovery) and includes a link to contact information for state Medicaid oces.
Web address: http://www.cms.hhs.gov/MedicaidEligibility/
The State Medicaid Manual makes available to all state Medicaid agencies informational and procedural
material needed by the states to administer the Medicaid program. The material is organized into major parts,
which are divided into chapters and sections. (Chapter 3 is about Eligibility). The manual is structured as
59
Chapter 2: Financial Eligibility Rules and Options
closely as possible to the codication of Medicaid regulations. A crosswalk of manual sections and regulations
is also included.
Web Address: http://www.cms.gov/Manuals/PBM/itemdetail.asp?lterType=none<erByDID=-99&
sortByDID=1&sortOrder=ascending&itemID=CMS021927&intNumPerPage=10
Kaiser Commission on Medicaid and the Uninsured
The Kaiser Commission on Medicaid and the Uninsured provides information and analysis on health care cov-
erage and access for the low-income population, with a special focus on Medicaid’s role and coverage of the
uninsured. The Commission is a major initiative of The Henry J. Kaiser Family Foundation and is based at the
Foundation’s Washington, DC oce.
Web address: http://www.k.org/about/kcmu.cfm
Specic information about Medicaid nancial eligibility by state using the latest Kaiser data is available at
http://www.k.org/medicaid/8048.cfm.
60 Understanding Medicaid Home and Community Services: A Primer
Endnotes: Citations, Additional Information,
and Web Addresses
1
Letty Carpenter is the original author of this chapter. Ernest McKenney and Janet O’Keee updated the
chapter.
2
This Primer uses person-rst language when referring to persons with disabilities and elderly persons,
unless referring to the specic language used in statutes, regulations, or programs, as in this instance.
3
Additional information about the Medicare program can be obtained from the CMS website at http://
www.cms.gov/home/medicare.asp.
4
The amount of monthly earnings considered as SGA depends on the nature of a person’s disability.
The Social Security Act species a higher SGA amount for statutorily blind individuals ($1,640 per
month in 2010); Federal regulations specify a lower SGA amount for non-blind individuals ($1,000 per
month in 2010). Both SGA amounts generally increase with increases in the national average wage
index. Additional information is available at http://www.ssa.gov/OACT/COLA/sga.html.
5
State Medicaid Director Letter, April 9, 2010 at http://www.cms.gov/smdl/downloads/SMD10005.PDF.
6
Subclauses (I)–(VII) of §1902(a)(10)(A)(i) of the Social Security Act.
7
As amended by §2001(c) of the Aordable Care Act.
8
Benchmark rules apply to the new group whether or not the state has otherwise elected the option
to provide benchmark benet coverage under its State Plan. Individuals in the new group who are
exempt from mandatory enrollment in a benchmark benet plan must receive medical assistance
under the state’s currently approved plan. Others must be provided with benchmark or benchmark-
equivalent coverage, including Secretary-approved benchmark coverage described in §1937(b)(1)(D).
Consistent with the provisions of §1937, children covered under the new group must receive all Early
and Periodic Screening, Diagnostic, and Treatment services.
9
If individuals have only work earnings (i.e., they do not have any unearned income), and they do not
pay for any work expenses, they can earn up to $1,433 per month in 2010 before their SSI federal cash
payments stop. Additional information is available at http://ssa-custhelp.ssa.gov/cgi-bin/ssa.cfg/php/
enduser/std_alp.php?p_sid=n6qe7NWj.
10
See Endnote 4.
11
Section 1902(r)(2) of the Social Security Act.
12
This limitation applies only to income and only to certain optional eligibility groups. There are no such
limits on using §1902(r)(2) to liberalize rules for resources.
13
Under §1902(r)(2) of the Social Security Act, a state can elect to disregard more generous amounts.
Note: For the rst time since the poverty guidelines began to be issued in 1965, the annual average
Consumer Price Index has decreased from the gure for the previous year. Therefore, the Department

61
Chapter 2: Financial Eligibility Rules and Options
of Health and Human Services poverty guidelines have been frozen until at least May 31, 2010 at
2009 levels in order to prevent a reduction in eligibility for certain means-tested programs, including
Medicaid, Supplemental Nutrition Assistance Program, and child nutrition. Additional information is
available at http://aspe.hhs.gov/poverty/09extension.shtml.
14
This provision applies to §209(b) states as well, which cannot use more restrictive eligibility criteria for
this group.
15
States can use higher levels or additional disregards under the §1902(r)(2) exception.
16
Typically this is every month. In some states it is every 6 months. But in the latter case, the person must
be able to spend down an amount that equals six times their monthly “excess” income before becom-
ing eligible.
17
State-by-state information concerning supplements for SSI beneciaries may be found in State Assis-
tance Programs for SSI Recipients, January 2009. (Released October 2009). Social Security Administra-
tion, Oce of Policy, Oce of Research, Evaluation, and Statistics. Available from Social Security Online
at http://www.ssa.gov/policy/docs/progdesc/ssi_st_asst/2009/.
18
Under §1902(r)(2), described above.
19
Whether or not the income is counted depends on the specic nature of the transaction; for example,
who the payment goes to and what the funds are used to purchase, as determined by additional Med-
icaid rules.
20
A recent state survey found that of 43 states (7 did not respond), 19 allow Miller Trusts for institutional-
ized individuals. Of the 7 states that did not respond, based on 2000 data, 1 allows Miller Trusts; this
adds up to 20 states. For states that use the 300 percent rule for HCBS waivers, of the 43 states that
responded, 18 allow Miller Trusts. Of the 7 states that did not respond, based on 2000 data, 1 allows
Miller Trusts, this adds up to 19 states. Lina Walker, AARP Public Policy Institute. Personal communica-
tion, March 24, 2010.
21
Post-eligibility rules apply to all individuals in institutions, regardless of their eligibility group.
22 Post-eligibility share-of-cost rules also apply to persons in ICFs/ID, long-term hospitals, and other med-
ical institutions, regardless of eligibility category. Persons who become eligible by meeting a medically
needy spend-down obligation also face an additional post-eligibility share-of-cost obligation based
on their remaining income.
23
This description is condensed from the analysis provided by Coey, G. (January 2010). The Medicaid
Long-Term Services and Supports Provisions in the Senate’s Patient Protection and Aordable Care
Act.
24
In 1990, the Supreme Court ruled in Sullivan vs. Zebley, that in order to meet the standard of equal
treatment, the initial disability determination process for children must include a functional limitation
component just as it is used for adults. The decision in the case that successfully contested the 1996
denitional change became moot in 1997, when §4913 of the Balanced Budget Act of 1996 (P.L. 105-
33) restored Medicaid to the children who had lost eligibility under SSI’s 1996 denitional change. See
http://www.dhs.state.or.us/spd/tools/crew/blitz/protected/Protected-HO.pdf.
25
States may also use more liberal rules, such as not counting the parents’ income and resources under
§1902(r)(2).

62 Understanding Medicaid Home and Community Services: A Primer
26
This dierential treatment comes about because SSI treats persons living in an institution as a separate
household and eligibility unit than their family members. The §209(b) states are exceptions in that
they continue to deem, even for persons who live in institutions.
27
The Tax Equity and Fiscal Responsibility Act of 1982, P.L. No. 97-248, 96 Stat. 324 (September 3, 1982).
28
Section 1619 and, equivalently, §1905(q) of the Social Security Act.
29
The amount of the SSI benet is decreased as earnings increase over the allowable amount. The
Social Security Administration has published a rule to adjust the SGA level automatically each year for
individuals with impairments other than blindness. The adjustment is based on any increase in the
national average wage index. See http://www.ssa.gov/OACT/COLA/sgadet.html.
30
Section 1619(b).
31
Numbers from “Quarterly Report on SSI Disabled Workers and Work Incentive Provisions” (September
1999), Social Security Administration, Oce of Research, Evaluation, and Statistics.
32
Numbers from “SSI Disabled Recipients Who Work, 2008,” available from Social Security Online at
http://www.ssa.gov/policy/docs/statcomps/ssi_asr/2008/sect07.html#table44.
33
The 1997 provision is in §4733 of the Balanced Budget Act of 1997 (P.L. 105-33). The 1999 provision is
in §201 of the Ticket to Work and Work Incentives Improvement Act of 1999 (P.L. 106-170).
34
States are not permitted to use §1902(r)(2), described above, as a way to get to a higher eective
income level at which full premiums are charged.
35
This includes §209(b) states.
36
The penalty for resource transfers in SSI, enacted in P.L. 106-169, is a loss of SSI benets for a period of
time. If the Social Security Administration nds that resources were transferred for less than fair market
value in the 36 months prior to application, then a penalty period begins in the month the transfer
occurred. The duration in months is calculated by dividing the amount transferred by the maximum
monthly cash benet otherwise payable.
37
The period is 60 months if assets were transferred into or out of certain trusts.
38
Social Security Act, §1917(c)(2)(iii) and (iv).
39
Unused assets in the trust must revert to the state on the death of the individual, up to the total Med-
icaid amount spent on the individual’s behalf.
40
The penalty does not apply to individuals who are eligible for HCBS waiver programs under commu-
nity nancial eligibility rules.
41
The look-back period begins on the date someone applies for Medicaid. The penalty period begins on
the date the person becomes eligible for Medicaid, not the date of application.In many instances they
are the same date.

Chapter 3: Determining Service Eligibility
63
Guide to Chapter 3
Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 65
Service Criteria: General Considerations. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .65
Home Health Services . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 67
Misperceptions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 67
Addressing Cost Concerns . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 70
Ensuring Correct Application of Eligibility Criteria . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 70
Personal Care Benet. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 70
HCBS Waiver Programs . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 72
Misperceptions About Medical Bias in Nursing Facility Service Criteria . . . . . . . . . . . . . . . . . . . 75
HCBS State Plan Benet . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 77
Community First Choice Option . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 78
Major Considerations in Setting Service Criteria: A Recap . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 78
Resources. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .79
Endnotes: Citations, Additional Information, and Web Addresses . . . . . . . . . . . . . . . . . . . . . . . . 82
65
Chapter 3: Determining Service Eligibility
Chapter 3
Determining Service Eligibility
In addition to categorical and nancial eligibility criteria required by Federal Medicaid law, states set ad-
ditional eligibility criteria to determine who in the large group that is nancially eligible and entitled to
benets is eligible to receive specic services, such as nursing home, home health, or personal care. These
criteria are based on need and can include an assessment of medical/nursing needs, health and health-
related needs, functional limitations, and/or other factors. The goal of these eligibility criteria is twofold:
to dene medical necessity and to manage overall utilization. This chapter discusses Federal provisions for
determining eligibility for four major Medicaid benets: the mandatory Home Health benet, the Personal
Care benet, home and community-based services (HCBS) waiver programs, and the State Plan HCBS
option (under the Section [§]1915(i) authority). It also discusses factors for states to consider when setting
these criteria.
1
Introduction
Federal law and regulation specify the general eligibility and coverage requirements for mandatory and op-
tional Medicaid home and community services. States use additional criteria to specify who, within the general
eligibility group, will receive services. States use a number of dierent terms to describe these criteria: medical
necessity criteria, health and functional criteria, level-of-care criteria, and service criteria. These terms are often
used interchangeably, but, in fact, may have specic meanings in state usage, which may dier from usage
in Federal requirements. When referring to any of these criteria, this Primer uses the term service criteria. The
degree of exibility states have in setting these criteria depends on whether the service is Federally mandated
or a state option and, if optional, whether it is oered under the State Plan or through a waiver program.
Service Criteria: General Considerations
The purpose of service criteria is to dene medical necessity and to manage overall utilization. Controlling uti-
lization is typically understood to mean placing limits on either the number of times a service may be provid-
ed, or the period over which it can be provided, for a given condition.
2
For a Federally mandated service, such
as Home Health, states are required to dene the service in the State Plan and may specify reasonable limita-
tions to the dened service. States also develop the process by which they determine an individual’s medical
necessity for a service, a process which is not contained in the State Plan and about which the Centers for
Medicare & Medicaid Services (CMS) has historically issued little guidance. Some states have included medical
necessity criteria in their State Plan, but these are considered by CMS to be part of the denition of reasonable
limitations.
These Federal requirements allow states considerable exibility, because reasonable limitations and medical
necessity are not dened further in Federal law or regulation (although limitations must be approved by CMS
in the State Plan). States often interpret the medical necessity criterion to mean that pre-authorization by a
medical professional is needed. But medically necessary services do not have to be medical services, that is,
services provided by licensed medical personnel; they may be services and supports provided by personal
assistants or home health aides to address functional needs. (See discussion of medical necessity under the
heading Misperceptions, later in this chapter.)

66 Understanding Medicaid Home and Community Services: A Primer
Service criteria generally include some measures of
functioning, such as the ability to perform activities
of daily living (ADLs) and instrumental activities of
daily living (IADLs) without assistance. ADLs include
eating, bathing, dressing, toileting, transferring
(e.g., from a bed to a chair), and maintaining con-
tinence. IADLs include medication management,
money management, light housework, laundry,
meal preparation, transportation, grocery shopping,
and using the telephone.
3
While IADL performance
requires higher cognitive functioning than does
ADL performance, assistants who provide help with
IADLS, other than medication and money manage-
ment, generally need less training than those who
provide help with ADLs. This is particularly true
when ADL assistance requires tasks covered by a
Nurse Practice Act, such as tube feeding.
4
Optional benets provided under the State Plan,
such as personal care services, carry no Federal
statutory or regulatory provisions regarding the
type or level of impairment a person must have to
receive benets. The only Federal rule for optional
benets is that the state must make the service
equally available to all beneciaries who satisfy the
service criteria that the state sets as dened and
limited in the State Plan.
States are permitted to choose the measures they
use to assess the particular level and/or combina-
tion of needs a person must have to be eligible. A
state may require a person to have 2 out of 5 ADL
impairments or 4 out of 12 ADL and IADL impair-
ments. This exibility has resulted in considerable
variation in the service criteria for states’ Personal
Care programs.
Determining Medical Necessity
Examples of questions that could be relevant in
determining medical necessity include
1. Relation to medical condition: Is the ser-
vice required to identify, diagnose, treat,
correct, cure, ameliorate, palliate, or pre-
vent a disease, illness, injury, disability, or
other medical condition, or is the service
required to assist an individual to perform
activities of daily living?
2. Medical reason for treatment: Is the service
provided for medical reasons rather than
primarily for the convenience of the ben-
eciary, caregiver, or provider?
3. Clinical appropriateness: Is the service
consistent—in terms of amount, scope,
and duration— with generally accepted
standards of good medical practice?
4. Medical need for choice among alternate
settings: Is the service aording treatment
generally provided to similarly situated
individuals in the setting, or is there an
alternate available setting where, under
generally accepted standards of good
medical practice, the same service may be
safely and eectively provided? This ques-
tion would not apply where Medicaid or
the Americans with Disabilities Act require
that the beneciary have a choice among
alternate settings.
Source: CMS Oce of Counsel.
Designing Medicaid service criteria can be a major
challenge for states, because competing policy ob-
jectives are involved. On the one hand, states want
to ensure that service criteria identify all individu-
als who have a legitimate need for assistance. On
the other hand, states must operate their Medicaid
programs in accord with their budgets. Because the
number of people served is a major determinant of
program costs, setting service criteria is a key nan-
cial decision.
Setting service criteria based on a trade-o be-
tween coverage and costs can have unintended
eects on other parts of the long-term care system.
67
Chapter 3: Determining Service Eligibility
For example, because nursing homes are expensive,
a state may establish stringent level-of-care criteria
for Medicaid coverage. Although, the provision of
home and community services through an HCBS
waiver program can be considerably less expensive,
Federal law requires that states use the same level-
of-care criteria for nursing homes and HCBS waiver
programs. Thus, stringent institutional criteria can
be an obstacle to serving people through HCBS
waivers, because some people who meet the crite-
ria may be too impaired to be cared for safely and
cost-eectively in the community unless they have
extensive informal help. Very stringent service crite-
ria may also result in premature institutionalization,
if informal care networks “burn out” because paid
assistance is not available until a person becomes
severely impaired.
Alternatively, states may decide they would rather
serve more people and control utilization (and
therefore costs) by limiting the amount of services
provided and reimbursement rates. The problem
here is that the more restrictions the state imposes
on the amount, scope, and duration of services, the
more likely it is that people with signicant needs
will be inadequately served in the community and
end up in an institution at a greater cost to the state.
Such trade-os suggest that there is no “correct”
decision regarding service criteria. An approach that
is appropriate in one state may not work in another.
This underscores the need to make decisions about
service criteria within the broader context of a
state’s long-term care system—which includes both
institutional and home and community services
and, with respect to the latter, several alternative
funding streams.
States use various approaches to ensure that a
program’s service criteria not only match the policy
goals for that program but also t with and meet
the goals of the larger long-term care system.
Several states do so by using an assessment process
that starts with an eligibility determination for the
highest level of need—nursing facility/waiver ser-
vices. If applicants do not meet the nursing facility
level-of-care criteria, they are then considered for
other long-term care programs that have progres-
sively lower need requirements. The waiver program
may require three ADL limitations, for example, but
the Medi caid Personal Care program may require
only two, and a state-funded program for those not
eligible for Medicaid may require only one ADL plus
one IADL impairment.
The remainder of this chapter provides information
about Federal provisions related to the selection
of service criteria for four Medicaid benets: Home
Health, Personal Care, HCBS waivers, and State Plan
HCBS. The rst three benets account for the vast
majority of Medicaid spending on home and com-
munity services; State Plan HCBS became an option
in 2007. (See Chapter 4 for a more detailed descrip-
tion of these service options.) While the same or
similar services may be covered by all three benets
(e.g., assistance with ADLs), states have more ex-
ibility when dening service criteria for optional
than for mandatory benets.
Home Health Services
Home health services are a mandatory benet for all
individuals entitled to nursing facility care under a
state’s Medicaid State Plan—that is, for categorically
eligible persons age 21 or older. If a state chooses
to cover nursing facility care for younger persons,
or for the medically needy, home health services
become mandatory for these groups as well.6
To receive home health services, Federal regulations
specify that the services must be ordered by a phy-
sician as part of a written plan of care. Beyond this
authorization procedure, and the general require-
ment that services be medically necessary, there are
no additional Federal requirements.
Misperceptions
Despite the unambiguous nature of Federal cover-
age and eligibility requirements, misperceptions
that additional Federal requirements further restrict
who may receive home health services are com-
mon. The rst misperception is that individuals
must be eligible for nursing facility care in order to
receive home health services (i.e., that they must
meet a state’s nursing facility level-of-care criteria).
This misunderstanding has arisen because the word
68 Understanding Medicaid Home and Community Services: A Primer
entitled to nursing facility care has been interpreted
to mean eligible for nursing facility care. The Federal
requirement species the coverage groups entitled
to the Home Health benet. Those entitled include
(a)categorically eligible persons age 21 or over,
(b)persons under age 21 if the State Plan provides
nursing facility services for them, and (c)medically
needy persons if the State Plan provides nursing
facility services for them. It also states clearly that
eligibility does not depend on the need for institu-
tional care or for skilled nursing or therapy services.
Additionally, even if the state does not cover per-
sons under age 21, the Early Periodic Screening,
Diagnosis, and Treatment mandate requires that
home health services be provided to this group if
they are needed.
A second misperception is that states must use Fed-
eral eligibility requirements for the Medicare Home
Health benet to determine eligibility for the Medic-
aid Home Health benet. In particular, many incor-
rectly believe that to be eligible for Medicaid home
health services, a person has to meet the Medicare
home-bound requirement and need skilled nurs-
ing or therapy services. In fact, states may not limit
Medicaid home health services to individuals who
require skilled services as dened by Medicare (i.e.,
skilled nursing and therapy services).
6
Additionally, while Federal regulations state that
home health services must be provided in the
home, there is no requirement that beneciaries
be homebound. A July 2000 State Medicaid Direc-
tor Letter claries that a homebound requirement
violates Medicaid comparability requirements.
7
While Medicaid home health services must be pro-
vided by a Medicare-certied home health agency,
this requirement is a provider qualication; it does
not create an eligibility linkage between the two
programs. Federal Medicaid policy permits states
to provide home health services to persons with a
wider range of needs than is possible through the
Medicare program.
Federal Coverage and Eligibility
Requirements for Medicaid
Home Health Services
Mandatory State Plan home health services are
(a)nursing services provided on a part-time or
intermittent basis by a home health agency that
meets requirements for participation in Medi-
care; (b)home health aide services provided by
a home health agency that meets requirements
for participation in Medicare; and (c)medical
supplies, equipment, and appliances suitable for
use in the home.
• The optional home health services are
physical therapy, occupational therapy,
speech pathology, and audiology services.
• Services must be ordered by a physician
as part of a written plan of care that the
physician reviews every 60 days.8
• Once a state denes its Home Health ben-
et—whether it includes only mandatory
home health services or both mandatory
and optional services—the benet must
be available to all Medicaid beneciaries
entitled to nursing facility services under
the State Plan.
• States may place coverage limits on home
health services if the limits are based on
considerations related to medical neces-
sity or utilization control.
• Eligibility of beneciaries to receive home
health services does not depend on their
need for, or discharge from, institutional
care, or their need for skilled nursing or
therapy services.
69
Chapter 3: Determining Service Eligibility
Provision of Services Outside a Beneciary’s Home
A Connecticut lawsuit—Skubel v. Fuoroli—challenged CMS’s regulation requiring that Medicaid home health care
services be provided exclusively in a beneciary’s place of residence. The lawsuit focused on the receipt of nurs-
ing services outside the home.
In 1997, the Court of Appeals ruled that the Medicaid statute is ambiguous with respect to whether home
health care services must be provided exclusively at the recipient’s residence.
9
Specically, the court ruled that
“the Medicaid statute neither allows nor prohibits reimbursement for home health services outside the recipi-
ent’s residence. The statute merely provides that states may include ‘home health care services’ in their Medicaid
programs.
10
It does not dene home health care services, and though the statute implies that the services will
normally be rendered in the home, neither the context of the provision nor the structure of the statute indicates
whether the home is the exclusive locus of the necessary services.”
The court went on to hold that “the regulation as written is invalid,” because the restriction of home health care
services to a beneciary’s residence “ignores the consensus among health care professionals that community
access is not only possible but desirable for disabled individuals.” The court further stated that the assumptions
behind the restriction of services to the beneciary’s residence were medically obsolete, and that “the technol-
ogy and knowledge now exist to allow many people with disabilities, elderly or not, to venture into the commu-
nity, where before they would have been considered permanently homebound.”
To ensure that the ruling would not result in increased costs for the state, the court expressly limited benecia-
ries of Medicaid-covered home health nursing services to the number of hours of services to which they would
be entitled if the services were provided exclusively at the recipient’s place of residence.
11

70 Understanding Medicaid Home and Community Services: A Primer
Addressing Cost Concerns
States can address concerns about the cost of the
Home Health benet without using the impermis-
sible homebound criterion. For example, states may
establish criteria to determine who needs the ser-
vice based on medical necessity, criteria which take
account of beneciaries’ unique needs, as described
in the following examples.
When a condition—such as quadriplegia—prevents
individuals from going to another health care set-
ting to obtain the service.
When going to an outpatient setting for the ser-
vice would constitute a medical hardship due to
an individual’s condition, or is contraindicated by a
documented medical condition, such as the need to
be protected from exposure to infections.
When going to an outpatient setting for the ser-
vice would interfere with the eectiveness of the
service. Examples include (1)when hours of travel
would be required; (2)when services are needed
at a frequency that makes travel extremely dif-
cult, such as IV care three times a day; (3)when
a client needs re gular and unscheduled catheter
changes, and having home health services in place
will prevent emergency room visits for unscheduled
catheter changes due to blockage or dislodgment;
and (4)when there is a history of noncompliance
with outpatient services that has led to adverse
consequences, including emergency room use and
hospital admissions.
12
States can also control costs for the Home Health
benet by limiting the amount, scope, and dura-
tion of the services provided—as long as all services
listed in the State Plan are sucient to meet the
needs of most persons who need the services. The
State Plan must include a list of services that will
be provided, as well as their amount, scope, and
duration. For example, some states limit the number
and duration of daily home health aide visits, and
preauthorization is required to exceed these limits.
Other states require preauthorization for all services
to ensure appropriateness.
The appropriate context for making decisions about
limits on a state’s Home Health benet is the state’s
entire system of home and community services. A
state may opt to cover registered nurse and home
health aide visits through the Home Health benet,
for example, and not through a waiver program to
ensure that all beneciaries who need these ser-
vices receive them, not just those who meet the
nursing home level-of-care criteria. However, if a
state uses institutional rules for the waiver program,
doing so will limit services under the Home Health
benet to those who meet the stricter nancial
eligibility criteria for State Plan services.
Ensuring Correct Application of
Eligibility Criteria
States contracting with private managed care
organizations to provide the Medicaid Home Health
benet must specify in their managed care con-
tracts who will determine eligibility for the benet
and what service criteria will be used. Clear and
precise terms are crucial. Eligibility criteria that are
framed in very general terms—medical necessity,
for example—can be interpreted very dierently
in a managed health care plan that customarily
provides primary and acute health care benets but
not long-term care services.
Home health services can be provided as acute,
post-acute, and/or long-term care services. If a state
has an HCBS waiver program administered, for ex-
ample, by an Area Agency on Aging, but the state’s
capitated health programs control the Home Health
benet, the two systems will need to collaborate to
ensure that individuals entitled to and eligible for
home health services receive them.
Personal Care Benet
Personal care services provided through the State
Plan are an optional benet. When personal care
services were rst authorized in the mid-1970s, they
had to be prescribed by a physician in accordance
with a treatment plan. In 1993, Congress removed
the requirement for physician authorization and
gave states the option to use other methods to
authorize the benet in accordance with a state-
approved service plan. There are no other Federal

71
Chapter 3: Determining Service Eligibility
statutory or regulatory requirements regarding
eligibility for services. Within the broad parameters
of the Federal denition of personal care services,
states are free to determine service criteria as well
as the amount, scope, and duration of the services.
The State Medicaid Manual denition of personal
care services provides the primary guidance for
establishing these criteria:
Personal care services . . . may include a range of hu-
man assistance provided to persons with disabilities
and chronic conditions of all ages, which enables
them to accomplish tasks they would normally do
for themselves if they did not have a disability. As-
sistance may be in the form of hands-on assistance
(actually performing a personal care task for a per-
son) or cueing so that the person performs the task
by him/herself. Such assistance most often relates to
performance of activities of daily living (ADLs) and
instrumental activities of daily living (IADLs).
13
The Manual also states that people with cognitive
impairments can be oered services through the
Personal Care option:
An individual may be physically capable of perform-
ing ADLs and IADLs but may have limitations in
performing these activities because of a cognitive
impairment. Personal care services may be required
because a cognitive impairment prevents an indi-
vidual from knowing when or how to carry out the
task. For example, an individual may no longer be
able to dress without someone to cue him or her on
how to do so. In such cases, personal assistance may
include cueing along with supervision to ensure
that the individual performs the task properly.
14
Given the Federal Medicaid denition of personal
assistance, service criteria should be based on a
need for assistance with ADLs or with IADLs. There
is a considerable body of research on ADLs and
IADLs to guide states in designing their service
criteria. Generally, ADLs are more frequently used
than IADLs to determine service eligibility, because
they are widely believed to measure a greater level
of need. But research indicates that dependencies
in multiple IADLs also indicate a high level of need
(e.g., the inability to use the telephone actually indi-
cates a very high level of impairment).
15
Limitations
in performing other IADLs, such as meal preparation
and medication management, may actually pose a
greater health risk than an ADL limitation in bathing
and dressing. A number of states use both ADLs and
IADLs in their service criteria.
An important consideration when selecting ser-
vice criteria is that the level of impairment a state
requires for eligibility matches the services avail-
able. For example, if a state requires applicants to be
severely impaired, the maximum number of service
hours permitted should be sucient to enable
them to remain in the community. It is also impor-
tant to ensure that assessment methodologies do
not inadvertently exclude certain groups, such as
persons with dementia. For example, if the eligibility
criteria require that an individual needs “hands-on”
assistance with ADLs, a person who needs cueing
and supervision to perform ADLs will be excluded.
In eect, states have a very high level of discretion
when determining who will receive personal care
services through the State Plan. However, states
may not violate Medicaid comparability require-
ments by restricting services to those with a par-
ticular diagnosis or condition.
Given that personal care services are subject to Fed-
eral statewideness and comparability requirements,
states understandably have cost concerns about
increasing access to these services through the use
of liberal service criteria. As mentioned, there is no
“correct” decision regarding service criteria. Wheth-
er or not particular service criteria are appropriate
and make sense depends on the broader context
of a state’s policy goals for its entire long-term care
system (i.e., whether the criteria t logically into the
overall plan for providing services to people with
long-term care needs through multiple programs).
72 Understanding Medicaid Home and Community Services: A Primer
The Comparability Requirement
With few exceptions (such as the targeted case
management benet), service criteria for any
State Plan benet—mandatory or optional—are
subject to the “comparability” requirement. Un-
der this requirement, services must be available
on a comparable basis to all Medicaid benecia-
ries in an eligibility group in the state who need
the service; that is, the State Plan may not oer
a service only to persons who have a particular
condition or oer it in dierent forms to dierent
groups.
16
Additionally, states must use the same
eligibility criteria for all applicants, and any limits
on service amount, scope, and duration must be
applied equally to individuals currently receiving
services and those applying for services.
The eect of these requirements is that states
cannot have service criteria that target particular
groups of people by diagnosis, or condition (e.g.,
requiring that individuals have a spinal cord
injury). Additionally, any changes made in the
service criteria—and in the amount, scope, and
duration of service—must be applied equally to
those currently receiving services and those ap-
plying for them. These provisions constitute the
“comparability” requirement. HCBS waivers are
not State Plan services and not subject to this
requirement—they “waive” comparability.
The Statewideness Requirement
States cannot restrict the availability of State
Plan services to particular geographic regions.
Some states design programs funded only with
state dollars to provide services for people who do
not meet Medicaid’s eligibility criteria but none-
theless need services. For example, the goal of the
Connecticut Home Care Program for Elders is to
avoid institutionalization of frail individuals age 65
or older. The program includes both a state-funded
component and a Medicaid waiver component. Be-
cause many individuals who need services to avoid
nursing home placement do not meet Medicaid’s
nancial eligibility criteria and/or the waiver’s level-
of-care criteria waiver, this population is served in
the state program, which has less stringent nancial
and service eligibility criteria than does the waiver
program.
HCBS Waiver Programs
Under HCBS waiver programs, states are permitted
to waive Federal comparability and statewideness
requirements in order to provide home and com-
munity services to people who would otherwise
require an institutional level of care reimbursable by
Medicaid.
To be eligible for waiver services, individuals must
rst meet a waiver’s targeting criteria, such as age
and diagnosis or condition. A state may have a
number of waiver programs targeting dierent
groups: people age 65 or older, those age 18 to 64
with physical disabilities, children who are technol-
ogy dependent, persons with intellectual disabilities
and other developmental disabilities (hereafter
referred to as developmental disabilities), persons
with AIDS, and persons with traumatic brain injury.
Individuals who meet the targeting criteria must
then meet service criteria, which for HCBS waiver
programs are the level-of-care criteria states use
to determine eligibility for either a hospital, nurs-
ing facility, or intermediate care facility for persons
with intellectual disabilities (ICF/ID)—also called
institutional criteria.
17
Level-of-care criteria explicitly
describe the type and level (or severity) of function-
al limitations and/or medical and nursing needs an
individual must have to be admitted to an institu-
tional setting.
73
Chapter 3: Determining Service Eligibility
Illustrative Service Criteria for Personal Care Services: State Examples
Arkansas. To be eligible for State Plan Personal Care services, a person must have physical dependency needs
and require assistance performing the following tasks and routines: eating, bathing, dressing, personal hygiene,
bladder and bowel requirements, taking medications, laundry, incidental housekeeping, and shopping for per-
sonal maintenance items.
Texas. To be eligible for State Plan Personal Care services, the applicant/client must
1. Meet the minimum functional need criteria as set by the department. The department uses a standard ized
assessment instrument to measure the client’s ability to perform activities of daily living. This yields a score,
which is a measure of the client’s level of functional need. The department sets the minimum required
score for a client to be eligible, which the department may periodically adjust commensurate with available
funding.
2. Have a medical need for assistance with personal care:
• the individual’s medical condition must be the cause of the individual’s functional impairment in per-
forming personal care tasks;
• persons diagnosed with mental illness and intellectual disability, or both, are not considered to have an
established medical need based solely on such diagnosis. The diagnoses do not disqualify an individual
for eligibility as long as the individual’s functional impairment is related to a coexisting medical condi-
tion;
• have a signed and dated practitioner’s statement that includes a statement that the individual has a cur-
rent medical need for assistance with personal care tasks and other activities of daily living.
3. Require at least 6 hours of service per week. An applicant/individual requiring fewer than 6 hours of service
per week may be eligible if the applicant/individual meets one of the following criteria:
• requires primary home care or community attendant services to provide respite care to the caregiver;
• lives in the same household as another individual receiving primary home care, community attendant
services, family care, or Community Based Alternatives personal assistance services;
• receives one or more of the following services (through the department or other resources):
i. congregate or home-delivered meals,
ii. assistance with activities of daily living from a home health aide,
iii. day activity and health services, or
iv. special services to persons with disabilities in adult day care.
• receives aid-and-attendance benets from the Veterans Administration;
• receives services through the department’s In-home and Family Support Program;
• receives services through the Medically Dependent Children Program; or
• is determined, based upon the functional assessment, to be at high risk of institutionalization without
primary home care or community attendant care services.
74 Understanding Medicaid Home and Community Services: A Primer
These criteria usually include measures of the need
for nursing and medically-related services and for
assistance with ADLs. A determination that a person
meets the required level-of-care criteria is based on
information gathered through a formal assessment
process carried out when an individual applies for
services. In the case of ICF/ID services, applicants
must have an intellectual disability or a “related”
condition, and be found to need various supports
necessary to maintain or improve functioning.
18
In
the case of nursing facility services, the need for
skilled and unskilled nursing care is generally as-
sessed, as is the need for assistance with ADLs and
other aspects of functioning.
The Federal requirement that states use the same
or equivalent service criteria for waiver services that
they use for institutional placement stems from
the waiver program’s primary purpose: to oer an
alternative to institutionalization.
19
This statutory
requirement was added by Congress in part to ad-
dress concern about the cost of expanding home
and community services: states must demonstrate
that they are providing waiver services only to
people who are eligible for institutional placement.
CMS cannot waive this requirement or lessen its im-
pact by regulation. Congress would have to amend
the Federal Medicaid statute to allow states to use
substantively dierent service criteria for a waiver
program than for institutional services (i.e., criteria
not based on the need for institutional services).
Level-of-Care Criteria for ICFs/ID and
HCBS Waiver Programs for People with
Developmental Disabilities
Some states use “categorical” level-of-care cri-
teria referencing specic “related conditions” by
medical diagnoses or type, such as intellectual
disability, spina bida, or autism. Other states
use “functional” criteria, such as that provided by
the Federal Developmental Disabilities Assis-
tance and Bill of Rights Act of 2000,
20
which are
based on a person’s adaptive abilities or capacity
to perform tasks at a specic level. The majority
of states, however, use a combination of the two
approaches, referencing both categorical and
functional criteria.
21
When the waiver authority was enacted in 1981,
home and community services could be provided
under a waiver program only to persons who met
the level-of-care criteria for any one of the following
institutions: a Medicaid skilled nursing facility (SNF),
an intermediate care facility (ICF) providing nurs-
ing services, an ICF/ID, or a hospital that is Medicaid
certied as a hospital but provides long-term care
services. In 1987, the Omnibus Budget Reconcilia-
tion Act eliminated the distinction between man-
datory SNFs and the optional ICFs and mandated
a new nursing facility benet, which includes the
former SNF and ICF benets.
The only Federal requirement for persons to receive
the former ICF level of care—now the minimum
level of care in a nursing facility—is a need on a
regular basis for “health-related care and services
[provided] to individuals who because of their men-
tal or physical condition require care and services,
above the level of room and board, which can be
made available to them only through institutional
facilities.”
25
Within this broad denition, states are
free to set whatever service criteria they choose for
nursing facility care, which (or their equivalent) are
then used to determine eligibility for waiver ser-
vices. States vary considerably in the stringency of
their minimum level-of-care criteria.
26
75
Chapter 3: Determining Service Eligibility
Lawsuit Related to Maryland’s
Level-of-Care Criteria
On November 30, 2007, Maryland’s Court of
Special Appeals ruled that Maryland’s standard for
determining eligibility for nursing facility services
and HCBS waiver programs—a need for constant
skilled nursing care—was stricter than allowed
under Federal law. The Court determined that
people should be eligible if they need constant
care and supervision provided by health care
aides, but not necessarily the level of care that
would require licensed or highly skilled nurses.
22
As a result of the Court’s ruling, the State devel-
oped new minimum level-of-care criteria for ap-
plicants who do not meet the criteria for a skilled
level of nursing home care. These criteria include
“a need for health-related services above the level
of room and board on a regular basis.” The State
describes such services as
• A need for hands-on assistance to adequate-
ly and safely perform two of ve ADLs—
bathing, dressing, mobility, toileting/contin-
ence, and eating—as a result of a current
medical condition or disability; or
• Supervision of an individual’s performance
of two or more ADLs for an individual with
cognitive decits, as indicated by a score of
15 or less on the Folstein Mini-Mental Status
Exam (MMSE),23 and who is in need of assis-
tance with at least three or four instrumental
activities of daily living—medication man-
agement, money management, telephone
use, and housekeeping; or
• Supervision of an individual’s performance
of two or more ADLs combined with the
need for supervision and redirection of
individuals exhibiting at least two of the
following behavior problems: wandering
several times a day; hallucinations/delusions
at least weekly; abusive/aggressive behav-
ior several times a week; disruptive/socially
inappropriate behavior several times a week;
and/or self-injurious behavior several times
a month.24
Misperceptions About Medical Bias in
Nursing Facility Service Criteria
A common criticism of nursing facility level-of-care
criteria is that they are “medically biased,” that is,
(a)they do not adequately assess functional limita-
tions and how they aect the need for long-term
care, or (b)they give greater weight to nursing and
medical needs than to functional limitations caused
by physical or mental impairments. However, no
Federal statute or regulation mandates that states
adopt such a medical approach when setting nurs-
ing facility level-of-care criteria.
The term medically necessary does not imply a
distinction between medical conditions and func-
tional limitations caused by physical or mental
impairments. The correct sense of the term is that
services need simply to be “necessary” (i.e., needed
by the individual). Determining medical necessity
is the process states use to determine whether a
specic person requires a covered service. States
must provide covered services to eligible individuals
who require them. States also make medical neces-
sity determinations to control utilization and avoid
wasting resources on unneeded services.

76 Understanding Medicaid Home and Community Services: A Primer
There is no Federal denition of medical necessity
for specic services, so states are free to dene it
broadly (e.g., medically necessary services are those
that promote optimal health and functioning). Thus,
the requirement that services be medically neces-
sary does not mean a state is required to use only
medical—or even any medical—service criteria to
determine eligibility for nursing facility services.
Oregon, for example, uses only functional criteria.
27
Nor must a state give greater weight to medical and
nursing needs than to functional needs.
No clear line separates functional from medical
needs. Health status and functioning are closely in-
terrelated; immobility due to paralysis or even frailty
can lead to serious medical problems in multiple
body systems. Thus, failure to address functional
limitations can result in serious medical prob-
lems that require not only nursing home care, but
hospitalization as well. The primary reason people
need long-term care services is because they have
functional limitations. Even if people require spe-
cialized health care (e.g., injections or catheteriza-
tion), research has shown that people can meet
these needs themselves if they are not physically or
mentally impaired. Thus, the single most important
measure of need for long-term care is a person’s
functional limitations.
Another common misperception is that a physical
illness or disability is required in order to be eligible
for Medicaid coverage of nursing facility care, rather
than assistance with ADLs or IADLs due to function-
al limitations caused by cognitive decits or mental
illness. In fact, §1915(a)(1)(C) of the Social Security
Act clearly states that while the overall facility must
not be primarily for the treatment of mental dis-
eases, a nursing facility provides health-related care
and services to individuals who because of their
physical or mental condition require, on a regular
basis, care and services (that are above the level of
room and board), which can be made available to
them only through institutional facilities. However,
a Federally required process called Preadmission
Screening and Resident Review requires states to
ensure that individuals with serious mental illness
or an intellectual disability are admitted to a nursing
facility only if the facility can meet their needs.
Another common misperception about Medicaid
level-of-care criteria is that an institutional standard
requires a severe level of medical need or functional
limitation. There is no such Federal requirement. In
addition to having criteria for a skilled level of care,
states’ nursing facility benet must include minimal
criteria that comports with the Federal denition
of the former ICF criteria: a need, on a regular basis,
for health-related care and services by individuals,
who because of their mental or physical condition,
require care and services (above the level of room
and board), which can be made available to them
only through institutional facilities.
28
However states dene their nursing home level-of-
care criteria, many people who meet those criteria
will remain in the community, even without for-
mal services. A study in Connecticut, for example,
found that some people with severe functional
limitations (three or more ADL impairments), who
met the nursing facility level-of-care criteria, chose
to go without nursing home and waiver services
rather than spend down to Medicaid eligibility or
be subject to estate recovery provisions.
29
States’
concerns about increasing the number of people
admitted to nursing facilities are understandable.
However, states can prevent unnecessary institu-
tionalization by screening people prior to nursing
facility admission to determine whether services
could be provided in home and community settings
(i.e., establish pre-admission screening or nursing
facility diversion programs). Other steps that states
can take to reduce the number of people in nurs-
ing facilities include the establishment of nursing
facility transition programs and “money follows
the person” policies to allow institutional funds to
follow nursing facility residents to home and com-
munity settings. Implementation of such programs
and policies can help to ensure that only those who
truly cannot be served safely and cost-eectively in
the community will be admitted to and remain in
nursing facilities.
30
77
Chapter 3: Determining Service Eligibility
Illustrative Use of Functional Measures to
Determine Eligibility for Nursing Facility
and Waiver Services: Oregon
Oregon’s level-of-care criteria specify 18 func-
tional levels with 1 representing the most
impaired and 18 the least impaired. The State
does not consider medical or nursing needs to
determine eligibility. The State assesses the need
for assistance with mobility (ambulation and
transferring), eating, and elimination (toileting,
bowel and bladder care), and assistance due to
impaired mental status (cognition and behav-
ior.) The denitions of ADL assistance recognize
that the need for assistance can be the result
of a physical impairment, limited endurance, or
cognitive impairment.
The State assesses mental status, with measures
of memory, orientation, adaptation to change,
awareness of needs, and judgment. Memory is
dened as the ability to remember and appro-
priately use current information, which aects
an individual’s health, safety, and welfare. Be-
haviors that may aect living arrangements and/
or jeopardize the safety of self or others are also
assessed; these include wandering, those that
pose a danger to self or others, and those that
negatively aect living arrangements, providers,
and/or others.
Threshold Eligibility Requirement. Depending
on available funding, the State sets dierent
levels as the threshold eligibility requirement. In
the past 15 years, it has varied from level 13 to
level 18.
HCBS State Plan Benet
The Decit Reduction Act of 2005 (DRA-2005)
added §1915(i) to the Social Security Act, which
allows states, at their option, to provide home and
community-based services under the Medicaid
State Plan without a waiver.
31
Section 1915(i) was
subsequently amended by the Patient Protection
and Aordable Care Act of 2010 (hereafter, the Af-
fordable Care Act).
The only Federal requirement regarding the needs-
based criteria for this optional State Plan benet is
that they be less stringent than a state’s level-of-
care criteria for institutional services, that is, nursing
facilities, ICFs/ID, and hospitals that are Medicaid
certied as hospitals but provide long-term care
services. However, if a state chooses to use the 300
percent of Supplemental Security Income nancial
eligibility criteria for this benet, to be eligible indi-
viduals must also be eligible for either a §1915(c),
(d), or (e) waiver or a §1115 waiver. For a §1915(c)
waiver, this means that individuals must meet the
level-of-care criteria for institutional services.
If the state does not have needs-based criteria as
part of its level-of-care criteria for these institutions,
the state will have to add them.
32
If a state revises its
needs-based eligibility criteria, it must continue of-
fering §1915(i) services in accordance with individu-
al service plans to participants who do not meet the
new revised needs-based criteria, but continue to
meet the former needs-based criteria, for as long as
the State Plan HCBS option is authorized.
33
Needs-Based Level-of-Care Criteria
Because minimum eligibility for the §1915(i)
benet must be set below institutional level-of-
care criteria, states may want to use this option
to serve individuals with a low level of need and
to serve only individuals with a higher level of
need in institutions and through HCBS waivers.
(However, states could choose not to set such a
ceiling, and allow individuals whose needs meet
institutional and HCBS waiver criteria to be able
to receive State Plan HCBS.)
In order to implement the State Plan HCBS
benet, states may need to add needs-based
criteria to their institutional level-of-care criteria
requirements, if none presently exist. Sec-
tion 1915(i) of the Social Security Act does not
require that such added needs-based institu-
tional level-of-care criteria necessarily result
in excluding individuals who would be served
without the added criteria. In fact, the purpose
of §1915(i) is to expand access to home and
community-based services for individuals who
are not at an institutional level of care, rather
than to reduce access to institutional and waiver
services.

78 Understanding Medicaid Home and Community Services: A Primer
Community First Choice Option
The Aordable Care Act of 2010 also establishes a
new State Plan optional benet—the Community
First Choice Option, eective October 2011.
34
The
Federal Medical Assistance Percentage rate in the
Community First Choice Option will be six percent-
age points higher than the state’s usual matching
percentage for Medicaid services. To be eligible for
services, individuals must require hands-on assis-
tance, supervision, or cueing with activities of daily
living, instrumental activities of daily living, and/
or health-related tasks. If their income exceeds 150
percent of the Federal Poverty Level, they must
meet the state’s institutional level-of-care criteria.
Major Considerations in Setting Service
Criteria: A Recap
Federal policies with respect to service criteria es-
tablish a framework within which states have wide
latitude to select service criteria that best suit their
unique long-term care service system. Three consid-
erations, in particular, should guide state choices in
setting their service criteria:
Service criteria should be developed with an eye
toward the full constellation of services and sup-
ports a state oers—both through the Medicaid
program and with other state and local resources. In
other words, criteria should not be crafted for spe-
cic programs without considering the criteria for
other long-term care service programs in the state.
The criteria should t together so that all individu-
als needing long-term care services in the state are
able to obtain the services and supports that will
meet their needs.
It is important to recognize that there is a constant
tug-and-pull among state policy aims. On the one
hand, states desire to make services and supports
broadly available. On the other hand, states must
manage their budgets. States, for example, may
sometimes impose stringent service criteria for cost
containment reasons, which then undermines their
ability to promote appropriate access. Careful man-
agement of dierent components of the benet
package and establishment of an ecient service
delivery system can help a state to work its way
between these potentially conicting objectives.
Concern that using less stringent criteria (with
respect to the institutional/waiver eligibility linkage)
will result in higher demand for—and expenditures
on—institutional services, seems to be misplaced.
Experience conrms that most individuals want to
remain in their homes and in the community. Their
ability to do so is strengthened through the provi-
sion of home and community services.
79
Chapter 3: Determining Service Eligibility
Resources
Since the Primer was rst published in 2000, numerous reports and other resources have become available
on the Internet. This section includes key resources regarding service eligibility for Medicaid long-term care
services and supports. Most of the publications cite additional resources and the websites have links to
other information sources.
Publications
Centers for Medicare & Medicaid Services. (2008). Application for a §1915(c) Home and Community-
Based Waiver [Version 3.5]: Instructions, Technical Guide and Review Criteria. Baltimore, MD: Department
of Health and Human Services.
This publication contains extensive information concerning Federal policies that apply to the operation of an
HCBS waiver, in particular, Appendix B: Participant Access and Eligibility.
Available at https://www.hcbswaivers.net/CMS/faces/portal.jsp under links and downloads, entitled §1915(c)
Waiver Application and Accompanying Materials.
Centers for Medicare & Medicaid Services. State Medicaid Director Letter. August 6, 2010. Improving Ac-
cess to Home and Community-Based Services.
The purpose of this letter is to inform states of, and provide guidance on, several changes to §1915(i) of the
Social Security Act made by the Aordable Care Act. Under §1915(i), states have the option to amend their
State Plans to provide home and community-based services without a waiver. These changes, which become
eective October 1, 2010, include revised and new §1915(i) provisions for removal of barriers to oering home
and community-based services through the Medicaid State Plan.
Available at http://www.cms.gov/smdl/downloads/SMD10015.pdfHendrickson, L., and Kyzr-Sheeley, G.
(2008). Determining Medicaid Nursing Home Eligibility: A Survey of State Level of Care Assessment. New
Brunswick, NJ: Rutgers Center for State Health Policy.
This study describes the nursing facility level-of-care determination processes for individuals applying for
Medicaid coverage of nursing home services. The Appendix provides a brief description of data each state col-
lects, the name of the assessment form, plus contact information for state sta.
Available at http://www.hcbs.org/moreInfo.php/doc/2216
80 Understanding Medicaid Home and Community Services: A Primer
Zaharia, R., and Moseley, C. (2008). State Strategies for Determining Eligibility and Level-of-Care for ICF/
MR and Waiver Program Participants. New Brunswick, NJ: Rutgers Center for State Health Policy.
This report presents the results of a survey of state developmental disabilities agency ocials regarding the
determination of initial eligibility/level of care and the “annual level of care” for services furnished under Med-
icaid waiver and ICF/MR programs. Forty-seven states provided information on state waiver eligibility criteria
and practices. The report describes state level-of-care assessment approaches and provides legislative cita-
tions and contact information for state sta.
Available at http://www.hcbs.org/moreInfo.php/doc/2305
O’Keee, J. (1999). Elderly Persons with Cognitive and Other Mental Impairments: Can They Meet Medic-
aid Level-of-Care Criteria for Nursing Homes and for Home and Community-Based Waiver Programs? Pub.
#9704, Washington, DC: AARP, Public Policy Institute.
This study investigates whether persons ages 65 or older, with functional limitations caused by cognitive and
other mental impairments, can meet states’ Medicaid level-of-care criteria for nursing home and HCBS waiver
programs. A review of 42 states’ Medicaid level-of-care criteria found that many states do not use measures
that appropriately assess the need for services among persons with cognitive and other mental impairments.
The report includes a state-by-state description of Medicaid level-of-care criteria relevant for persons with
cognitive and other mental impairments. To obtain a free copy of this document, contact AARP’s Public Policy
Institute at (202) 434-3840.
Note: Although this and the following publication are more than 10 years old, more recent reports with this level of
detail are not available.
O’Keee, J. (1996). Determining the Need for Long-Term Care Services: An Analysis of Health and Function-
al Eligibility Criteria in Medicaid Home and Community-Based Waiver Programs. Pub. #9617, Washington,
DC: AARP, Public Policy Institute.
This report provides, through text and tables, an overview and comparison of the criteria that 42 states use
to determine eligibility for nursing home and HCBS waiver programs. To obtain a free copy of this document,
contact AARP’s Public Policy Institute at (202) 434-3840.
81
Chapter 3: Determining Service Eligibility
Websites
Centers for Medicare & Medicaid Services
Overview of Preadmission Screening and Resident Review (PASRR). Federal law requires that a Medicaid-cer-
tied nursing facility may not admit an applicant with serious mental illness (SMI), an intellectual disability (ID),
or a related condition, unless the individual is properly screened, thoroughly evaluated, found to be appropri-
ate for nursing facility placement, and will receive all specialized services necessary to meet the individual’s
unique SMI/ID-related needs. Nursing facility residents with SMI or ID must have a Resident Review when there
is a signicant change in the resident’s physical or mental condition. CMS requires each state and territory to
specify the PASRR program in their Medicaid State Plan.
Web address: http://www.cms.hhs.gov/pasrr/
The State Medicaid Manual. This manual makes available to all state Medicaid agencies, in a form suitable for
ready reference, informational and procedural material needed by states to administer the Medicaid program.
The manual provides instructions, regulatory citations, and information for implementing provisions of Title
XIX of the Social Security Act. Instructions are ocial interpretations of the law and regulations, and, as such,
are binding on Medicaid state agencies. The material is organized into major parts, which are divided into
chapters and sections. The manual is structured as closely as possible to the codication of Medicaid regula-
tions. A crosswalk of manual sections and regulations is also included.
Web address: http://www.cms.hhs.gov/Manuals/PBM/itemdetail.asp?lterType=none<erByDID=-99&sortBy
DID=1&sortOrder=ascending&itemID=CMS021927&intNumPerPage=10
82 Understanding Medicaid Home and Community Services: A Primer
Endnotes: Citations, Additional Information,
and Web Addresses
1
Janet O’Keee and Gary Smith co-authored the original chapter. Janet O’Keee updated the chapter.
2
States may make provision for “outliers”—those individuals whose condition responds less well than expect-
ed for their condition, and who, as a consequence, may receive more services for a longer period.
3
The ADL and IADL scales are based on a developmental model: children learn to eat, toilet, bathe, and dress
themselves before they develop the mental ability to do more cognitively complex activities such as us-
ing the telephone and managing money. When cognitive abilities start to deteriorate (as in a person who
develops dementia) the ability to perform activities that require more complex mental functioning (IADLs)
is generally lost before the ability to perform ADLs. States are not bound by the denitions implied by this
developmental model; they can, for example, dene ADLs to include whatever tasks/activities they consider
important to determine a need for long-term care.
4
People who work with individuals who have cognitive impairments or behavior issues need specialized train-
ing.
5
Section 1902(a)(10)(d) of the Social Security Act.
6
42 CFR 440.230(c) and 42 CFR 440.240.
7
State Medicaid Director Letter, July 25, 2000. Available at http://www.cms.hhs.gov/smdl/downloads/
smd072500b.pdf.
8
The frequency of further physician review of a beneciary’s continuing need for medical equipment and sup-
plies is determined on a case-by-case basis, based on the nature of the item prescribed.
9
Skubel v. Fuoroli. (No. 96-6201). United States Court of Appeals, Second Circuit. Decided May 13, 1997. Ruling
available at http://openjurist.org/113/f3d/330.
10
42 U.S.C. §1396d(a)(7). When Medicaid was rst enacted in 1965, coverage of home health services was op-
tional. In 1970, Congress made coverage of home health services mandatory for individuals entitled to skilled
nursing facility services under a State Plan.
11
While CMS has not issued formal guidance on allowing states to provide home health services outside an
individual’s home, CMS has supported and will continue to support such exibility when analyzing State Plan
amendments related to the Home Health benet.
12
These examples are drawn from Colorado’s eligibility criteria for the Home Health benet in the year 2000.
At the time of publication, it was not possible to determine if the State still uses these criteria.
13
State Medicaid Manual, Part 4—Services, §4480.
14
Ibid.
15
Kassner, E., and Jackson, B. (1998). Determining Comparable Levels of Functional Disability. Washington, DC:
AARP, Public Policy Institute. Spector, W.D., and J.A. Fleishman (1998). Combining activities of daily living with
instrumental activities of daily living to measure functional disability. Journal of Gerontology. 53(B):S46-S57.

83
Chapter 3: Determining Service Eligibility
16
At §1902(a)(10)(B) of the Social Security Act.
17
Zaharia, R., and Moseley, C.(2008). State Strategies for Determining Eligibility and Level-of-Care for ICF/
MR and Waiver Program Participants. New Brunswick, NJ: Rutgers Center for State Health Policy. Available
at http://www.hcbs.org/moreInfo.php/doc/2305; Hendrickson, L., and Kyzr-Sheeley, G. (2008). Determining
Medicaid Nursing Home Eligibility: A Survey of State Level of Care Assessment. New Brunswick, NJ: Rutgers
Center for State Health Policy. Available at http://www.hcbs.org/moreInfo.php/doc/2216.
18
Eligibility for ICF/ID services is limited to persons with intellectual disabilities or related conditions (42 CFR
435.1010; 42 CFR 440.150). Eligibility for home and community-based services furnished under §1915(c) or
§1915(b)(c) “managed care” Medicaid waivers is directly linked to the ICF/ID level of care. For both ICFs/ID
and HCBS waiver programs, states must determine during the level-of-care evaluation process that potential
service recipients (a)have a diagnosis of an intellectual disability or a related condition (42 CFR 435.1010; 42
CFR 441.302), and (b)require the level of services provided by an ICF/ID. Intellectual disability (and the former
term “mental retardation”) are not specically dened; related conditions are dened functionally. (States
have generally interpreted the term “related condition” to mean developmental disabilities other than an
intellectual disability. Ernest McKenney, personal communication, December 8, 2009.)
Eligibility for home and community-based services under the waiver program is extended to individuals
who, “but for the provision of waiver services,” would otherwise require the level of support and assistance
furnished by an ICF/ID program (42 CFR 442.302(c)(1)). States are required to use level-of-care evaluation
instruments or processes for waivers that yield equivalent outcomes to those used for the ICF/ID program.
After a person is admitted to the waiver program, states are required to certify at least annually that he or she
continues to need the “level of care provided” (42 CFR 441.302 (c)(2)), during an annual level-of-care determi-
nation process.” Unless noted otherwise, text above is taken verbatim from Zaharia, R., and Moseley, C. (2008),
op. cit.
19
States may use dierent evaluation instruments and processes for determining eligibility for waiver services
than for institutional placement as long as they can explain in their waiver application how and why they dif-
fer and also provide assurances that the outcome of a dierent assessment instrument or process is “reliable,
valid, and fully comparable to the outcome for institutional evaluation. In particular, the state must be able to
demonstrate that individuals who meet level of care via the application of the waiver instrument also would
meet level of care when the institutional instrument is employed.” Appendix B: Participant Access and Eligibil-
ity, Item B-6-e in Application for a §1915(c) Home and Community-Based Waiver, [Version 3.5], Instructions,
Technical Guide and Review Criteria. See the Resources section of this chapter for the web link.
20
42 U.S.C. 15002 Sec. 102.
21
The term ‘‘developmental disability’’ means a severe, chronic disability of an individual that (i)is attributable
to a mental or physical impairment or combination of mental and physical impairments, (ii)is manifested be-
fore the individual attains age 22, (iii)is likely to continue indenitely, and (iv)results in substantial functional
limitations in three or more of the following areas of major life activity: (I)self-care; (II)receptive and expres-
sive language; (III)learning; (IV)mobility; (V)self-direction; (VI)capacity for independent living; (VII)eco-
nomic self-suciency; and (VIII)reects the individual’s need for a combination and sequence of special,
interdisciplinary, or generic services, individualized supports, or other forms of assistance that are of life-long
or extended duration and are individually planned and coordinated (42 U.S.C. 15002 Sec. 102). Note, this
denition is more expansive than the regulatory denition of a “related condition” at 42 CFR 435.1010. The
text that this endnote references, and the endnote itself, are taken verbatim from Zaharia, R., and Moseley, C.
(2008), op. cit.
22
Maryland Dept. of Health and Mental Hygiene v. Brown, 177 Md. App. 440, 935 A.2d 1128 (2007), armed
and opinion adopted, 406 Md. 466, 959 A.2d 807 (2008).
23
States should not use an MMSE score as an eligibility criterion because the MMSE and similar mental status
tests were not designed to determine whether or to what extent an individual needs long-term care services.

84 Understanding Medicaid Home and Community Services: A Primer
These tests were developed as clinical screening tools to determine whether more in-depth assessment is
needed to make a diagnosis of dementia. Most importantly, as the Advisory Panel on Alzheimer’s Disease
has noted, these tests are not correlated with the specic functional limitations or service needs of people
with dementia. O’Keee, J., Tilly, J., and Lucas, C. (May 2006). Medicaid Eligibility Criteria for Long-Term Care
Services: Access for People with Alzheimer’s Disease and Other Dementias. Washington, DC: Alzheimer’s
Association. Additionally, the MMSE is insensitive to the functional limitations common in certain types of
dementia. Many individuals with dementia who have extensive functional limitations will never reach the
score specied in this eligibility criterion. Donald Royall, M.D., Professor and Chief, Division of Aging and
Geriatric Psychiatry, University of Texas Health Science Center at San Antonio. Personal communication,
June 28, 2010.
24
Maryland Department of Health and Mental Hygiene (July 1, 2008). Maryland Medical Assistance Program.
Nursing Home Transmittal No. 213. Available at: http://www.msba.org/sec_comm/sections/elder/docs/
nursinghometransmittal213.pdf.
25
Section 1919(a)(1) of the Social Security Act.
26
O’Keee, J. (1996). Determining the Need for Long-Term Care Services: An Analysis of Health and Functional
Eligibility Criteria in Medicaid Home and Community-Based Waiver Programs. Pub. #9617, Washington, DC:
AARP, Public Policy Institute.
27
For reimbursement purposes, many states distinguish between those who need a skilled level of care and
those who need lower levels of care; others use case mix reimbursement. The need for medical and skilled
nursing services is always assessed when determining if a person needs a skilled or high level of care. It is
when assessing applicants for ICF or minimal levels of care that states dier widely in the measures they
use—some using functional measures only, some nursing measures only, and most a combination of both.
O’Keee, J. (1996). Determining the Need for Long-Term Care Services: An Analysis of Health and Functional
Eligibility Criteria in Medicaid Home and Community-Based Waiver Programs. Washington, DC: AARP, Public
Policy Institute.
28
Application for a §1915(c) Home and Community-Based Waiver, [Version 3.5], Instructions, Technical Guide
and Review Criteria. Glossary, p. 304. See the Resources section of this chapter for a web link to the applica-
tion, instructions, and appendices.
29
Most of the people interviewed in this study were able to remain in the community because they had ex-
tensive informal care supplemented by small amounts of privately paid care. O’Keee, J., Long, S.K., Liu, K.,
and Kerr, M. (1999). How do They Manage? A Case Study of Elderly Persons Functionally Eligible for Medic-
aid Waiver Services but Not Receiving Them. Washington, DC: AARP, Public Policy Institute.
30
In a study of 42 states’ nursing facility level-of-care criteria, respondents in states that used less stringent
criteria said that most beneciaries with lower levels of need could be safely served in the community.
O’Keee, J. (1996). Determining the Need for Long-Term Care Services: An Analysis of Health and Functional
Eligibility Criteria in Medicaid Home and Community-Based Waiver Programs. Washington, DC: AARP, Public
Policy Institute.
31
P.L. 109–171. §6086(a).
32
The lack of functional criteria is more likely to be an issue for ICF/MR level-of-care criteria (which in some
states is largely determined by diagnosis) than for nursing facility level-of-care criteria.
33
State Medicaid Director Letter, August 6, 2010. Available at http://www.cms.gov/smdl/downloads/
SMD10015.pdf.
34
Section 2401 of the Aordable Care Act, amending §1915 of the Social Security Act.

Chapter 4: Options for Designing Service Coverage: General Considerations
85
Guide to Chapter 4
Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 87
Medicaid Home and Community Services: An Overview . . . . . . . . . . . . . . . . . . . . . . . . . 87
Federal Policy Considerations . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 91
State Policy Goals and Objectives . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 93
Home and Community Services under the Medicaid State Plan . . . . . . . . . . . . . . . . . . . . . . . . . . 94
Personal Care/Personal Assistance . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 95
State Plan Home and Community-Based Services . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 99
Community First Choice Option . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .100
Services That May Be Oered Under an HCBS Waiver Program . . . . . . . . . . . . . . . . . . . . . . . . . .102
Supports Waivers . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .105
Supporting Individuals to Live in Their Own or Family Home. . . . . . . . . . . . . . . . . . . . . . . . . . . .106
Medicaid Financing for Supports to Individuals Living in Their Own Home . . . . . .106
Factors to Consider When Choosing Coverage Options: Two Illustrative Services . . . . . . . .107
1. Personal Care/Personal Assistance . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .107
2. Case Management . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .111
Resources. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .116
Endnotes: Citations, Additional Information, and Web Addresses . . . . . . . . . . . . . . . . . . . . . . .119
87
Chapter 4: Options for Designing Service Coverage: General Considerations
Chapter 4
Options for Designing Service Coverage: General Considerations
To remain in their homes and communities, many people with disabilities and chronic conditions need long-term
care services and supports, ranging from personal assistance to more specialized services, as well as assistive tech-
nology and environmental modications. Federal Medicaid law and policy give states great latitude to oer indi-
viduals a wide range of home and community services through a state’s regular Medicaid program. States can also
oer a comprehensive range of services by operating one or several home and community-based services (HCBS)
waiver programs. This chapter discusses Medicaid coverage options, including important issues states need to
consider in selecting the particular combination of home and community services and benets that best suits their
needs.1
Introduction
Changes in Federal Medicaid statute and policy over the past three decades have made it feasible for states to
provide a wide range of home and community services. The many options for furnishing these services can be
confusing for policymakers, state ocials, advocates, and consumers alike, as they can be funded through one
or more of three alternative routes: (1)a state’s regular Medicaid State Plan, (2)managed care programs, and/
or (3)one or several HCBS waiver programs, each oering a distinct package of services and supports to dier-
ent groups of individuals.2
Combining these alternatives in creative ways can give states substantial latitude in designing their Medicaid
home and community service coverages and customizing benet packages to meet the needs of particular
groups. Use of HCBS waivers also provides considerable exibility for states to manage service costs and the
number of people served. This exibility explains the considerable variation in the services and supports that
states oer.
This chapter begins with an overview of the broad types of Medicaid home and community services and sup-
ports a state may oer. It then describes major Federal and state considerations that can inuence decisions
concerning whether to oer a service as a regular Medicaid program benet or through an HCBS waiver pro-
gram. The chapter concludes with more detailed descriptions and illustrations of coverage options—focusing
rst on services that may be oered under the regular Medicaid State Plan and then on services that may be
oered under an HCBS waiver program.
Medicaid Home and Community Services: An Overview
Home and community services can be thought of as falling into ve overarching categories. It is useful to con-
sider these in generic terms before proceeding to a detailed discussion of how they are treated in Medicaid
law and policy.

88 Understanding Medicaid Home and Community Services: A Primer
Personal Care—also called personal assistance and
attendant care—involves helping individuals per-
form everyday activities when they have physical or
mental impairments that prevent them from carry-
ing out these activities independently. These activi-
ties can include Activities of Daily Living (ADLs) and
Instrumental Activities of Daily Living (IADLs). ADLs
include eating, bathing, dressing, toileting, transfer-
ring from bed to chair, and maintaining continence.
IADLs include activities such as light housework,
laundry, transportation, and medication manage-
ment.
This assistance can be furnished in the home or
community settings, as well as to individuals who
live in foster care, group homes, and other residen-
tial care settings. The terms used for individuals who
provide personal care vary, and include personal
assistants, personal attendants, personal care aides,
and direct care workers. Certied nursing assistants
and home health aides also provide personal care.
Individuals with various types of disabilities often
require this form of basic assistance throughout
their lives. Thus, a need for personal care is a major,
if not the primary, reason many individuals seek
Medicaid long-term care services and supports.
States use several dierent terms to describe assis-
tance with ADLs and IADLs, which may be provided
under the mandatory Home Health benet, the op-
tional State Plan Personal Care benet, the optional
Section (§)1915(i) HCBS State Plan benet, and/or
a §1915(c) wai ver (hereafter called HCBS waiver). In
October 2011, an additional State Plan option will
be available—the §1915(k) Community First Choice
Option benet, which was authorized by the Patient
Protection and Aordable Care Act of 2010 (here-
after called the Aordable Care Act). Personal care
can also be provided under the optional §1915(j)
Self-directed Personal Assistance Services State Plan
benet. However, only states that oer personal
care under either the State Plan Personal Care op-
tion or an HCBS waiver may employ the §1915(j)
authority. (See Chapter 7 for a detailed discussion of
the §1915(j) authority.)
Health-Related Services. Personal care can include
assistance with health and health-related tasks,
which encompass a wide range of skilled and
unskilled nursing services that address chronic
conditions and functional impairments (e.g., tube
feedings, catheterization, range of motion exercises,
and medication administration). However, assis-
tance with skilled tasks may be provided only when
delegated by a licensed nurse in accordance with
state law.
Specialty Services. This category comprises a wide
range of services related to the specic nature of
an individual’s impairment. These services gener-
ally share the common aim of helping individuals
to improve their functioning. Adult day health
services address both functional and health needs.
Psychiatric rehabilitation services address the needs
of individuals who have a mental illness that im-
pairs their functioning. Habilitation services en-
able people with intellectual disabilities and other
developmental disabilities (ID/DD, hereafter called
developmental disabilities) to acquire or improve
skills to help them become more independent.
Assistive technology helps people with many types
of disabilities become more self-sucient. States
may oer these specialized services through vari-
ous options, including an HCBS waiver program.
Many types of assistive technology (e.g., motorized
wheelchairs and communication devices) are forms
of medical equipment and supplies covered under
the mandatory Home Health benet.
Adaptive Services. In order to remain in their own
home and function in the community, many indi-
viduals with physical impairments need home and
vehicle modications. Home modications include
the installation of wheelchair ramps, widening
doorways, and retrotting bathrooms and kitch-
ens so that individuals with physical impairments
can get around their homes. Vehicle modications
include modifying a car or a van to enable a person
to drive or be transported to work and/or commu-
nity activities. These services can be covered under
HCBS waiver programs.

89
Chapter 4: Options for Designing Service Coverage: General Considerations
Family and Caregiver Supports. These supports
are designed to help family members and friends
who support individuals with disabilities. Vari-
ous Medicaid options are available to maintain
and strengthen these supports. Respite care—for
unpaid caregivers who are absent or need relief—is
one of these services. State Plan personal care ser-
vices—in addition to those provided on an ongoing
basis—can be authorized to temporarily relieve an
unpaid caregiver.
States may also provide “caregiver training and edu-
cation” as a distinct service under an HCBS waiver
program to strengthen an unpaid caregiver’s ability
to meet the needs of the person they are assisting.
Training and education can cover a wide range of
topics, such as instructions for using equipment
specied in the service plan and ensuring com-
pliance with treatment regimens. It may include
(a)paying trainers to come into the home to teach
skills and techniques for addressing the program
participant’s (hereafter, the participant’s) needs, so
that training can be customized to the individual
and the caregivers; (b)paying for caregivers to
attend special training and education classes; and
(c)paying the expenses associated with caregivers
attending workshops and conferences where they
learn how to better meet participants’ needs. (These
expenses might include conference fees, arranging
substitute care while caregivers are away, or paying
for personal assistance at the training conference
itself if the participant accompanies the caregiver.)
Caregiver training may also be paid for under the
optional Rehabilitation benet. Rehabilitation ser-
vices in Kentucky, for example, include home visits
to (a)help family members and seriously mentally
ill beneciaries practice eective communication
techniques to defuse stressful situations that occur
in home settings, and (b)coach family members to
improve their skills for managing a severely emo-
tionally disturbed child. Training and supports may
also be oered as component parts of other ben-
ets, such as Home Health.
Social Supports. Social supports are intended to
help individuals take an active part in both their
family and community and can help avoid so-
cial isolation. Social supports such as companion
services, for example, provide assistance so that
individuals can participate in community activities
(e.g., by providing a personal attendant to enable
the individual to attend church). These services can
be covered under HCBS waiver and State Plan HCBS
programs.
Case Management/Service Coordination helps
individuals who need services and supports funded
by several sources. Some may be available through
the Medicaid State Plan and others through other
public programs such as state programs for person
with disabilities and programs funded under the
Older Americans Act. A common feature of home
and community services is the provision of case
managers, who may also be called care coordina-
tors, service coordinators, or support coordinators.
They frequently prepare—or facilitate preparation
of—an individual service plan that describes how all
the services and supports a person might need will
be identied and delivered. They also play an active
role in monitoring the quality and eectiveness of
home and community services. Several Medicaid
options are available for covering case manage-
ment/service coordination, which are discussed
later in this chapter.
As states consider which home and community
benets to oer, and how to oer them, it is help-
ful to keep in mind that no bright line distinguishes
home and community services and supports from
other types of Medicaid benets. Many benets not
mentioned in this overview are very much a part of
the mix required to meet the needs of individuals
with disabilities and chronic conditions. For exam-
ple, State Plan coverage of medical equipment and
supplies can provide power wheelchairs and other
mobility aids. The State Plan may also cover thera-
peutic services such as occupational and physical
therapy, which many
90 Understanding Medicaid Home and Community Services: A Primer
Respite Benets
Respite benets encompass whatever services an individual needs (e.g., personal care and nursing services).
They are usually furnished on an intermittent basis explicitly to provide relief to primary unpaid caregivers. Re-
spite, for example, can be provided to give parents a night or weekend o periodically from the intense caregiv-
ing needed to support children with severe cognitive and/or physical disabilities or medical needs. It is particu-
larly needed if caregivers themselves become ill.
Respite is also important for spouses or adult caregivers of older adults, particularly those with dementia who
need around-the-clock supervision. Respite care benets the individual directly by providing services usually fur-
nished by caregivers, and indirectly by helping avoid caregiver “burnout,” which can lead to institutionalization.
Under HCBS waiver programs, respite can be provided in the family home by bringing a worker into the home
while the caregivers are away for a few hours or overnight.
Some states also allow respite care provided through HCBS waiver programs to be furnished at sites other than
the family home, including especially designated respite care facilities. This out-of-home respite is used most
often when the primary caregiver(s) will be away overnight or for extended periods, or to enable the primary
caregiver(s) to be at home alone during the respite period.
States may establish whatever limits they elect with respect to the amount of respite that will be available to pri-
mary unpaid caregivers. It is not uncommon for states to cap the amount of respite at 30 days during a calendar
year. Some states do not impose such caps in their HCBS waiver programs, leaving the amount of respite that will
be authorized to be worked out during the individual service planning process based on the needs and circum-
stances of the particular informal caregivers.
Most states permit caregivers to “bank” respite benets and to use the authorized amount whenever it is most
needed. This practice recognizes that since respite is intended to renew the energies of the caregiver (for the di-
rect longer term benet of the participant), caregivers should determine when it is used. States have the option
to permit “banked respite” to be carried over from one year to the next.

91
Chapter 4: Options for Designing Service Coverage: General Considerations
individuals need to improve or prevent a decline
in their functioning. As a consequence, in crafting
eective home and community service strategies,
it is important to take stock of other services in
the Medicaid State Plan and to modify or possibly
supplement them if needed. This will help to ensure
that the coverages chosen address the key needs of
those being served.
As states determine what services and supports to
oer, they need to consider certain Federal policy
issues and state goals and objectives that constrain,
or at least shape, their benet choices. The next
section addresses the Federal dimension and is fol-
lowed by a general discussion of state policy goals
and objectives.
Federal Policy Considerations
While Federal Medicaid law and policy give states
considerable latitude in deciding which Medicaid
home and community services they will oer, states
do not have complete freedom. State choices must
be consistent with Federal requirements and limita-
tions. Seven major Federal considerations merit
discussion here. Although they aect state exibility
somewhat, they need not pose serious barriers to
developing eective strategies to support individu-
als in their homes and communities.
State Plan Requirements. All services covered under
a state’s Medicaid plan—both mandatory and
optional—are subject to two important statutory
requirements. First, they must be available on a
comparable basis to all state Medicaid beneciaries
(in an eligibility group) who need the service. States
must use the same eligibility criteria for all appli-
cants and any limits on service amount, scope, and
duration must be equally applied to both individu-
als currently receiving services and those applying
for services. The eect of these requirements is that
states cannot have a waiting list and any changes
made in the eligibility criteria, as well as service
amount, scope and duration, must be applied
equally to both those currently receiving services
and those applying for them. These provisions con-
stitute the “comparability” requirement.
Second, services must be available statewide (i.e.,
the state cannot restrict the availability of the
service to particular geographic regions). This is
called the “statewideness” requirement.
4
There are
few exceptions to this statewideness requirement;
targeted case management is a major one. Federal
regulations also require that each Medi caid service
be sucient in amount, duration, and scope to
achieve its purpose. Within this broad requirement,
states have the authority to establish reasonable
and appropriate limits on the amount, duration, and
scope of each service.
Generally, when a state wishes to make home
and community services available only to cer-
tain distinct groups of Medicaid beneciaries
(e.g., adults with physical disabilities) it must seek
Federal approval of an HCBS waiver.
4
This waiver
authority permits states to waive both the compa-
rability and statewideness requirements in order
to target services to distinct groups of Medicaid
beneciaries. Once eligible for a waiver program,
participants must be provided all of the waiver
services for which they have a documented need,
and the services must be available in all parts of the
state covered by the waiver. The Aordable Care
Act includes a provision waiving comparability for
services provided under the State Plan §1915(i)
authority, but services must be provided statewide
to everyone who meets the eligibility criteria.
5
Services That Cannot Be Oered under the State
Plan. Some services may not be oered under a
Medicaid State Plan because they have not been
specied in either the authorizing legislation or
implementing regulations. An example is home
modications, which explains why home modica-
tions is one of the most common services oered
under HCBS waiver programs.
HCBS Waiver Coverage to Complement or Expand
State Plan Coverage. Through an HCBS waiver, a
state may augment the services it provides under
the State Plan. When a state retains the scope of a
State Plan service but increases its amount, dura-
tion, or frequency, the service is considered an “ex-
tended State Plan” service. For example, a state may
allow four home health aide visits each week under
the State Plan Home Health benet and allow three
additional visits under an HCBS waiver. States must
92 Understanding Medicaid Home and Community Services: A Primer
have established mechanisms to ensure no duplica-
tion of service provision or billing for State Plan and
waiver services.
6
Non-duplication. Federal policy provides that a
state may not oer precisely the same service
under an HCBS waiver that it oers under its regu-
lar Medicaid program. The reason for this prohibi-
tion is simple. People who participate in an HCBS
waiver program are already eligible, by denition, to
receive the full range of services available under the
State Plan. While a waiver service may be similar in
scope to a State Plan service, it would be considered
an “other” service rather than an “extended State
Plan” service if the method of service delivery (e.g.,
giving participants the ability to direct their servic-
es) diers under the waiver. States have added tasks
to the scope of services covered under a State Plan
in order to create a new waiver service that does not
duplicate the State Plan service (see Box).
EPSDT Mandate. When children are served in an
HCBS waiver program, states must take account of
the mandate to provide enhanced Early and Peri-
odic Screening, Diagnosis and Treatment (EPSDT)
services. Federal EPSDT requirements mandate that
Medicaid-eligible children receive all medically
necessary services (listed in §1905(a) of the Social
Security Act) that they require, regardless of wheth-
er such services are specically included in the State
Plan. Thus, medically necessary services for children
who need them cannot be restricted to children
who are waiver participants.
Redening Services: State Example
Texas provides attendant services through its
State Plan Personal Care program. The State
expanded the scope of attendant services to be
provided in its Community Based Alternatives
waiver to include protective supervision as tem-
porary relief for the primary caregiver, extension
of therapy services, and the performance of
nursing tasks delegated by licensed registered
nurses. Because the new service—called Person-
al Assistance Services—diers from attendant
services provided under the State Plan, waiver
participants do not have to rst obtain atten-
dant services under the State Plan Personal Care
program before receiving personal assistance
services through the waiver program.
Service Objective. A state can only oer services
that are materially related to the basic reasons a
person needs long-term services and supports. This
may seem obvious enough, but complicating issues
sometimes arise. In the case of services provided
under HCBS waivers, for example, a state may oer
only services that are either necessary for people
to avoid institutionalization or would be available
to beneciaries if they were in a facility. This provi-
sion takes no account of other services and sup-
ports—such as guardianship services and leisure
activities—that might be desirable but cannot be
considered necessary given the aims expressed in
Federal law. This does not imply that the state is pre-
vented from providing such services and supports;
only that Federal Medicaid dollars cannot be used
to purchase them.
Room and Board Expenses. Federal Medicaid dollars
are not available to pay for the “room and board”
expenses (i.e., housing, utilities, and food) of non-
institutionalized persons, except in limited circum-
stances such as (a)out-of-home respite care, and
(b)the room and board costs of a live-in caregiver.
Federal nancial participation (FFP) is available for
room and board provided as part of respite care
furnished in a facility that is approved by the state
but not in a private residence.

93
Chapter 4: Options for Designing Service Coverage: General Considerations
The expectation is that individuals will use their
own income and resources (e.g., Federal Supple-
mental Security Income [SSI] benets and earn-
ings from employment) to meet room and board
expenses. The room and board exclusion can
complicate the development of strategies to sup-
port individuals in their homes and community-
based residential care settings. In contrast, room
and board expenses are Medicaid-reimbursable in
institutions, where individuals receive a signicantly
reduced SSI payment as a personal needs allowance
($30/month).
Obligations of Other Payers. Medicaid is deemed a
payer of last resort. This means that if another pub-
lic program or private third-party payer—such as a
private health insurance plan—is obliged to provide
a service to an individual, a state generally may not
replace this funding with Medicaid dollars. For ex-
ample, if two public programs such as Medicare and
Medicaid cover the same service and an individual
is eligible for the service in both programs, Medi-
care must pay rst for the service. Medicaid can only
pay once Medicare benets are exhausted.
State Policy Goals and Objectives
Federal policies provide a framework within which
states can weigh their options in deciding whether
to oer a service under their Medicaid State Plan or
through an HCBS waiver program. But a state makes
its particular coverage choices in light of its own
policy goals and objectives. Five major factors need
highlighting in this connection.
State Budget Impact. States must balance their bud-
gets on a regular basis—every year, for most states.
This requirement can make states wary of oering
services under their Medicaid State Plan, because
Federal rules prohibit them from reducing services
below the amount, duration, and scope needed to
achieve their purpose, and from limiting the num-
ber of people who receive the service. While states
can set the medical necessity criteria for State Plan
services, they must serve everyone in the state who
requests services and meets the criteria. Because
they cannot predict how many individuals will qual-
ify and how much it will cost to serve each person,
spending for State Plan services is less predictable
than for HCBS waiver programs.
Predictability of costs is the major reason why many
states have used HCBS waiver programs to expand
the availability of home and community services
rather than through State Plan benets, such as
Home Health and Personal Care. HCBS waivers
permit states to serve only a set number of bene-
ciaries that the state itself establishes for the waiver
and to set individual cost limits for participants.
States may also use an aggregate cost neutrality cal-
culation to determine the total amount of funding
available for waiver services. Compared to setting
per capita limits for waiver participants, this ap-
proach gives states the exibility to serve individu-
als with extensive needs who require more services
than the average participant.
However, states that limit the provision of home
and community services to HCBS waiver programs
limit themselves to serving only a high-need
population—those who meet institutional level-of-
care criteria. By providing State Plan services (e.g.,
under the Personal Care, Rehabilitation, and/or the
§1915(i) benets), states can serve a population
with lower needs and help individuals maintain—
and/or slow the decline of—their health and func-
tional status, thereby delaying the need for more
costly services and supports.
Inclusiveness. When deciding whether to cover a
service under the State Plan or an HCBS waiver pro-
gram or both, states need to carefully consider how
services provided in dierent programs can comple-
ment each other in furnishing people with disabili-
ties the right amount and combination of services.
Target Populations. With a few exceptions, ser-
vices oered under a Medicaid State Plan must be
provided to all eligible individuals on a comparable
basis.
7
Thus, it can be dicult to vary services or
service delivery approaches based on the needs
of individuals who have specic impairments and
specialized needs. It also can be easier for a state to
craft a package of services and supports to meet the
needs of specic groups than to seek a one-size-ts-
all State Plan coverage design.
These considerations frequently lead states to select
an HCBS waiver program as a vehicle for oering

94 Understanding Medicaid Home and Community Services: A Primer
services to dened groups of individuals, because
the service package can be designed to meet their
distinct needs. The recently enacted §1915(i) HCBS
State Plan option also permits states to target ser-
vices to specic groups.
Maintaining a Unied Service Delivery System.
While Medicaid is the major funding source for
home and community services, it is frequently not
the only one. In many states, distinct state-funded
service systems or networks have evolved for
specic target populations, for example, individuals
who are elderly, who have a serious mental illness,
or who have a developmental disability. One group
for which states have historically not developed
specic programs or service systems is people 18 to
64 years of age with physical disabilities—a group
that is frequently underserved. Some states, such
as Connecticut, have programs targeted to people
who are nancially ineligible for Medicaid but meet
the state’s institutional level-of-care criteria.
8
These state-funded service systems often play a
crucial role in expanding home and community ser-
vices for the groups they serve. But they vary con-
siderably in the types and amounts of services they
provide and the numbers of people they serve. It is
important to maintain these service systems, but it
is also important to ensure that they are integrated
into a unied service delivery system for their par-
ticular target group. An eective way of achieving
this integration for many states is the targeted ap-
proach permitted under an HCBS waiver program.
This is a way of accessing Medicaid funding at the
same time as ensuring consistency in nancing and
practice across an array of funding sources.
Eligibility. As discussed in Chapter 2, a state can
qualify more individuals living in the community
for Medicaid using an HCBS waiver program than it
can under its State Plan because it has the option to
use the more liberal nancial eligibility rules used
for institutions when determining eligibility for an
HCBS waiver. Some individuals in the community
who might not qualify for State Plan Medicaid ben-
ets because they do not meet the income criteria,
in particular, may be eligible for services under an
HCBS waiver program, if the state uses institutional
nancial eligibility rules.
The following two sections, respectively, provide
detailed descriptions of the home and community
services that can be provided (a)under the Med-
icaid State Plan, and/or (b)through HCBS waiver
programs.
Home and Community Services
under the Medicaid State Plan
Federal law distinguishes between services oered
under a Medicaid State Plan and services that may
be oered when the Secretary of Health and Human
Services (HHS)—operating through the Centers for
Medicare & Medicaid Services (CMS)—grants waiv-
ers for a state to operate an HCBS waiver program.
The services that can be oered without a waiver
are called Medicaid State Plan services. Some of
these services must be provided by every state that
operates a Medicaid program, for example, home
health services. These are called mandatory servic-
es.
9
Others can be provided at state option—called
optional services.
When a state covers a service under its Medicaid
State Plan, it may impose limits on exactly what will
be provided and under what circumstances. Such
limitations take four forms: (1)medical/
functional need, (2)how often a person may receive
a service (amount), (3)for how long (duration), and
(4)the exact nature of what is provided (scope).
However, Federal law requires that such limitations
not undermine a person’s receipt of necessary assis-
tance. Any limitations states establish must gener-
ally be based on clinical grounds. Although limits
must not prevent the state from meeting the needs
of most Medicaid beneciaries most of the time,
states are not required to meet all beneciaries’
needs all the time.
A state’s decision to oer an optional service under
its Medicaid State Plan amounts to a decision to
make the service available to all individuals who
require it, within whatever limitations on eligibility,
amount, scope, and duration the state has estab-
lished. This is why Medicaid beneciaries are said to
be “entitled” to State Plan services.
10

95
Chapter 4: Options for Designing Service Coverage: General Considerations
A state has the option of covering under its State
Plan four key home and community services that
are especially important for people with disabilities:
(1)personal care, (2)targeted case management,
(3)clinic services, and (4)rehabilitative services. Ad-
ditionally, the state can cover a wide range of home
and community services under the new HCBS State
Plan option created by the
Decit Reduction Act of 2005 (DRA-2005) and
amended by the Aordable Care Act.
Each of these State Plan options will be discussed
next, followed by a brief discussion of services that
can be oered under an HCBS waiver program.
Personal Care/Personal Assistance
11
Prior to enactment of the Omnibus Reconciliation
Act of 1993 (OBRA 93), personal care services of-
fered through the State Plan were limited in scope
and had a medical orientation, due to the require-
ment that they be authorized by a physician and
supervised by a nurse. OBRA 93—together with
implementing regulations eective in November
1997—gave states the option to substantially
broaden the scope of personal care services to
furnish individuals a wide range of assistance in ev-
eryday activities, both in and outside their homes.
12
In January 1999, CMS released a State Medicaid
Manual Transmittal that updated the guidelines
concerning coverage of personal care services. In
it, CMS made clear that (a)personal care services
include assistance with both ADLs and IADLs, and
(b)personal care for people with cognitive impair-
ments may include cueing along with supervision
to ensure the individuals perform the task properly.
Formerly, such supervision generally was consid-
ered outside the scope of personal care. (See the
Resources section of this chapter for a link to the
Medicaid Manual.)
A state may now extend such services to include
supervision and assistance to people with cogni-
tive impairments, which can include people with
mental illness, intellectual disabilities, and demen-
tia. However, this supervision and assistance must
be related directly to the perfor mance of ADLs and
IADLs. Companionship or custodial observation of
an individual, absent hands-on or cueing assistance
that is necessary and directly related to ADLs or
IADLs, is not a Medicaid personal care service.
Specic provisions in the Manual are discussed next.
Scope of services—Personal care services covered
under a state’s program may include a range of
human assistance provided to people with dis-
abilities and chronic conditions of all ages, which
enables them to accomplish tasks they would
normally do for themselves if they did not have a
disability. Assistance may be in the form of hands-
on assistance (actually performing a personal
care task for a person) or cueing so that a person
performs the tasks by him/herself. Such assistance
most often relates to performance of ADLs and
IADLs . . . Personal care services can be provided
on a continuing basis or on episodic occasions.
Skilled services that may be performed only by a
health professional are not considered personal
care services.
However, skilled services may be provided under
the State Plan Personal Care benet when delegat-
ed by a licensed nurse in accordance with state law.
Cognitive impairments—An individual may be
physically capable of performing ADLs and IADLs
but may have limitations in performing these
activities because [of] a cognitive impairment . . .
Personal care services may be required because a
cognitive impairment prevents an individual from
knowing when or how to carry out the task. For
example, an individual may no longer be able to
dress without someone to cue him or her on how
to do so. In such cases, personal assistance may
include cueing along with supervision to ensure
that the individual performs the task properly.

96 Understanding Medicaid Home and Community Services: A Primer
In October 1999, CMS further revised the Manual
to permit states to oer the option of consumer-
directed personal care services (also called self-
direction or participant direction). The Manual
revisions explicitly recognized that individuals
who are receiving personal assistance may direct
their workers, that is, train, supervise, manage, and
dismiss them (if needed). In particular, the Manual
states the following:
Consumer-directed services—A state may
employ a consumer-directed service delivery
model to provide personal care services under
the Personal Care optional benet to individuals
in need of personal assistance, including people
with cognitive impairments, who have the ability
and desire to manage their own care.
See the discussion later in this chapter—and in
Chapter 7—about the §1915(j) State Plan authority,
which expands participant direction service delivery
options for both the State Plan Personal Care ben-
et and HCBS waiver programs.
These Manual materials describe a comprehensive
scope of personal care/assistance that a state may
choose to cover under its Medicaid State Plan—in
keeping with contemporary views concerning the
role personal assistance can play in supporting indi-
viduals with disabilities in a wide range of everyday
activities.
As a result of the changes made in Federal policy,
there is now little dierence in the scope of per-
sonal care services that may be oered under the
Medicaid State Plan and those that may be oered
under an HCBS waiver program. However, neither
the provisions of OBRA 93 nor the revised Fed-
eral regulations and CMS State Medi caid Manual
guidelines require a state to change the scope of its
pre-1993 coverage. In order to take advantage of
these changes, a state must le an amendment to
its Medicaid State Plan.
Targeted Case Management Services
States have the option of covering case manage-
ment services for a dened group of Medicaid
recipients, or for multiple groups, as long as dier-
ent provisions apply to each specied group (hence,
the term “targeted”).
13
Targeted case management
services are exempt from the comparability require-
ment, that is, they do not have to be available to all
Medicaid beneciaries. They can also be oered on
a less than statewide basis.
14
For example, a state may oer one form of targeted
case management services to recipients who have
a mental illness and another to people who are
elderly and have physical impairments. States may
use their own denitions to dene target groups
and may do so broadly (e.g., all Medicaid-eligible
individuals with a developmental disability) or more
narrowly (e.g., Medicaid-eligible individuals with a
developmental disability who also have a mental
illness). Other target groups states have established
include
• Adults with serious mental illness as dened by
the state.
• Children from birth to age 3 who are experienc-
ing developmental delays or behavioral disor-
ders as measured and veried by diagnostic
instruments and procedures.
• Pregnant women and infants up to age 1.
• Individuals 60 years of age or older who have
two or more physical or mental diagnoses that
result in a need for two or more services.
• Individuals with AIDS or HIV-related disorders.
• People being transitioned from nursing homes
to the community.
• Individuals enrolled in HCBS waiver programs.
Although the targeting aspects of this case man-
agement coverage make it somewhat akin to the
HCBS waiver program, there is one important
dierence. Once a state has established its target
population and geographic locations, targeted
case management services must be furnished to all
eligible individuals. A state may not limit the num-
ber of eligible individuals who may receive these
services.
States do have the option of limiting the entities
that may furnish targeted case management ser-
vices to individuals with a developmental disability

97
Chapter 4: Options for Designing Service Coverage: General Considerations
or a mental illness to enable them to tie provision of
these services to the “single point of entry” systems
common in state service systems that serve these
populations. Doing so enables states to maintain a
unied service delivery approach.
The four components of targeted case management
include assessment, service plan development, re-
ferrals, and monitoring. Targeted case management
services can be described as “planning, linking, and
monitoring” the provision of direct services and
supports obtained from various sources (the Med-
icaid program itself, other public programs, and a
wide variety of private sources), making their scope
very broad. Permitted activities can include (1)as-
sistance in obtaining food stamps, housing, and
legal services; (2)service/support assessment and
planning; and (3)monitoring the delivery of direct
services and supports to ensure they are meeting
individuals’ needs.
Although a range of activities on behalf of bene-
ciaries can be included within the scope of targeted
case management, some cannot. In particular,
• Activities related to authorization and approval
of Medicaid services.15
• Activities related to making basic Medicaid
eligibility determinations.
• Activities that constitute “direct services” to the
consumer (e.g., transporting an individual to
and from a doctor’s appointment is outside the
scope of targeted case management).16
• Activities provided to individuals in institutions.
This restriction is based on two Federal provi-
sions: (a)Federal regulations concerning Med-
icaid institutional services require that facilities
provide care coordination services to residents,
and (b)Medicaid prohibits duplicate payments
for the same service. However, targeted case
management services may be provided to resi-
dents of institutions in the last 180 consecutive
days of a Medicaid-eligible person’s institution-
al stay, if provided for community transition.
(See Chapter 6 for a discussion of Medicaid
provisions related to transitioning from institu-
tions to the community.)
• Activities that overlap or duplicate similar
services a person receives through other means
(e.g., development of a service plan by an HCBS
waiver case manager).
Other Medicaid options for covering case manage-
ment services are discussed later in this chapter.
Clinic Services
17
States have the option of covering specialized treat-
ment services and other supports under several
State Plan benets. The two benets that states
most frequently cover are the optional Clinic benet
and the optional Rehabilitation benet. States em-
ploy the Clinic benet for a wide variety of purposes
in their state Medicaid programs, including paying
for services furnished through health care clinics
and community mental health centers.
The Clinic benet also serves as a means of paying
for mental health services furnished to Medicaid
beneciaries on an outpatient basis. Mental health
clinics may provide mental health therapy and
other treatment to Medicaid beneciaries—services
needed by people who have serious and persistent
mental illness and need long-term care services
and supports to remain in their communities. The
clinical services provided through the Clinic benet
must be site-based and supervised by a physician.
(See the Resources section of this chapter for a web
link to a publication on how to use Medicaid to pro-
vide services for adults with serious mental illness.)
Rehabilitation
18
The Rehabilitation benet allows states more ex-
ibility to design service packages than does the
Clinic benet, because of its broad denition in
Federal regulation: “any medical or remedial servic-
es recommended by a physician or other licensed
practitioner of the healing arts, within the scope of
his practice under state law, for maximum reduction
of physical or mental disabilities and restoration of a
recipient to his/her best functional level.”
Rehabilitation services can include those that are
also covered under the Clinic benet. But unlike
services under that option, they are portable (i.e.,

98 Understanding Medicaid Home and Community Services: A Primer
not limited to specic sites under the direct, on-site
supervision of a physician). Many other services
also fall within the scope of Rehabilitation. Psy-
chiatric rehabilitation services include basic living
skills training (including independent living skills
and cognitive skills, as well as education regarding
medications and medication management), social
skills training, counseling and therapy, and collateral
services, such as consultation with and training of
family members, primary caretakers, providers, legal
guardians or other representatives, and signicant
others. Such training and counseling is limited to
activities that directly support the individual.
19
Collateral services can be covered as a specic
stand-alone category or as part of day treatment
or intensive in-home services. Through this activity,
reimbursement is provided for face-to-face encoun-
ters with people who are important in the ben-
eciary’s life, when those encounters are needed
to develop or implement the rehabilitation plan.
Psychiatric rehabilitation services are furnished in a
variety of locations, including homes, partial hospi-
talization or day programs for adults, day treatment
programs in schools or other locations for children,
and residential placements (including facilities with
fewer than 16 beds, such as group homes or thera-
peutic foster care homes). Crisis services and early
intervention services, including services for very
young children exhibiting signs of serious emotion-
al disorders, are also furnished under this option.
20
These services, along with personal care and
targeted case management, can be combined to
meet a wide range of service and support needs
for people who have a mental illness. Of the 46
states that use the Rehabilitation benet, many also
provide targeted case management services to this
population.
21
The Clinic and Rehabilitation optional benets are
not generally used to provide long-term care servic-
es and supports to individuals with disabilities other
than mental illness. During the 1970s and 1980s, a
few states secured CMS approval to cover daytime
services for people with developmental disabilities
under either the Clinic or the Rehabilitation ben-
et. CMS ultimately ruled that the services being
furnished were habilitative rather than rehabilita-
tive and consequently could not be covered under
either option in additional states.
However, Congress acted in 1989 to permit states
that had secured CMS approval of these coverages
to continue them but eectively prohibited other
states from adding such coverage. The main basis
for this ruling was that habilitative services could
be furnished only to residents of intermediate care
facilities for individuals with an intellectual disability
(ICFs/ID) under the State Plan or through an HCBS
waiver program for individuals who might other-
wise be eligible for ICF/ID services. A few states have
maintained their coverage of these services. But
many have dismantled their coverages in favor of
oering similar services through their HCBS waiver
programs. With the creation of the new HCBS State
Plan option under the §1915(i) authority, states may
now cover habilitation under the State Plan.
99
Chapter 4: Options for Designing Service Coverage: General Considerations
State Plan Home and
Community-Based Services
22
The DRA-2005 added §1915(i) to the Social Security
Act, which allows states, at their option, to provide
a broad range of home and community-based
services under the Medicaid State Plan.
23
The Aord-
able Care Act made a number of signicant changes
to the §1915(i) authority.
Section 1915(i) allows states to include any or all
of the services that are listed in §1915(c)(4)(B) of
the Social Security Act. These services include case
management, homemaker/home health aide, per-
sonal care, adult day health, habilitation, and respite
care services. In addition, the following services may
be provided to persons with chronic mental illness:
day treatment, other partial hospitalization services,
psychosocial rehabilitation services, and clinic ser-
vices (whether or not furnished in a facility). States
may also oer “such other services…as the Secre-
tary may approve.” CMS has drafted an application
for states to submit a State Plan amendment to add
an HCBS benet.
All individuals served under §1915(i) must meet
the needs-based criteria the state establishes for its
HCBS benet. These criteria must be less stringent
than its level-of-care criteria for institutional ser-
vices, that is, nursing facilities, ICFs/
ID, and hospitals that are Medicaid certied as hos-
pitals but provide long-term care services. These cri-
teria cannot be based solely on diagnosis but must
be based on an assessed need for a set of supports
and services due to functional limitations.
The evaluation process to determine eligibility must
be independent and not present a conict of inter-
est (i.e., service providers may not be involved in the
eligibility determination process if
Proposed Changes to Rehabilitation Benet Withdrawn
On August 13, 2007, CMS published a proposed rule—Medicaid Program; Coverage for Rehabilitative Services—
in the Federal Register to clarify the denition of Medicaid “rehabilitative services” and to establish new documen-
tation and other requirements.
Due to concerns about the proposed rule expressed by many states and numerous stakeholders, it was subject
to a Congressional moratorium that prohibited the Secretary of HHS from taking any action, including publica-
tion of a nal rule that was more restrictive with respect to coverage or payment for rehabilitative services than
the requirements in place as of July 1, 2007.
Before the expiration of the Congressional moratorium, the American Recovery and Reinvestment Act of 2009,
enacted on February 17, 2009, included a “Sense of Congress” that the Secretary should not promulgate a nal
regulation similar to the August 13, 2007 proposed regulation. In light of clear Congressional concern, as well as
the complexity of the underlying issues and of the public comments received, on November 23, 2009 CMS with-
drew the proposed rule in order to ensure agency exibility in re-examining the issues and exploring options
and alternatives with Congress and stakeholders.

100 Understanding Medicaid Home and Community Services: A Primer
they have a contract to furnish services under the
benet). Additionally, states must have safeguards
in place to ensure there is no conict of interest in
the needs assessment and service planning pro-
cesses.
States have the option to provide State Plan HCBS
to individuals with incomes up to 150 percent of
the Federal Poverty Level (FPL) who are eligible for
Medicaid under an eligibility group covered under
the State Plan without regard to whether they meet
institutional level-of-care criteria. They also have
the option of providing services to individuals with
income up to 300 percent of the SSI Federal benet
rate, but individuals in this new eligibility group
must be eligible for a §1915(c), (d), or (e) waiver
or §1115 demonstration program.
24
They do not,
however, have to be enrolled and receiving services
in either waiver program.
States may also make HCBS available to medically
needy people if they are covered under the State
Plan. For the medically needy group, states may ap-
ply income disregards to facilitate their eligibility for
HCBS benets (but not for other State Plan services).
States do not have the option to protect spousal in-
come and assets as they can under an HCBS waiver.
Community First Choice Option
The Aordable Care Act added §1915(k) to the
Social Security Act to allow states to provide
“Community-based Attendant Services and Sup-
ports”—called the Community First Choice Op-
tion—eective October 2011. Under §1915(k),
states that provide home and community-based
attendant services and supports through their State
Plans will receive a six percentage points higher
Federal match. To be eligible for this benet, indi-
viduals must meet Medicaid State Plan eligibility
criteria and have incomes that do not exceed 150
percent of the federal poverty level. If their income
is greater, they must meet institutional level-of-care
criteria.
Services under this option include home and com-
munity-based attendant services for the purpose of
assisting in “accomplishing activities of daily living,
instrumental activities of daily living, and health-
related tasks through hands on assistance, supervi-
sion, or cueing.” Funds can also be spent to provide
assistance with “the acquisition, maintenance, and
enhancement of skills necessary” for the individual
to accomplish such tasks; for “back-up systems or
mechanisms to ensure continuity of services and
supports (such as the use of beepers or other elec-
tronic devices)”; and for ‘‘voluntary training on how
to select, manage, and dismiss attendants.”
This option can also fund transition expenses
incurred when moving from an institution to the
community, such as security deposits for an apart-
ment or utilities, as well as basic kitchen supplies,
bedding, and other necessities required for transi-
tion. The law also allows “expenditures relating to a
need identied in an individual’s person-centered
service plan that increase independence or substi-
tute for human assistance, to the extent that expen-
ditures would otherwise be made for the human
assistance.”
Specic requirements for states that provide these
services and supports include the following:
• Collaborate with a Development and Imple-
mentation Council established by the state that
includes a majority of members with disabili-
ties, elderly individuals, and their representa-
tives.
• Establish and maintain a comprehensive con-
tinuous quality assurance system specically
for this service.
• Collect and report information for Federal over-
sight and the completion of a Federal evalua-
tion of the program.
For the rst full scal year in which the State Plan
amendment is implemented, the state must main-
tain or exceed the level of expenditures for services
provided under the State Plan, waiver programs, or
demonstrations.
101
Chapter 4: Options for Designing Service Coverage: General Considerations
Table 4-1. Texas Home and Community-Based Waiver Programs
Waiver Population Served
Medically Dependent Children
Program
Children (under age 21) at risk of nursing facility placement because of
complex medical needs.
Home and Community-Based
Services
People of all ages who qualify for ICF/ID services.
Community Living Assistance
and Support Services
People of all ages who have a disability—other than an intellectual
disability—that originated before age 22 and that aects their ability to
function in daily life.
Deaf-Blind Multiple Disabilities People age 18 or older who are deaf, blind, and have multiple disabili-
ties who qualify for ICF/ID/Related Conditions (RC) services.
Community Based Alternatives Adults (age 21 or older) who qualify for nursing facility services.
STAR+PLUS Adults (age 21 or older) who qualify for nursing facility services and live
in designated counties in the State. Services are provided through a
§1915(b) waiver and a §1915(c) waiver program.
Consolidated Waiver Program
Two waivers: One for ICFs/ID/RC
and one for nursing facilities.
People of all ages in Bexar County who qualify for nursing facility ser-
vices or ICF/ID/RC services.
Texas Home Living People of all ages, living with their families or in their own home, who
qualify for ICF/ID services and meet the SSI income limit.
Youth Empowerment Services Children between 3 and 18 years of age with Severe Emotional Dis-
turbance who qualify for a Hospital Inpatient Psychiatric Facility for
Individuals under 21 as provided for in 42 CFR 440.16.

102 Understanding Medicaid Home and Community Services: A Primer
Services That May Be Oered
Under an HCBS Waiver Program
25
Using the HCBS waiver as authorized under
§1915(c) of the Social Security Act, states have great
exibility to design programs that meet the unique
needs of individuals with disabilities. Collectively,
48 states and the District of Columbia operate 314
distinct HCBS waiver programs.
26
Some states, such
as Texas and Florida have 10 or more waivers for
specic populations (see Table 4-1 for a list of Texas’s
waiver programs).
To assist states in submitting requests to begin
waiver programs, CMS issued a standard HCBS
waiver application format in the early 1990s. Since
November 2006, CMS has oered a web-based ver-
sion of the application. Conversion to a web-based
application streamlined the preparation of waiver
applications and amendments, and improved
communication concerning waiver requests be-
tween CMS and the states. CMS encour ages states
to employ the web-based application to submit
new waivers, waiver renewals, and amendments.
The application is linked to specic instructions for
completing it and also includes technical guidance
regarding its use. (See the Resources section of this
chapter for a link to the latest version of the applica-
tion and accompanying instructions.)
The services a state may oer under the HCBS waiv-
er authority are not limited to those dened in the
waiver instructions and technical guidance. States
are free to accept the CMS denition, modify it to
reect other features and considerations important
to the state, and/or propose a new service entirely
and provide its denition. Many states use the CMS
denitions—often with modications—but many
others have proposed alternative denitions to
ensure that the service description exactly matches
the service they want to provide.
Because the CMS service denitions may not be
an exact match for what a state wants—and be-
cause CMS requires a precise denition of what will
be furnished to waiver participants
27
—it is best to
begin by developing a clear understanding of what
the state intends. This analysis should encompass
the types of services and supports to be delivered,
as well as how, where, and by whom. Gaining a
comprehensive understanding of its objectives puts
a state in a good position to decide how well the
denitions in the standard format “t.” A good rule
of thumb in considering CMS-predened coverage
is, “If it ts, use it. If it almost ts, change it to t. If it
doesn’t t at all, propose a new service.” See the Box
below for Colorado’s denition of Personal Assistant
Services provided under its Supported Living waiver
for people with developmental disabilities.
HCBS waivers cover many dierent services, includ-
ing protective services and home-delivered meals;
28
family counseling to deal with behavioral and other
problems; substance abuse counseling/services;
training in child and infant care for a parent with
a disability; crisis intervention services; behavioral
services, generally for individuals with developmen-
tal disabilities and acquired brain injuries; commu-
nity participation supports; and housing coordina-
tion to assist individuals in locating and obtaining
community housing.
The wide range of services makes it clear that no
exact formula exists for deciding which services and
supports to include in a particular HCBS waiver pro-
gram. States’ HCBS waiver programs dier in signi-
cant ways, but some of the large dierences among
the programs that serve similar target populations
are less signicant than meet the eye. Some states,
for example, elect to break down their services
into many distinct coverages, whereas others pull
together several closely related services into one
coverage category. For example, Colorado’s Sup-
ported Living Services waiver program for people
with developmental disabilities provides a service it
has named “Environmental Engineering,” which cov-
ers both home modications and assistive technol-
ogy. Other states choose to oer them as discrete
services. How exactly services and supports are
packaged and dened is less important than mak-
ing sure they are covered in one way or another.
Again, the best starting point for designing and
selecting HCBS waiver coverage is for the state to
assess the needs of the service population and
develop concrete ideas about how those needs can
best be met.
103
Chapter 4: Options for Designing Service Coverage: General Considerations
A more substantive reason why state waiver ser-
vices vary so widely is dierences among states in
the services already covered under the Medi caid
State Plan. In states that have broad, comprehen-
sive State Plan coverages, the services a state oers
under its HCBS waiver program will consist mainly
of those that cannot otherwise be covered under
the State Plan. This explains why, for example, some
states cover therapeutic services under their waiver
programs and others do not.
It also explains why HCBS waiver programs that
principally serve children usually oer fewer servic-
es than programs that principally serve adults with
disabilities. Because the EPSDT mandate requires
states to provide the full array of mandatory and
optional State Plan services to children, whether or
not they are actually covered under the State Plan,
HCBS waiver programs for children furnish a more
limited array of additional services.
Dierences among target populations may also
be important. As discussed earlier, several types of
waiver services cut across disability categories (e.g.,
personal care/personal assistance, service coordina-
tion, and home modications). These—and other
services—are needed by people with dierent
types of disabilities and are covered in nearly all
HCBS waiver programs.
However, there are also some dierences among
individuals that are linked to their disabilities and
how those disabilities need to be addressed. For ex-
ample, habilitation training is particularly important
for people with developmental disabilities, because
of the nature of their disability.
29
(Indeed, the provi-
sion of habilitation usually accounts for a signicant
share of the expenditures in HCBS waiver programs
that serve people with developmental disabilities
and is one reason why these waiver programs tend
to be relatively costly to operate.) However, habilita-
tion training is not relevant in meeting the needs
of most elderly individuals. Thus, state coverage
decisions are very much tied to the specic needs of
individuals in the target population.
Yet another substantive reason why states dier in
the services and supports they oer through their
HCBS waiver programs is that services and supports
Colorado Supported Living HCBS Waiver: Personal Assistant Services Denition
Personal assistant services provide necessary personnel and supports to meet the daily living needs of a person
with a developmental disability [on a less than 24-hour basis]. These services and supports, including evaluation
and assessment, are provided to ensure adequate functioning in the person’s own home, someone else’s home,
in the home of their natural or adoptive family, or for accessing and/or participating in the community.
Personal assistant services may include assistance or training with a wide range of activities necessary to meet
the daily living needs of the person in the home and community including
1. Personal care such as hygiene, bathing, eating, dressing, grooming, bowel and bladder care, menstrual care,
transferring, basic rst aid, giving medications, relief to a family who normally provides personal care, emer-
gency response in the form of human assistance, and operating medical equipment.
2. Household maintenance such as meal preparation, shopping and chores, assistance with money manage-
ment and personal nances, cleaning, laundry, and household repairs and maintenance related to the
person’s disability.
3. Mentorship activities such as planning; decision making; assistance with his/her participation on private
and public boards, advisory groups, and commissions; person-specic training costs associated with provid-
ing unique supported living services to an individual, such as training in child and infant care for parent(s)
who themselves have a developmental disability.
4. Supported living consultation such as assistance with decision making, planning daily activities, and direct
assistance to access community resources and/or service providers.

104 Understanding Medicaid Home and Community Services: A Primer
continue to evolve. Approaches that seemed appro-
priate in the past give way to new approaches, and
states vary in how quickly they adopt these chang-
es. One of the most useful features of the HCBS
waiver is that it is suciently exible to change over
time. States have considerable latitude to modify
and/or totally change their HCBS waiver coverages.
Each year, states submit numerous amendments
to their HCBS waiver programs, which add, delete,
and/or modify the services and supports states
oer. As a consequence, waiver programs that
have been in operation for a relatively long period,
usually have changed considerably since they were
rst approved. Coverages can be ne-tuned based
on feedback from waiver participants and service
providers concerning problems or gaps.
The “Application for a §1915(c) Home and Com-
munity Based Waiver [Version 3.5] Instructions,
Technical Guide and Review Criteria” has attached
to its instructions—in Appendix C—an excellent
description of and guidance on the service options
included in the HCBS waiver application format.
(See the Resources section of this chapter for a link
to the application and to a website where copies of
each state’s approved waiver applications are avail-
able.)
A Frequent Problem in Designing Waiver
Coverages: Tendency to Tie Them to Par-
ticular Service Settings
In designing HCBS waiver programs it is helpful
to remember that services can be furnished in
both the home and a wide range of community
settings. Historically, in developmental disabili-
ties services, states have tended to identify “day
habilitation” with particular sites. This has had
the eect of preventing habilitation services
from being furnished to individuals in everyday
community settings where training could be
used to assist the individual in mastering skills
important in community life. Several states are
now removing the ties of this service to specic
sites, and at least two states no longer oer
“facility-based” day programming.
Another example of problems that can be
caused by tying a service to a particular setting
can be found in the area of personal care/assis-
tance services. These services can be dened in
a way that ties their delivery to a person’s living
arrangement. But they can also be dened more
exibly, to permit their provision both in and
outside the home (as Michigan’s HCBS waiver
program for people with developmental disabil-
ities allows). Dened in this alternative fashion,
these services can be furnished more exibly
and more in accordance with an individual’s
specic needs and preferences.
105
Chapter 4: Options for Designing Service Coverage: General Considerations
HCBS Waivers for Adults with Serious
Mental Illness or Children with Severe
Emotional Disturbance
Some states provide services for adults with
serious mental illness and children with severe
emotional disturbance using §1915(c) waivers.
Colorado, Montana, and Wisconsin serve adults
using nursing facility level-of-care waivers. Indi-
ana, Kansas, Michigan, New York, Texas, Wiscon-
sin, and Wyoming provide services to children
and youth using the hospital level of care for
an inpatient psychiatric facility for individuals
under age 21, as provided in 42 CFR §440.160.
Supports Waivers
States are experiencing extremely high demand
for home and community services for people with
developmental disabilities. Many states, even those
that have substantially expanded their HCBS waiver
programs over the past decade, have very long
waiting lists for services.
30
Many factors account for
this high demand. One factor is the increasing lon-
gevity of this population, many of whom now live
with parents who themselves are elderly and less
able to meet the needs of their adult children.
31
A
second and related factor is that many people with
developmental disabilities outlive their parents.
As a consequence, many states are rethinking the
role that waiver services might play in meeting
the needs of people with developmental disabili-
ties—particularly with respect to increasing waiver
services and supports for individuals who live with
their families or have other informal caregivers who
provide support. While requests for services and
supports often take the form of families seeking a
group home placement, in-home and family sup-
port services can often meet individuals’ needs so
they do not have to leave the family home. States
that make services and supports more readily avail-
able to people with developmental disabilities who
live with their families, in fact, experience lower
demand for services in group homes and other
residential care settings.
33
States rethinking is taking various forms. Some
states have implemented distinct HCBS waiver
programs intended mainly to provide services and
supports to meet the needs of individuals who live
with their families or on their own, with either infor-
mal caregiving available to them or the capacity to
live without 24/7 supports. These programs do not
oer services in group homes and other residential
care settings that provide around-the-clock stang,
such as adult foster care.
These programs—called supports waivers—usu-
ally operate under stricter cost caps than the state’s
parallel HCBS waiver program, which covers service
in residential care settings, because the individu-
als being served have informal caregivers or less
intensive support needs. These caps enable the
state to avoid imposing service-by-service restric-
tions on utilization in order to maintain program
cost-eectiveness.
Supports waivers also permit the state to give
individuals and families considerable exibility in
selecting the mix of services and supports that best
meets their needs. However, unlike state-funded
family support programs, waiver services and sup-
ports must be for the direct benet of the waiver
participant. Although the HCBS waiver does allow
for services that support families to give care to a
family member with a disability, such as respite and
family training, services that are primarily for the
benet of the family can not be covered under a
Medicaid HCBS waiver.
The exibility aorded individuals and families also
permits states to reect many of the principles and
values under which developmental disabilities indi-
vidual support and family support programs have
operated for many years: namely, that the individual
or the family be in a position to ensure that the ser-
vices and supports they receive are tailored to meet
their needs and preferences.34
The availability of Medicaid funding allows states
to oer more comprehensive services and supports
to families than has typically been the case with
respect to state-funded family support programs,
many of which allot only $3,000 to $4,000 to a fam-
ily each year. Average annual expenditures per par-
ticipant for all HCBS ID/DD waivers for FY 2008 were
106 Understanding Medicaid Home and Community Services: A Primer
$43,464 per year.
34
In a study of 16 states’ supports
waivers in 2006, average annual participant expen-
ditures ranged from $4,015 to $24,443.
35
Operating distinct waiver programs that primarily
target individuals who live with their families has
both pros and cons. One of the main advantages
is that when creating a new program state ocials
and other stakeholders are often more willing to
consider new approaches to furnishing home and
community services than when modifying an exist-
ing program. Supports and services can be selected
that are especially relevant to meeting the needs of
people who live with their families, paying particu-
lar attention to those that can strengthen and sup-
port informal caregiving.
The main disadvantages appear to be (1)the ad-
ministrative complications associated with operat-
ing multiple HCBS waiver programs for the same
general target population, and (2)the CMS require-
ment that states safeguard participants’ health and
safety—even if their needs increase beyond what
can be addressed within the waiver service cap.
36
Supporting Individuals to Live in Their
Own or Family Home
In-home supports provide an alternative living
arrangement to provider-controlled residential pro-
grams. In-home supports are individually tailored
services that assist individuals to live in their own
home or in their family’s home. In-home supports
may comprise a variety of services such as residen-
tial habilitation, personal care, homemaker/chore
services, skills training, family training, respite, and
housing modications. In the past, in-home sup-
ports for individuals living in their own home (a
place they lease or own) were reserved for individu-
als deemed capable of “independent” living. The
model oered intermittent supports to individuals
who needed some assistance with activities of daily
living or some limited skills training or supervision
in order to live independently.
In the ID/DD eld, this model has changed dramati-
cally; even individuals who need around-the-clock
supports can now live in their own home. The op-
portunity to own or lease a home (or apartment) is
no longer reserved only for those individuals need-
ing minimal supports. Now, individuals live with
roommates and have either live-in or come-in sup-
port personnel to assist them. This type of arrange-
ment is often referred to as “supported living.” The
intensity, type, and frequency of supports are based
on the person’s needs and can be a combination of
support, supervision, and skills training based on
the person’s individual service plan.
For individuals living in their family’s home, similar
services can be brought in to assist the individual,
and other supports, such as respite and caregiver
training, can be made available to the family. These
supports help families to keep individuals in the
family home rather than seeking out-of-home
placement in facilities that are provider owned or
operated.
Medicaid Financing for Supports to
Individuals Living in Their Own Home
Supports for individuals living in their own or family
home can be nanced through the HCBS State Plan
benet, the HCBS waiver, or both. These supports
can be oered under the category of “residential ha-
bilitation.” States may also oer an array of in-home
supports. Common in-home supports include per-
sonal care, homemaker chore services, and respite
and training for informal caregivers.
37
Additionally, under the HCBS waiver, states have
the option of oering “live-in caregiver” payments
that cover services provided by an individual who
resides in the home of a waiver participant, and
also cover his/her room and board costs (see Box on
next page).
107
Chapter 4: Options for Designing Service Coverage: General Considerations
Factors to Consider When
Choosing Coverage Options:
Two Illustrative Services
Every state covers personal care and case manage-
ment in their Medicaid programs, either through
the State Plan, an HCBS waiver, or both. This section
will discuss the options for providing these two ser-
vices, highlighting the advantages and drawbacks
of each, which may vary by state depending on a
state’s conguration of its long-term care system, as
well as its policy goals.
1. Personal Care/Personal Assistance
The three major Medicaid options for covering
personal care (also called personal assistance) are
the Medicaid State Plan Personal Care benet, the
Medicaid State Plan HCBS benet, and an HCBS
waiver. States may also provide personal care under
the Community First Choice Option, authorized by
the Aordable Care Act, eective October 2011.
Thirty-four states and the District of Columbia cover
personal care under their Medicaid State Plans,
but only a few states make it broadly available.
For example, California, New York, and Texas oper-
ate relatively extensive State Plan Personal Care
programs; elsewhere, provision of such services is
more limited.
38
Many states that oer personal care
have strict limitations on its delivery. Some either
stringently regulate the amount of personal care
services an individual can receive or cap the dollar
value of such services at a level well below the an-
nual cost of nursing facility services.
39
Others limit eligibility for personal care services by
identifying a population or level of functional limita-
tion for which they will provide assistance. How-
ever, states must be careful not to violate Medicaid
comparability requirements by restricting services
to those with a particular diagnosis or condition,
such as by making benets available only to people
who use wheelchairs. All states are required to pro-
vide all §1905(a) services, including personal care,
to children under the expanded EPSDT mandate,
whether or not the state covers the service under its
State Plan.
HCBS Waiver Core Services Denition: Live-in Caregiver
Live-in Caregiver: An unrelated live-in personal caregiver who resides in the same household as the waiver
participant. Payment for this service includes the additional costs of rent and food that can be reasonably at-
tributed to the unrelated live-in personal caregiver. Payment will not be made when the participant lives in the
caregiver’s home or in a residence that is owned or leased by the provider of Medicaid services.
Under the HCBS waiver, states can elect to cover the costs of a live-in caregiver. These costs must be detailed in
the cost-neutrality formula in the HCBS waiver application and must be described as a discrete service in the
state’s waiver application. The Connecticut Department of Developmental Services (DDS) oers “live-in caregiv-
er” as a service under its HCBS waiver for individuals with developmental disabilities using the following deni-
tion: “DDS reimburses the waiver participant for the cost of the additional living space and increased utility costs
required to aord the live-in caregiver a private bedroom. The reimbursement for the increased rental costs will
be based on the DDS Rent Subsidy Guidelines and will follow the limits established in those guidelines for rental
costs. The reimbursement for food costs will be based on the United States Department of Agriculture Moderate
Food Plan Cost averages. Payment will not be made when the participant lives in the caregiver’s home or in a
residence that is owned or leased by the provider of Medicaid services.”
108 Understanding Medicaid Home and Community Services: A Primer
The principal reason why many states do not cover
personal care under the State Plan or, if they do,
impose considerable restrictions on its provision, is
concern about controlling expenditures for an en-
titlement benet. State ocials often want to know
(1)How many Medicaid beneciaries will qualify to
receive the service? (2)How many service hours will
they use once eligible? On the other hand, because
HCBS waivers permit states to cap the number of
beneciaries and the cost of services, most states
cover personal care or a similar service under an
HCBS waiver (or a §1115 waiver in Arizona and
Vermont.)
Personal Care and the Medicaid Home
Health Benet
Personal care is also provided by home health
aides under the mandatory Medicaid Home
Health benet. However, this benet is a very
costly way to provide personal care because it
is subject to the same rules regarding provider
conditions for participation as the Medicare
Home Health benet. Under these rules, agen-
cies must be Medicare certied and home
health aides must be supervised by a licensed
nurse. These requirements signicantly increase
the costs of a home health aide compared to
that of a personal assistant from a non-Medicare
certied agency and, of course, personal assis-
tants hired by Medicaid beneciaries who direct
their services.
It is important to note that the Medicaid Home
Health benet cannot use the same eligibility
criteria that Medicare uses, for example, requir-
ing that individuals need skilled nursing care or
be homebound. (See Chapter 3 for a more de-
tailed discussion of the Medicaid Home Health
benet.)
Advocates for personal care point out that this
service is usually less costly per person than in-
stitutional services and, consequently, that add-
ing this coverage will result in lower institutional
expenditures—by avoiding or delaying admission
of individuals to institutions, as well as enabling in-
stitutionalized persons to return to the community.
However, state ocials are often concerned that
such savings might be oset by the eect of more
people overall seeking services once their availabil-
ity becomes known (i.e., increased demand). The
costs of meeting the needs of more people could
oset the savings stemming from reduced nurs-
ing facility usage. Both are legitimate points and
the challenge for state policymakers and disability
advocates is to strike a balance between the need
to control costs and the need to provide home and
community services so that individuals can live in
the least restrictive setting.
Expenditure concerns, as noted earlier, have
prompted many states to turn to an HCBS waiver
program to secure Medicaid nancing of personal
care assistance services, since the waiver program
permits tighter cost and use limits. Table 4-2 sum-
marizes the dierences in personal care service
coverage between State Plan and HCBS waiver
programs.
Personal Care: Issues in Both State Plan and
Waiver Programs
Regardless of the Medicaid authority used, states
need to consider several issues related to the provi-
sion of personal care. Depending on how they are
addressed, these issues can either impede or facili-
tate its provision.
Delegation of Nursing Tasks
Certain health-related personal care tasks (e.g.,
medication administration and tube feeding) fall
under the jurisdiction of states’ Nurse Practice Acts.
Federal Medicaid policy does not dictate who must
perform skilled nursing tasks, merely that such tasks
be performed in compliance with applicable state
laws. But state laws and regulations often dictate
that such tasks be performed by or closely super-
vised by a licensed nurse, which can signicantly
increase the cost of serving individuals with medical
or health-related needs in the community.

109
Chapter 4: Options for Designing Service Coverage: General Considerations
To avoid duplicating Home Health benets already
available through Medicare or under the Medicaid
State Plan, many HCBS waiver programs do not oer
skilled nursing or rehabilitative therapies. However,
“skilled” paraprofessional services may still be pro-
vided by personal care workers under HCBS waivers
or under the State Plan Personal Care option—as
long as the services are provided in conformity with
the state’s Nurse Practice Act.
A 1999 Medicaid Manual transmittal specically
states that
Services such as those delegated by nurses or phy-
sicians to personal care attendants may be pro-
vided so long as the delegation is in keeping with
state law or regulation and the services t within
the personal care services benet covered under a
state’s plan. Services such as assistance with medi-
cations would be allowed if they are permissible in
states’ Nurse Practice Acts, although states need to
ensure that the personal care assistant is properly
trained to provide medication administration and/
or management.
40
This policy and its applicability to optional State
Plan personal care services and HCBS waiver pro-
grams were rearmed in a July 2000 letter from
CMS to State Medicaid Directors.
41
Several states, notably Oregon, have amended their
Nurse Practice Acts to enable licensed nurses to
delegate nursing tasks under specic conditions.
Others have amended their Nurse Practice Acts to
exempt certain individuals—such as participant-
directed personal assistants—from the provisions
of the Act, just as most Acts exempt unpaid family
members who perform these tasks.
Provider Qualications
States typically require individuals who would
provide personal care services to have completed a
basic training course. To ensure proper supervision
of personal care workers, some states require that
they be employed by agencies that hire the work-
ers and supervise them. More and more states are
routinely requiring individuals who would provide
personal care services to undergo criminal back-
ground checks and checks against abuse/neglect
registries.
With the increase in state options for participants
to direct their services, however, many states now
allow individuals to directly hire the persons they
want to provide services and to train and super-
vise them. States need to determine what provider
qualications will be required and, in so doing,
balance concerns about safety with participants’
ability to choose who they will hire. (See Chapter 7
for a detailed discussion of various service delivery
models for participant-directed services.)
Change in Medicaid Statute to
Increase Participant Direction Service
Delivery Options
Section 6087 of the DRA-2005 added §1915(j) to
the Social Security Act, eective January 2007.
43
This
authority permits states to prospectively disburse
cash to participants who direct their personal care/
personal assistance services using an individual
budget. States may not oer participant-directed
services under the §1915(j) authority except
through an existing State Plan Personal Care pro-
gram or an HCBS waiver program.
Absent the §1915(j) authority, participant direction
of Medicaid State Plan personal care is limited to
use of the employer authority. The §1915(j) author-
ity also allows states to permit participants who
direct their services under the State Plan Personal
Care option to use their individual budgets to pur-
chase non-traditional goods and services other than
personal assistance, to the extent that expenditures
would otherwise be made for human assistance.
(States already have the authority under §1915(c) to
allow HCBS waiver participants to purchase a broad
range of goods and services.)
Employing Family Members
All of the Medicaid authorities allow participants to
hire friends and relatives to provide personal care
services. States also have the option under the HCBS
waiver authority, and the §1915(j) and §1915(i)
authorities, to allow participants to hire legally
responsible relatives (i.e., spouses, and parents and
110 Understanding Medicaid Home and Community Services: A Primer
Table 4-2. Key Features of Medicaid Options for Covering Personal Care
Feature State Plan
Personal Care
HCBS Waiver State Plan HCBS
Entitlement States can not target
services by age or
diagnosis.
States must pro-
vide services to all
categorically eligible
individuals who
meet the eligibility
criteria.
Services must be
provided statewide.
States can target services
by age and diagnosis.
States can limit the num-
ber of people served.
States can limit the geo-
graphic area in which a
waiver program is avail-
able.
States can target services by
age and diagnosis.
States must provide services
to all individuals in an eligi-
bility group who meet the
eligibility criteria.
Services must be provided
statewide.
Financial
Criteria
Beneciaries must
meet community
nancial eligibility
standards.
States may set nancial
eligibility criteria up to
300 percent ($2,022 per
month) of the Federal
SSI benet ($674 per
month in 2010).
States may set nancial
eligibility criteria at 150 per-
cent of the FPL ($1,354 per
month in 2009) or at 300
percent of the Federal SSI
benet ($2,022 per month)
42
Eligibility
Criteria
Beneciaries must
have functional limi-
tations—specied
by the state—that
result in a need for
the services covered.
Beneciaries must meet
the minimum institu-
tional level-of-care crite-
ria and have a medical/
func tional need for the
specic service.
Beneciaries eligible under
150 percent of the FPL must
meet functional eligibility
criteria that is less stringent
than institutional level-of-
care criteria.
Beneciaries eligible under
the 300 percent of SSI
income eligibility standard
must meet institutional
level-of-care criteria.
Services Services include
only those specied
in the Federal deni-
tion of personal care
services.
Coverage can include
a very broad array of
state-dened services,
only some of which are
specied in statute.
Coverage can include a very
broad array of state-dened
services, only some of which
are specied in statute.
Payment of
Relatives
Relatives other than
legally responsible
relatives may be
paid to provide
personal care, at the
state’s option.
Relatives, including
those legally respon-
sible, may be paid to
provide personal care
and other services under
specic circumstances
determined by the state.
Relatives, including those
legally responsible, may be
paid to provide personal
care and other services un-
der specic circumstances
determined by the state.

111
Chapter 4: Options for Designing Service Coverage: General Considerations
legal guardians of minor children).
44
Generally, to be
a paid personal care provider, a legally responsible
relative has to be providing services that a parent
or spouse would not be providing for a non-dis-
abled spouse or minor child; for example, feeding
a 15-year-old child or bathing a spouse. However,
Medicaid still prohibits the hiring of legally respon-
sible relatives under the State Plan Personal Care
option.
Within the broad parameters of Federal policy, it is
up to states to dene the particular circumstances
under which relatives will be paid to furnish services
to participants. States can take various factors into
account, including the availability of other sources
for the same services, costs of using family members
to provide services versus costs of purchasing such
services from conventional sources, and specic
circumstances with respect to participants.
2. Case Management
Medicaid gives states three ways to cover case man-
agement services: (1)targeted case management,
(2)HCBS waiver programs, and (3) administrative
claiming.
45
This section discusses the advantages
and drawbacks of each option in obtaining Federal
nancial participation.
46
Some states cover case
management services under their HCBS waiver
programs and use the targeted case management
option for Medicaid beneciaries not receiving
waiver services. For example, some states cover case
management services in HCBS waiver programs for
adults and children with developmental disabili-
ties, and make targeted case management services
available to individuals who have been wait-listed
for the waiver services. Targeted case management
services can also be made available to people who
qualify for a state’s HCBS waiver program (in lieu of
providing such services under the waiver program),
as well as for individuals who do not participate in
the waiver program.
Targeted Case Management
Advantages to States of Oering Targeted
Case Management Services
• The state is free to dene the population that
will be targeted.
• The service may be oered to all Medicaid-
eligible persons who need home and commu-
nity services. Consequently, they may be made
available without regard to type of service or
funding source. This feature makes targeted
case management a potentially very useful
coverage option in establishing a broad-based
coordinated service system.
• The costs of targeted case management
services are claimed at the Federal Medical
Assistance Percentage, which in many states is
signicantly higher than the 50 percent match-
ing rate that applies to administrative claiming
(see below).47
• A problem for case management covered
under an HCBS waiver program is that FFP is
only available once the person has entered the
program. Thus, case management costs in-
curred in advance of enrollment are not eligible
for FFP unless they are covered under targeted
case management, administrative claiming,
or under the HCBS waiver if they are begun
before waiver participation but completed on
the rst day the person is enrolled in the waiver
program. However, targeted case manage-
ment services may be furnished irrespective
of whether the person is enrolled in an HCBS
waiver program, enabling most pre-enrollment
costs associated with service coordination to
be recouped.
• Once states were severely limited in obtaining
FFP for targeted case management services
furnished to residents of institutions. This
limitation arose from the concern that activities
performed for institutionalized persons by case
managers not on the facility sta would dupli-
cate activities facilities are required to conduct
on behalf of their residents.

112 Understanding Medicaid Home and Community Services: A Primer
• FFP is now available for targeted case man-
agement services to assist and arrange for
residents’ transition to the community for up
to 180 days preceding discharge. This policy
enables a state to involve case managers earlier
in the community placement process. FFP for
such targeted case management services is
available regardless of whether the person is
enrolled upon discharge in an HCBS waiver
program, receives other Medicaid home and
community services, or is supported through
alternative funding sources.48
• If the institutional resident does not transition,
FFP can be secured by charging the targeted
case management service as an administra-
tive expense. In this case, the activity must be
claimed as administrative case management,
which is reimbursed at the 50 percent match-
ing rate. (See Chapter 6 for a detailed discus-
sion of Medicaid coverage of transition servic-
es, and the Resources section of this chapter for
a link to a CMS State Medicaid Director Letter
regarding the earliest date of service for which
FFP can be claimed.)
• When the targeted groups are those with
serious mental illness or developmental dis-
abilities, targeted case management enables a
state to strictly limit who may be contracted to
provide case management services. This is ben-
ecial when service providers are to be limited
to the case management authorities already
established in state law, or where counties or
other local entities such as Community Centers
are responsible for the provision of case man-
agement services. It allows states to tie delivery
of targeted case management services into
their already established single point of entry
systems. In contrast, when case management/
service coordination is oered to these popula-
tions under an HCBS waiver program, Medicaid
freedom of choice of provider rules apply and
a state must allow HCBS waiver participants to
obtain case management/service coordination
from any qualied provider.
Drawbacks to States of Oering Targeted
Case Management Services
• Obtaining FFP for targeted case management
requires “service claiming” (i.e., claims for reim-
bursement for a specic service delivered to a
specic Medicaid recipient). Service claiming
can generate considerable paperwork. It can
also pose logistical problems in developing a
reimbursement mechanism that enables the
relevant authority to maintain base operation
levels when the amount of case management
varies individual-to-individual, month-to-
month. The varying workload problem also
arises when service coordination is oered as
a distinct service under an HCBS waiver pro-
gram.49
• The necessity for service claiming can also
make it dicult to obtain reimbursement for
activities conducted on behalf of all recipients
rather than distinctly for the benet of a spe-
cic individual (e.g., sta development activi-
ties for case managers). Costs used in the devel-
opment of the reimbursement rates must take
into consideration sta time spent in general
administrative activities such as intake, as well
as training and travel.
• Service coordinators often support individu-
als in ways that fall outside the scope of tar-
geted case management activities for which
FFP may be claimed. But, FFP for targeted
case management services is not available for
“direct services.” Examples are a case manager’s
driving an individual to a doctor’s appointment
(transportation) or helping the person manage
their nances. Federal policy dictates that such
direct services be claimed via other categories
(e.g., making a claim for Medicaid transporta-
tion services).50 Having to assign some of the
activities case managers routinely conduct on
behalf of individuals to other categories creates
administrative and billing complexity.

113
Chapter 4: Options for Designing Service Coverage: General Considerations
HCBS Waiver Coverage
FFP is available for the costs of case management
when a state covers such services under its HCBS
waiver program. This option diers little from tar-
geted case management with respect to types of
activities for which FFP may be claimed. The general
interchangeability of these options is illustrated by
the fact that all states operate HCBS waiver pro-
grams for people with developmental disabilities,
but states divide about equally between those that
use targeted case management coverage and those
that cover service coor dination as a waiver service.
Advantages to States of Covering Case
Management as a Waiver Service
• Covering case management as a waiver service
tightly links availability of such services to the
target population served through the HCBS
waiver program. Thus, the scope of such cover-
age may be tied directly to the specic needs of
the waiver population.
• Covering case management as a waiver service
enables a state to provide for more intensive
service coordination for HCBS waiver partici-
pants than it might (for nancial reasons) be
prepared to oer a wider range of individuals.
Drawbacks to States of Oering Case
Management as an HCBS Waiver Coverage
• The service is limited to individuals enrolled in
the HCBS waiver program.
• Under an HCBS waiver, a state may not limit
case management service providers to estab-
lished case management authorities for any-
one—including those with serious mental ill-
ness and developmental disabilities—as it can
under the targeted case management option.
• Claims for FFP may only begin once the person
has been approved for admission to the waiver
program. This prevents the state from being
reimbursed for pre-enrollment case manage-
ment expenses. However, some pre-waiver case
management costs may be covered if (a)they
are begun before waiver participation, but
completed on the rst day the person enrolls
in the waiver; or (b)they occur in the 180 days
preceding transition from an institution to the
community.
Administrative Claiming
Administrative claiming takes advantage of a provi-
sion in Federal law permitting states to claim FFP
for administrative expenses they incur in operat-
ing their Medicaid programs. Such expenses may
include costs of intake, assessment, service plan-
ning, arranging Medicaid services for recipients, and
overseeing service delivery—many of the activities
typically performed by case managers.
Administrative claiming diers from the targeted
case management and waiver alternatives in one
important aspect: It may not be used to assist recipi-
ents to access non-Medicaid services—even though
such services might benet them. Case managers
may work to coordinate access to all services in
a care plan. But administrative claiming can only
be used for the administration of the Medicaid
program, as established by a time study or other
method to apportion Medicaid and non-Medicaid
costs.
Advantages to States of Using the Adminis-
trative Claiming Option for Case Manage-
ment Activities
• It is not necessary to bill for distinct activities
on behalf of specic individuals, because ad-
ministrative claiming is not service-based. Ad-
ministrative claiming is usually accomplished
by apportioning the costs an organization
incurs between those attributable to
Medicaid recipients and those attributable to
non-recipients and/or other state or Federal
non-Medicaid programs. While the cost appor-
tionment process can be complicated, this does
not always constitute an additional barrier,
because some organizations must do cost ap-
portionment in any case whenever they receive
Federal funds for administering non-Medicaid
programs.

114 Understanding Medicaid Home and Community Services: A Primer
• Because administrative claiming does not have
a rule requiring states to contract with “any
qualied provider,” (as they must with State
Plan services) the state can limit which entities
can make an administrative claim for case man-
agement. This can be especially advantageous
for states that operate a single point of entry
system through human service authorities that
also administer the provision of non-Medicaid
benets. For example, some states use admin-
istrative claiming for a range of case manage-
ment functions that are not specically covered
under the case management service for waiver
beneciaries (e.g., eligibility determination; ad-
ministrative functions involving case managers
such as program planning, development, and
outreach; and certain licensing and contracting
functions).
• Administrative claiming is consistent with
models where a state has established, by law
or regulation, a distinct network of local single
point of entry/case management authorities.
The administrative claiming option for case
management activities provides states with
the capability of securing FFP for external
case management services furnished to insti-
tutionalized persons that does not hinge on
whether the person’s discharge from the facility
is imminent. Administrative claiming may be
employed to provide external oversight of the
well-being of institutionalized persons, as well
as to support “inreach” activities to provide in-
formation concerning the availability of home
and community services.
Administrative claiming may also span case
management activities that are directly tied to
arranging and assisting a person’s return to the
community—over and above that provided by
discharge planners—without respect to length
of time involved. However, such activities must
be tied to arranging Medicaid home and com-
munity services. The state
Medicaid agency may obtain case manage-
ment services for institutionalized persons via
contract with a state program oce or through
local human services agencies. Organizing
case management for institutionalized persons
under the administrative claiming option may
simplify use of Medicaid dollars to underwrite
such services in comparison to other available
service options.
Drawbacks to States of Using
Administrative Claiming for
Case Management Services
• Federal reimbursement of administrative
expenses is limited to 50 percent of allowable
costs. In states where the service rate is greater
than 50 percent, administrative claiming will
yield less FFP.
• Administrative claiming is limited to activi-
ties related solely to administration of a state’s
Medicaid program. Thus, the costs of activities
that assist individuals to access services not
available in a state’s Medicaid program, such
as housing, food, education, and employment,
will have to come from state/local dollars.
Alternatively, states can use the targeted case
management option to cover the activities
that relate to the consumer’s needs but do not
involve Medicaid services.
• Individuals lose the protections contained in
Medicaid law with respect to provider freedom
of choice, since administrative claiming usu-
ally restricts service coordination activities to a
single provider source.
115
Chapter 4: Options for Designing Service Coverage: General Considerations
States May Use One, Two, or All Three of the Case Management Authorities
Federal policy allows states to select the options or combinations of options that will be most eective in meet-
ing the needs of individuals and families with long-term care needs. Federal policy does prohibit states from
claiming the costs of the same activity of service coordination for the same individual under more than one al-
ternative at the same time. But as long as this prohibition is observed, a state can use the three options to serve
recognizably dierent purposes. For example, a state may combine service coordination as a distinct service for
participants under HCBS waivers with targeted case management services for Medicaid recipients not being
served by the waiver program. This allows the state to oer case management services under its State Plan that
are more limited in scope than those oered under an HCBS waiver.
Wyoming takes advantage of this possibility by oering targeted case management to individuals wait-listed
for waiver services, to help them connect with other sources of direct service assistance while awaiting waiver
coverage.
Sometimes a state may want to add administrative claiming to the case management mix. Although administra-
tive claiming may not be used to assist recipients in accessing non-Medicaid services, it has the advantage of
allowing FFP claiming for certain services that are not claimable under targeted case management or an HCBS
waiver—including outreach, quality assurance/quality improvement, operating automated data systems, and
various state-level administrative activities.
116 Understanding Medicaid Home and Community Services: A Primer
Resources
Since the Primer was rst published in 2000, numerous reports and other resources have become available
on the Internet. This section includes key resources relevant to service coverage. Most of the publications
cite additional resources and the websites also have links to other sources of information.
Publications
Centers for Medicare & Medicaid Services. (2008). Application for a §1915(c) Home and Community-Based
Waiver [Version 3.5]: Instructions, Technical Guide and Review Criteria.
This publication contains extensive information concerning Federal policies that apply to the operation of an
HCBS waiver, in particular, Appendix C: Participant Services, which includes core service denitions.
Available at https://www.hcbswaivers.net/CMS/faces/portal.jsp under links and downloads, entitled §1915(c)
Waiver Application and Accompanying Materials.
Smith, G., Fortune, J., Agosta, J., and O’Keee, J. (2007). Gauging the Use of HCBS Supports Waivers for
People with Intellectual and Developmental Disabilities: Proles of State Supports Waivers. Washington, DC:
U.S. Department of Health and Human Services, Oce of the Assistant Secretary for Planning and Evalua-
tion, Oce of Disability, Aging and Long-Term Care Policy.
This project was funded to (a)gather descriptive information on HCBS waivers, both comprehensive and
supports, operated for people with intellectual and developmental disabilities in 17 states with the supports
waivers; (b)determine how supports waivers have emerged as separate and distinct HCBS waivers; (c)better
understand the range of participant characteristics and experiences that distinguish supports waivers from
other HCBS waivers; and (d)more fully appreciate how states view supports waivers as a way to address de-
mand for home and community services among people with developmental disabilities.
Available at http://aspe.hhs.gov/daltcp/reports/2007/gaugingfr.htm
Smith, G., Kennedy, C., Knipper, S., O’Brien, J., and O’Keee, J. (2005). Using Medicaid to Support Working
Age Adults with Serious Mental Illnesses in the Community: A Handbook. Washington, DC: U.S. Department of
Health and Human Services, Oce of the Assistant Secretary for Planning and Evaluation, Oce of Disabil-
ity, Aging and Long-Term Care Policy.
This Handbook focuses on working-age adults between the ages of 21 and 64 with serious mental illnesses,
whose need for support extends beyond mental health services that can be eectively provided by primary
care physicians or periodic visits to outpatient settings. It is designed to improve understanding and provide
greater clarity concerning Medicaid’s contribution in supporting working-age adults with serious mental ill-
117
Chapter 4: Options for Designing Service Coverage: General Considerations
nesses in the community.
Available at http://aspe.hhs.gov/daltcp/reports/handbook.htm
Summer, L.L., and Ihara, E.S. (2005). The Medicaid Personal Care Services Benet: Practices in States that Oer
the Optional State Plan Benet. Washington, DC: AARP, Public Policy Institute.
This paper reports on the eligibility requirements, characteristics of beneciaries, program expenditures, types
of services, and methods of service delivery in 26 states (and the District of Columbia) that oered the optional
Medicaid Personal Care Services benet in 2004. The site includes both the full version and a brief summary.
Available at http://www.aarp.org/health/medicare-insurance/info-2005/2005_11_medicaid.html
CMS: State Medicaid Director Letter (July 25, 2000). Olmstead Update No: 3.
This letter discusses a policy change regarding the earliest date of service for which Federal nancial participa-
tion can be claimed, and explains some of the ways that Medicaid funding may be used to help people of all
ages with disabilities and chronic illnesses transition from an institution to a community residence.
Available at http://www.cms.gov/smdl/downloads/smd072500b.pdf
Websites
CMS: Medicaid State Waiver Programs and Demonstration Projects
The Social Security Act authorizes multiple waiver and demonstration authorities to allow states exibility in
operating Medicaid programs. Each authority has a distinct purpose, and distinct requirements. This site pro-
vides information about these authorities and includes information about state-specic
Medicaid waiver and demonstration programs. Users can access fact sheets, copies of proposals, approval let-
ters, and other documents related to specic programs.
Web address: http://www.cms.hhs.gov/MedicaidStWaivProgDemoPGI/01_Overview.asp
The following site contains approved waiver applications for each state. Clicking on a specic state on the map
will lead to a site with a list of all of the state’s approved waiver applications with links to view them.
118 Understanding Medicaid Home and Community Services: A Primer
Web address: http://www.cms.hhs.gov/MedicaidStWaivProgDemoPGI/%2008_WavMap.asp
CMS: The State Medicaid Manual
The State Medicaid Manual makes available to all state Medicaid agencies informational and procedural
material to administer the Medicaid program. The material is organized into major parts, which are divided
into chapters and sections. (Chapter 4 is about Services.) The manual is structured as closely as possible to the
codication of Medicaid regulations. A crosswalk of manual sections and regulations is also included.
Web address: http://www.cms.gov/Manuals/PBM/itemdetail.asp?lterType=none<erByDID=-99&
sortByDID=1&sortOrder=ascending&itemID=CMS021927&intNumPerPage=10

119
Chapter 4: Options for Designing Service Coverage: General Considerations
Endnotes: Citations, Additional Information,
and Web Addresses
1
Gary Smith and Janet O’Keee co-authored the original chapter. Janet O’Keee, Ernest McKenney, and
Robin Cooper updated the chapter.
2
States may also use §1115 Research and Demonstration waivers to provide long-term care services, as
do Arizona and Vermont.
3
Sections 1902(a)(10)(B) and 1902(a)(1) of the Social Security Act.
4
Section 1915(c) of the Social Security Act. The relevant Federal statute authorizes the Secretary of
Health and Human Services to grant these waivers. Medicaid also provides other options for targeting
services to specic groups, including the targeted case management benet and various managed
care authorities, and most recently, the §1915(i) authority.
5
State Medicaid Director Letter, August 6, 2010. Available at http://www.cms.gov/SMDL/SMD/itemde-
tail.asp?lterType=none<erByDID=0&sortByDID=1&sortOrder=descending&itemID=CMS1238355&
intNumPerPage=10.
6
For example, it is increasingly common for states to oer, under HCBS waiver programs for people
with developmental disabilities, supplementary dental services over and above the dental benets
available under the State Plan, which are typically very limited. This “extended” coverage option can be
and is employed for other Medi caid State Plan services as well, such as rehabilitation therapies, vision
services, and prescription drugs.
7
Exceptions include targeted case management services, among others.
8
Connecticut Home Care Program for Elders. Information available at http://www.ct.gov/dss/cwp/view.
asp?a=2353&q=305170 and http://www.ct.gov/dss/lib/dss/documents/fee-for-servicechcp_xls.xls.
9
These services are listed in §1905(a) of the Social Security Act.
10
Adding or changing coverage of home and community services that Federal law permits to be cov-
ered under the Medicaid State Plan requires a state to take various formal steps. A state adds, deletes,
or changes a service in its Medicaid State Plan by ling a State Plan amendment with CMS, which
reviews the coverage and approves it if it conforms to Federal law and regulations.
11
Section 1905(a)(24) authority.
12
The 1997 regulations can be found at 42 CFR 440.167.
13
This state option was added in §1915(g) of the Social Security Act.
14
CMS guidelines concerning targeted case management services are in Sections 4302 et seq. of the
State Medicaid Manual. See the Resources section of this chapter for a web link to the manual.
15
Activities related to eligibility determinations and service authorization may be reimbursed as admin-
istrative expenses.

120 Understanding Medicaid Home and Community Services: A Primer
16
States are required to ensure that appropriate transportation is available. See the transportation provi-
sions in 42 CFR 431.53. Transportation may also be provided as a service under the State Plan.
17
Dened in 42 CFR 440.90 with additional CMS guidelines in §4320 of the State Medicaid Manual.
18
Dened in 42 CFR 440.130(d).
19
Teaching parents to anticipate and deal with a child’s rage is an example of an activity that directly
supports the Medicaid beneciary. Marriage counseling for the child’s parents does not and is not
covered.
20
Much of the information provided here on the Rehabilitation benet is drawn from Koyanagi, C. and
Brodie, J. (July 1994). Making Medicaid Work to Fund Intensive Community Services for Children with
Serious Emotional Disturbances. Washington, DC: Bazelon Center for Mental Health Law. This publi-
cation is no longer available because it has been updated and re-published as two new reports. The
reports are available for purchase at the
Bazelon Center’s website at http://www.bazelon.org/News-Publications/Publications/CategoryID/20/
List/1/Level/a/ProductID/51.aspx?SortField=ProductNumber%2cProductNumber and at: http://www.
bazelon.org/News-Publications/Publications/List/1/CategoryID/20/Level/a/ProductID/32.aspx?SortFiel
d=ProductNumber%2cProductNumber.
21
No data are available to determine how many states oer targeted case management to a specic
group.
22
Information about the §1915(i) authority is from the State Medicaid Director Letter, August 6, 2010.
http://www.cms.gov/SMDL/SMD/itemdetail.asp?lterType=none<erByDID=0&sortByDID=1&sortOr
der=descending&itemID=CMS1238355&intNumPerPage=10.
23
P.L. 109–171, Section 6086(a).
24
Eligibility for a §1915(c) waiver requires that an individual meets the state’s institutional level-of-care
criteria.
25
Statutory authority for HCBS waiver programs is contained in §1915(c) of the Social Security Act. Ap-
plicable Federal regulations are found at 42 CFR 441 Subpart G. These regulations were last modied
in 1994. CMS guidelines concerning HCBS waiver programs are contained in Sections 4440 et seq. of
the State Medicaid Manual. These guidelines are updated periodically.
26
Eiken, S., and Burwell, B. (2009). Medicaid HCBS Waiver Expenditures: FY 2003 through FY2008.
Cambridge, MA: Thomson Reuters. Available at http://www.hcbs.org/moreInfo.php/doc/2795.
27
With respect to services a state proposes to cover that depart from those that appear in the waiver
application, the denition of each waiver service must describe goods and services in concrete terms,
along with any conditions that apply to the provision of the service. The denition of a service cannot
use terms such as “including but not limited to . . .,” “for example . . .,” “including . . .,” or “etc.” CMS will not
approve vague, open-ended, or overly broad service denitions. The service must be dened in a man-
ner to make it clear exactly what will be furnished to the beneciary.
28
Although Medicaid cannot pay for food, services such as home-delivered meals and the provision of a
meal and snack in adult day health settings are reimbursable because they do not constitute a com-
plete daily diet. (Core service denition. Attachment to the Instructions to Appendix C for the HCBS
Waiver Application, Version 3.5. See the Resources section of this chapter for a web link to the applica-

121
Chapter 4: Options for Designing Service Coverage: General Considerations
tion and instructions.)
29
Persons of all ages with many dierent types of disabilities can benet from habilitation services.
Coverage of habilitation has generally been provided only to people with developmental disabilities,
which are dened as those occurring before age 22. However, a CMS letter to State Medicaid Directors
claries that neither Medicaid law nor implementing regulations restrict who may receive habilitation
services in an HCBS waiver. Individuals who do not have an intellectual disability or other develop-
mental disabilities, such as persons with traumatic brain injury or physical disabilities that occurred
after age 22, may also receive habilitation services through a waiver program.
30
Smith, G. (1999). Closing the Gap: Addressing the Needs of People with Developmental Disabilities
Waiting for Supports. Alexandria, VA: National Association of State Directors of Developmental Dis-
abilities Services.
31
Among individuals with developmental disabilities who live with their families, about 25 percent live
with parents who themselves are older than 60.
32
Smith, G. (1999). Serving and waiting: An update. In A Supplement to Closing the Gap: Addressing the
Needs of People with Developmental Disabilities Waiting for Supports. Alexandria, VA: National Asso-
ciation of State Directors of Developmental Disabilities Services.
33
This type of HCBS waiver program is sometimes called a middle-range program, because it lls the
gap between limited state-funded family support programs and HCBS waiver programs intended
mainly to buy specialized group home and similar residential services.
34
The average is based on the average daily HCBS waiver census. Lakin, K.C., Larson, S., Salmi, P., and
Scott, N. (2009). Residential Services for Persons with Developmental Disabilities: Status and Trends
through 2008. Minneapolis, MN: University of Minnesota, Research and Training Center on Community
Living. Available at http://rtc.umn.edu/risp08. Print copies may be requested by contacting Naomi
Scott at [email protected] or 612-624-8246.
35
Smith, G., Agosta, J., Fortune, J., and O’Keee, J. (April 2007). Gauging the Use of HCBS Supports Waiv-
ers for People with Intellectual and Developmental Disabilities: Final Project Report. Washington, DC:
U.S.
Department of Health and Human Services, Oce of the Assistant Secretary for Planning and Evalu-
ation, Oce of Disability, Aging, and Long-Term Care Policy. Available at http://aspe.hhs.gov/daltcp/
reports/2007/gaugingfr.htm.
36
While states must safeguard health and safety under all waivers, it becomes more dicult in a waiver
that has a cap that is well below what comprehensive waivers permit. Caps in supports waivers tend to
be in the $15-25,000 range and the state must be able to ensure health and safety whatever the cost.
If a waiver participant’s needs increase but there is no opportunity to move to another waiver and
the person does not want to go to an ICF/ID, the state must supplement the services solely with state
dollars if the person is to stay enrolled on the supports waiver. The lower cap poses issues, particularly
when individuals need only a modest increase above the cap, because for cost containment reasons
the state does not want to enroll them in the comprehensive waiver, which opens up the service
menu and can lead to much greater increased costs (e.g., residential services instead of in-home sup-
ports).
37
The §1915(j) authority may also be used to provide supports to people in their own home.

122 Understanding Medicaid Home and Community Services: A Primer
38
Among the states that oered personal care services in 2008, annual per capita outlays for such ser-
vices (i.e., total personal care expenditures divided by the state’s total population) ranged from less
than $0.10 to a high of $151.02. Burwell, B., Sredl, K., and Eiken, S. (2009). Medicaid Long-Term Care Ex-
penditures in FY 2008. Cambridge, MA: Thomson Reuters. Available at http://www.hcbs.org/moreInfo.
php/doc/2793. (A few of the states included in the data analysis cover personal care services only for
children covered by the EPSDT mandate, which likely accounts for the very low amount spent in some
states.)
39
The limits each state imposes are listed in U.S. General Accounting Oce. (May 1999) Adults with Se-
vere Disabilities: Federal and State Approaches for Personal Care and Other Services. GAO Publication
No. GAO/ HEHS-99-101. Washington, DC: GAO.
40
Health Care Financing Administration Medicaid Manual Transmittal Part 4, No. 73, September 17, 1999.
41
State Medicaid Director Letter: Olmstead Update Number 3. July 25, 2000. Available at http://www.
cms.hhs.gov/smdl/downloads/smd072500b.pdf.
42
For the rst time since the Federal Poverty Level (FPL) guidelines began to be issued in 1965, the an-
nual average Consumer Price Index has decreased from the gure for the previous year. Therefore, the
Department of Health and Human Services poverty guidelines have been frozen until at least May 31,
2010 at 2009 levels in order to prevent a reduction in eligibility for certain means-tested programs,
including Medicaid, Supplemental Nutrition Assistance Program, and child nutrition. Additional infor-
mation is available at http://aspe.hhs.gov/poverty/09extension.shtml.
43
The text of §1915(j) is located at http://www.paelderlaw.com/pdf/DRA_Provisions.pdf.
44
They may also do so under a §1115 waiver.
45
Case management activities are also covered routinely as a component of another service. For ex-
ample, home health agencies that provide home health services are required to perform certain case
management activities.
46
The amount of FFP for services is called the Federal Medical Assistance Percentage, which cannot
exceed 83 percent or go below 50 percent. The FFP for administrative claiming is 50 percent.
47
The cost of HCBS waiver case management services can also be claimed at the service rate.
48
States can recoup the costs of service coordination furnished to individuals returning to the communi-
ty through the HCBS waiver program when the person is enrolled in the HCBS waiver after discharge.
As with targeted case management services, FFP is available for service coordination furnished during
the 180-day period preceding institutional discharge. These service coordination activities are consid-
ered completed when the person enrolls in the waiver program.
49
Solutions exist for this problem, but they can involve their own complications.
50
To the extent that driving a beneciary to a doctor’s appointment is necessary, it could be paid for as a
Medicaid State Plan service rather than as a targeted case management service. The person’s case
manager may certainly transport the individual to a physician’s appointment. Although the costs
involved cannot be claimed as case management (because the service is direct), they may be reim-
bursed as a transportation service under the Medicaid State Plan, or as an administrative expense.

Chapter 5: Providing Medicaid Services in Community Residential Settings
123
Guide to Chapter 5
Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .125
Denitions and Terminology . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .126
Major Types of Residential Care Settings in Which Medicaid Services May be Provided . . .127
Adult Foster Care . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .127
Child Foster Care . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .128
Residential Care Facilities . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .131
Older Adults and Younger Adults with Physical Disabilities . . . . . . . . . . . . . . . . . . . . . .131
Adults with Developmental Disabilities . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .132
Medicaid Financing for Services in Residential Care Settings . . . . . . . . . . . . . . . . . . . . . . . . . . . .132
Which Authority to Use . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .134
Considerations When Using the HCBS Waiver Authority . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .134
Level-of-Care Criteria and State Regulation of Residential Care Facilities . . . . . . . . .137
Target Population . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .137
Licensing and Contracting Issues . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .137
Enabling Medicaid Beneciaries to Pay for Room and Board . . . . . . . . . . . . . . . . . . . . . . . . . . . .138
Limiting the Amount Facilities Can Charge for Room and Board . . . . . . . . . . . . . . . . .138
Providing State Supplements to the SSI Payment . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .139
Using the 300 Percent of SSI Standard and Providing an
Adequate Personal Maintenance Allowance . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .139
Income Supplementation by Family Members or Trusts . . . . . . . . . . . . . . . . . . . . . . . . .140
Eect of Medically Needy Rules on the Ability to Pay for Room and Board . . . . . . .142
Service Payment Rates: Adequacy Concerns . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .143
Bundling Payments . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .143
Resources. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .144
Endnotes: Citations, Additional Information, and Web Addresses . . . . . . . . . . . . . . . . . . . . . . .147
125
Chapter 5: Providing Medicaid Services in Community Residential Settings
Chapter 5
Providing Medicaid Services in Community Residential Settings
This chapter provides guidance to states about selecting coverage options for services in a wide range of residential
care settings that are provider owned and/or operated, encompassing foster care, group homes, and residential
care facilities, including those called assisted living. When a state is faced with dierent ways of covering services,
the tasks of choosing among the coverage alternatives and dening the precise services to be provided in specic
settings require a detailed analysis of each alternative in the context of a state’s broader service system.1
Introduction
To reduce institutionalization—particularly for individuals who lack housing or cannot be served cost eec-
tively in their own or a family member’s home—states oer services in residential care settings. This chapter
deals with the provision of Medicaid services only in provider-owned and/or -operated residential care set-
tings that are not institutions.
Using Medicaid to pay for services in residential care settings is of interest to states that want to decrease
expenditures on institutional care. Compared to Medicaid-covered institutions—nursing homes, intermedi-
ate care facilities for persons with intellectual disabilities (ICFs/ID), hospitals, and some inpatient psychiatric
facilities
2
—residential care settings have the potential to be more homelike and to provide residents greater
autonomy and privacy. Compared to services delivered in individuals’ homes, they may also oer economies
of scale as well as the opportunity for socialization.
For many individuals with disabilities and chronic illnesses—such as individuals with dementia who need con-
siderable supervision but little nursing care—residential care settings can provide an alternative to institution-
alization. The populations a state chooses to serve in these settings, much like the mix of facilities, depends on
the state’s overall long-term care system and specic policy goals.
Residential care settings can be owned and/or operated by either individual service providers or agencies of-
fering around-the-clock services. The level of sta support typically relates to the needs of residents as well as
applicable state regulations. Sta are employed on either a live-in or come-in basis.
3
They provide assistance
with activities of daily living (ADLs), and help individuals to gain access to community activities. Depending
on state regulations, individuals may share rooms or may have private rooms and share common public areas
(dining and living rooms, and sometimes kitchens).
The size of residential care settings varies widely. In the system serving individuals with an intellectual disabil-
ity or other developmental disability (ID/DD, hereafter referred to as developmental disabilities), some residen-
tial care settings may have more beds than a community ICF/ID.
4
Although Medicaid regulations that apply
to the provision of services in residential care settings do not specify an upper size limit for these settings, the
Centers for Medicare & Medicaid Services (CMS) denes “larger” facilities as settings serving four or more unre-
lated individuals.
5
CMS reviews proposed waiver services in residential care settings to ensure that
A home-like character is maintained in larger settings, that is, the facility is community-based, provides an
environment that is like a home, provides full access to typical facilities in a home such as a kitchen with cooking
facilities, small dining areas, provides for privacy, visitors at times convenient to the individual, and easy access to
resources and activities in the community.
6
126 Understanding Medicaid Home and Community Services: A Primer
Residential care settings and the services they
provide are governed by state law and regula-
tions, which vary greatly across states. They can be
licensed or certied, or in some instances have only
to meet Medicaid requirements if serving Medic-
aid-eligible persons. States typically license these
settings, performing annual reviews to ensure that
they meet required standards. Some states choose
to use national accreditation bodies to qualify
providers, in lieu of or in addition to state stan-
dards. While some states license particular settings
to serve specic populations (e.g., older adults or
individuals with developmental disabilities), some
states, such as Minnesota, license facilities to serve
many dierent populations. See Box for Minnesota’s
denition of a Group Home.
Settings licensed to serve more than one popula-
tion may choose to serve only one in order to tailor
services to meet their needs—and most do. Addi-
tionally, if serving participants in Section (§)1915(c)
Medicaid home and community-based services
(HCBS) waivers (hereafter referred to as HCBS
waivers), these settings will also have to meet the
standards approved under the waiver for serving
this population and be able to serve residents who
meet institutional level-of-care criteria. Settings
serving specic populations, such as individuals
with dementia and those with developmental dis-
abilities, may have specic licensing requirements
to ensure that they have the specialized competen-
cies needed to serve these populations.
Minnesota’s Denition of Group Homes:
Group Residences for Adults with Dis-
abilities
Group Residences for Adults with Disabilities are
dened as “Agency-owned or -operated facilities
that provide an alternative living environment
for adults with developmental disabilities, sen-
sory impairments, physical disabilities, emo-
tional problems, multiple disabilities, or chronic
illnesses such as AIDS, who are in need of
personal services, supervision, and/or assistance
essential for self-protection or for sustaining the
ADLs, and consequently are unable to live with
their own families or in a more independent set-
ting. Group residences for adults with disabili-
ties may be licensed by the State/province and
may be distinguished according to the level of
service residents require. Service levels depend
on the self-care skills residents possess, their
limitations in the areas of physical coordination
and mobility, and the presence and extent of
behavior problems, including disruptive or self-
injurious behavior.”
7
There are no applicable Federal statutes regarding
licensing or certication standards for residential
care settings other than §1616(e) of the Social
Security Act (the Keys Amendment), which requires
states to set their own standards for residences
where “a substantial number of Supplemental Se-
curity Income (SSI) recipients” reside.
8
If states wish
to use Medicaid HCBS waivers to fund services in
residential care settings, as discussed in more detail
below, CMS requires as a condition of approval that
they describe how they will ensure compliance with
§1616(e).
Denitions and Terminology
The service systems for dierent populations use
very dierent and sometimes contradictory terms
to describe non-institutional provider-operated resi-
dential care settings. In the service system for older
adults and younger adults with physical disabilities,
the generic terms traditionally used for these set-
tings are foster care and residential or congregate
care. Consumer preference for the assisted living
model of residential care—which provides both
privacy and autonomy—has led providers to market

127
Chapter 5: Providing Medicaid Services in Community Residential Settings
all types of residential care settings as assisted liv-
ing—whether or not they provide private units or
operate with a service philosophy that ensures resi-
dent autonomy. Thus, assisted living has become a
generic term for many dierent types of residential
care settings for older adults.
9
Because states regulate residential care settings,
the terms they use for them vary considerably. For
example, states use 31 dierent names for adult
foster care, including adult family home, family care
rest home, adult residential care home, elder group
home, and assisted living establishment, to name
but a few.
In the service system for people of all ages with
developmental disabilities, the generic term resi-
dential settings includes the entire range of living
options: institutions (ICFs/ID), provider-owned and/
or -operated facilities such as group homes, foster
care, a family member’s home, and a person’s own
home. The ID/DD system also uses the term com-
munity residential program, which may include
both community (i.e., small) ICFs/ID as well as group
homes. As with the aging services system, states
have hundreds of dierent names for ID/DD resi-
dential programs, including residential habilitation
facilities, group residences, or residential treatment
facilities, among others.
The enormous variability in the terms states use for
the same or similar residential care settings can cre-
ate considerable confusion. Therefore, this Primer
will use the terms dened in the Box below.
Major Types of Residential Care
Settings in Which Medicaid
Services May be Provided
Three major types of residential care settings that
are provider owned and/or operated furnish long-
term care services and supports to persons of all
ages with disabilities and/or chronic illnesses: adult
foster care, child foster care, and residential care
facilities.
Denitions of Residential Care Settings
Residential care settings. A generic term
encompassing all types of state-regulated
(licensed or certied) foster care and residen-
tial care facilities, regardless of their size or the
population they serve.
Foster care. A home owned or rented by an
individual or family in which they live and in
which they provide care and support for one
or more unrelated persons. Depending on
the state, these homes can serve up to 6 or 8
residents, but typically serve 1 to 3 residents. (In
a few states, corporations own and/or operate
settings licensed as foster homes and provide
stang 24 hours-a-day.) Foster care providers
can serve adults or children.
Residential care facility. A building or resi-
dence—other than a foster care home—owned,
rented, or managed by the service provider, or
the provider’s agent, to provide housing, ser-
vices, and supervision. This term includes many
types of facilities—from group homes serving
as few as 2 or 3 individuals with developmental
disabilities to board and care homes or assisted
living facilities serving 100 or more older adults.
When referring to residential care settings in
specic states, the Primer will use the terms
these states use.
Adult Foster Care
Adult foster care is typically provided in a private
home, oering 24-hour support to one or more
individuals. Most commonly the support is provided
by the owners of the home, although foster care
providers may engage other individuals to provide
care. In some states, corporate entities oversee and
manage foster homes. States may contract with
each primary caregiver for the provision of adult
foster care services, and/or contract with agencies
that, in turn, contract with and supervise individual
caregivers. In addition to room and board, foster
care providers typically furnish assistance with daily
living activities and help in accessing community
activities.
128 Understanding Medicaid Home and Community Services: A Primer
Denition of Adult Foster Care in HCBS
Waiver Application
“Personal care and supportive services (e.g.,
homemaker, chore, attendant care, companion,
medication oversight [to the extent permitted
under state law]) provided in a licensed (where
applicable) private home by a principal care pro-
vider who lives in the home. Adult foster care is
furnished to adults who receive these services in
conjunction with residing in the home. Separate
payment is not made for homemaker or chore
services furnished to a participant receiving
adult foster care services, since these services
are integral to and inherent in the provision of
adult foster care services.”
10
States may use this denition, or modify or
supplement it to reect the scope of adult foster
care to be furnished through a waiver program.
Adult foster care homes serve individuals with a
wide range of disabilities, including those with
physical and/or cognitive impairments, serious
mental illness, and developmental disabilities.
Arizona, Maine, Oregon, Washington, and Wiscon-
sin, among other states, oer adult foster care as
a means to keep older adults connected to their
home communities when they can no longer live
alone. Oregon has made eorts to recruit and train
foster care providers for older adults specically to
increase the viability of this option as an alternative
to nursing homes.
11
Most foster homes serve a relatively small number
of individuals. As an example, in 2007, of the 23,848
family foster homes serving individuals with devel-
opmental disabilities, only 652 served four or more
individuals, with the maximum number nationally
being six individuals.
12
In an HCBS waiver program,
adult foster care is considered a residential habili-
tation service for individuals with developmental
disabilities only when habilitation is included in
the dened scope of the adult foster care service; it
is not considered a residential habilitation service
when habilitation services are furnished in the adult
foster care setting by a dierent provider and billed
separately.
Adult foster care settings usually are licensed or
certied; 17 states regulate these settings for older
adults under assisted living regulations.
13
States
have exibility in setting provider standards but
most require specialized training to support specic
populations, such as adults with developmental dis-
abilities and older adults with dementia.
Child Foster Care
The provision of Medicaid services for children in
foster care settings is permissible, typically through
an HCBS waiver program. The waiver application
does not include a denition for child foster care—it
is subsumed under the waiver service called “resi-
dential habilitation” (see Box), as are group homes
(discussed below).
14
Denition of Residential Habilitation in
HCBS Waiver Application
“Residential habilitation means individually
tailored supports that assist with the acquisi-
tion, retention, or improvement in skills related
to living in the community. These supports
include adaptive skill development, assistance
with ADLs, community inclusion, transportation,
adult educational supports, social and leisure
skill development, that assist the participant to
reside in the most integrated setting appropri-
ate to his/her needs. Residential habilitation also
includes personal care and protective oversight
and supervision.”
The method by which the costs of room and
board are excluded from payment for residential
habilitation is specied in Appendix I-5 of the
Waiver application.
15
Children’s foster homes are often the private homes
of individuals licensed by the state to provide care
to one child or a few children. These homes may
serve children who are placed voluntarily or those
under state protection. In either case, the home
must meet the state’s licensing criteria. When foster
homes serve “special” populations such as children
with developmental disabilities, some states require
providers to have training above and beyond what
is required for a general foster care license. Children
with serious emotional disturbances (SED) may also
129
Chapter 5: Providing Medicaid Services in Community Residential Settings
be served in child foster care. Detailed information
about services for children with SED is the subject
of a separate publication listed in the Resources sec-
tion of this chapter.
Payments under the HCBS waiver cannot supplant
funding under Title IV-E of the Social Security Act
(hereafter called the Act) that pays for the basic
foster home care and services for children in state
custody. Waiver services to children in foster care
can only supplement the basic services that must
be covered under Title IV-E. According to Title IV-E
regulations, “Foster care maintenance payments are
payments made on behalf of a child eligible for Title
IV-E foster care to cover the cost of (and the cost of
providing) food, clothing, shelter, daily supervision,
school supplies, a child’s personal incidentals, liabil-
ity insurance with respect to a child, and reasonable
travel for a child’s visitation with family, or other
caretakers.”
16
The HCBS waiver application instructions note that
Waiver services may be furnished to children in
foster care living arrangements but only to the ex-
tent that waiver services supplement maintenance
and supervision services furnished in such living
arrangements and waiver services are necessary
to meet identied needs of children. Waiver funds
are not available to pay for maintenance (includ-
ing room and board) and supervision of children
who are under the state’s custody, regardless of
whether the child is eligible for funding under Title
IV-E of the Act. The costs associated with main-
tenance and supervision of these children are
considered a state obligation. The costs associated
with the treatment of these children may be Med-
icaid reimbursable [under either the State Plan or
an HCBS waiver]. Depending on the nature of the
treatment (i.e., habilitation), the costs of treatment
may be eligible for Federal nancial participation
under a waiver.
17
Utah and Wisconsin, among other states, cover fos-
ter care services under an HCBS waiver for children
with “exceptional needs” (i.e., those requiring inten-
sive assistance due to medical or behavioral support
needs). See Box for Utah’s pro-visions pertaining
to coverage of residential services under an HCBS
waiver for children in foster care.
Moving from Adult Foster Care to Shared Living Arrangements
To better support individuals with developmental disabilities, new, more personalized approaches to adult
foster care are being used, such as Shared Living. The purpose of Shared Living is to create a more equal arrange-
ment than is found in traditional foster care—one based on mutual choice. In Shared Living, the individual with
a disability and the provider choose to live together. Although the provider furnishes support and supervision,
the expectation is that the relationship is more equal and more personal than is typically the case in foster care.
A Shared Living arrangement is usually in the Shared Living Provider’s home or apartment, but could also be in
the home or apartment of the individual with a disability, in which case it would be considered a home-based
supports approach. Many dierent arrangements can be developed based on individuals’ unique needs and
situation.
A human services agency in Pennsylvania serving individuals with developmental disabilities oers a foster care
approach called Lifesharing Thru Family Living. This approach provides an option for people with developmental
disabilities to be active, participating members in a family and the community in which the family lives. This ap-
proach emphasizes the importance of matching individuals and families to enable harmony in values, interests,
and mutual commitments. Family Living Specialists work closely with the family and the individual, and serve
as the primary support to ensure a successful match. For more information, see http://www.skillsofcentralpa.
org/public/services/lifesharing.php
130 Understanding Medicaid Home and Community Services: A Primer
Utah’s HCBS Waiver Denition of Residential Services for Children in Foster Care
To ensure compliance with CMS payment requirements, Utah has established a prior authorization process and
criteria to determine if children in foster care have exceptional needs that can be supported though the HCBS
waiver program. In its approved HCBS Residential Services denition, Utah notes that, “For children in the cus-
tody of the Division of Child and Family Services (DCFS), the costs of basic and routine support and supervision
are not covered as waiver services. Compensation for this routine support and supervision is covered by other
funding sources associated with the DCFS. Children in DCFS custody are eligible to receive this service only after
the provision of this service has been prior-authorized by the minor’s support coordinator. Such prior-authoriza-
tion will occur only after it has been determined that the minor has exceptional care needs that materially aect
the intensity or skill level required of the service provider.”
Utah denes a variety of medical and/or behavioral conditions that would qualify a child for this exceptional
payment including, among other conditions, “… emotional or behavioral needs such as hyperactivity; chronic
depression or withdrawal; bizarre or severely disturbed behavior; signicant acting out behaviors; or, the minor
otherwise demonstrates the need for 24-hour awake supervision or care in order to ensure the safety of the
minor and those around him/her.”
The exceptional care criteria also includes a variety of medical needs, such as ostomy care or catheterization;
tube feeding or supervision during feeding to prevent complications such as choking, aspiration or excess
intake; frequent care to prevent or remedy serious conditions such as pressure sores; suctioning; assistance in
transferring and positioning throughout the day; two or more hours of therapy per day; assistance with multiple
personal care needs including dressing, bathing and toileting; complex medical treatment throughout the day;
or, the minor has a complex and unstable medical condition that requires constant and direct supervision.
Utah further species that, “This service is intended to accomplish a clearly dened set of outcomes associated
with the child’s habilitation that is outlined in their individual support plan. Services provided under this service
denition are only those that are over and above the basic routine supports provided for through the DCFS.”
18
131
Chapter 5: Providing Medicaid Services in Community Residential Settings
Residential Care Facilities
For individuals who live in residential care facili-
ties—whatever their age or type of disability—in
order to receive waiver services, the facility must
be specically included as a setting for service
provision in the state’s waiver program. As noted
earlier, states must have licensure, certication, or
some other standards for their operation, including
required provider qualications and methods to en-
sure facility oversight and monitoring. States must
include a description of these standards and pro-
vider qualications in the HCBS waiver application.
19
HCBS waiver requirements include “portability,” that
is, the service funding is an individual benet for the
beneciary and is not tied to the facility; individu-
als can move from one type of setting to another
as their needs change. States may also use the
State Plan Personal Care optional benet to pro-
vide personal care in these facilities, as does North
Carolina. However, Medicaid personal care services
cannot duplicate or replace services that are part of
the residential care facilities’ existing service pack-
age. They can only be used to supplement existing
services.
Older Adults and Younger Adults with
Physical Disabilities
For older adults, until the introduction of the private
pay assisted living model in the late 1980s, the most
frequently used general term for residential care
settings other than foster care was board and care.
The new assisted living model diers signicantly
from traditional board and care. According to three
of the major assisted living industry trade associa-
tions, privacy and exible services that will meet
residents’ needs and allow them to age in place are
key elements of the assisted living philosophy.
20
The
new assisted living model of residential care be-
came popular with older adults because it oered
what nursing homes and traditional board and care
facilities generally do not: privacy and control over
one’s daily activities. Another reason for its popu-
larity is that assisted living facilities—many built
in the 1990s—have much more desirable physical
environments than do most board and care facilities
and nursing homes, many of which were built in the
1960s and 1970s.
21
Due to the popularity of the private pay model of
assisted living, many operators of board and care
homes and other types of residential care settings
believe they will be put at a competitive disadvan-
tage if they cannot market themselves as “assisted
living.” Consequently, under pressure from the
residential care industry, most states have amended
their statutes to rename domiciliary care homes,
board and care homes, and even adult foster care,
as assisted living.
22
Today, virtually all residential
care settings for older adults market themselves as
assisted living despite the fact that some provide
few services and the physical character of a substan-
tial portion of these settings is quite institutional,
with two to four persons sharing a bedroom, and as
many as 8 to 10 residents sharing a bathroom.
23
This general use of the term assisted living is also
found in the HCBS waiver application, which uses
the term assisted living services to cover a wide
range of services that can be provided in residential
care settings. However, in its guidance, CMS encour-
ages states to use a “more accurate name,” noting
that the term assisted living describes a setting,
not a service and that Medi caid never pays for as-
sisted living in the ordinary sense of a monthly fee
to the facility for room, board, and services. Rather,
Medicaid may cover, as a waiver service, some of
the supportive services provided to beneciaries in
residential care settings.
24
Core Denition of Assisted Living
Services in the HCBS Waiver Application
Personal care and supportive services (home-
maker, chore, attendant services, meal prepara-
tion) that are furnished to waiver participants
who reside in a homelike, non-institutional
setting that includes 24-hour on-site response
capability to meet scheduled or unpredictable
resident needs and to provide supervision,
safety, and security. Services also include social
and recreational programming, and medication
assistance (to the extent permitted under state
law). Nursing and skilled therapy services are
incidental rather than integral to the provision
of assisted living services. Payment is not made
for 24-hour skilled care.

132 Understanding Medicaid Home and Community Services: A Primer
CMS guidance notes that when a waiver includes
“assisted living services,” the locations of service
delivery must meet criteria described in Appendix
C-2 of the HCBS waiver application with regard to
the “home-like” character and community integra-
tion of the facility.
25
On June 22, 2009, CMS issued
an advance notice of proposed rulemaking in the
Federal Register to solicit comments about den-
ing standards for what constitutes “home-like” and
“community” under HCBS waivers.
Adults with Developmental Disabilities
The most common type of residential care facility
serving adults with developmental disabilities is the
group home. Group homes are generally operated
by agencies that both own the settings and provide
the support sta assisting the residents.
Based on the state’s policy goals and the interests
and preferences of stakeholders, group homes may
also be made available to other populations, such as
children with developmental disabilities or serious
emotional disturbances. As with adult and child fos-
ter care, waiver services provided in group homes
and other residential care facilities for persons with
developmental disabilities are subsumed under the
waiver service category of residential habilitation.
CMS provides a general denition of residential
habilitation but states have the exibility to adopt
this suggested denition or create a completely
dierent denition crafted to suit the state’s services
system and array of settings.
26
States may establish highly specialized group
homes to serve specic populations, such as indi-
viduals with autism spectrum disorders, intensive
medical support needs, or challenging behaviors.
These specialized settings may have additional
requirements, such as specialized training, and
may receive additional reimbursements due to the
nature of the services provided.
Medicaid Financing for Services
in Residential Care Settings
27
Medicaid provides several authorities for nancing
services in residential care settings: HCBS waivers,
28
Section 1115 research and demonstration waivers
(hereafter referred to as §1115 waivers), and the
Medicaid State Plan. State Plan services include
personal care (through the Personal Care optional
benet), rehabilitation services, and services oered
under the §1915(i) HCBS benet, including personal
care and habilitation services. Each of these Med-
icaid authorities has specic eligibility, application,
and approval requirements. (See Chapters 1 and 4
for more information about all of these authorities.)
However, Medicaid will pay for services furnished in
residential care settings only if a “homelike environ-
ment” is preserved. Thus, Medicaid will not pay for
services in residential care settings if they are lo-
cated in the wing of a nursing home or an ICF/ID. As
discussed earlier, CMS has provided guidance as to
what constitutes a home-like character, particularly
in regard to what CMS denes as “larger” facilities—
those serving four or more unrelated individuals.
States may provide HCBS waiver services only in
residential care settings that are permitted under
state regulations to serve individuals who meet
institutional level-of-care criteria. Some states, such
as Oregon, license both adult foster care providers
and residential care facilities to serve persons who
meet the state’s nursing home level-of-care crite-
ria. Others, such as North Carolina, use the State
Plan Personal Care option to provide personal care
services to individuals in residential care settings,
because these facilities are not permitted to serve
individuals who meet the nursing home level-of-
care criteria. Some states use both the HCBS waiver
and State Plan Personal Care option to provide
services in dierent types of settings.

133
Chapter 5: Providing Medicaid Services in Community Residential Settings
In 1981, Oregon was the only state to use the HCBS
waiver authority to fund services in residential care
settings for older adults. Few states followed suit
until the 1990s, when the growth in private pay
assisted living focused attention on residential care
alternatives to nursing homes. In 2009, 46 of the
50 states and the District of Columbia used either
a waiver or State Plan optional services (or both)
to provide services in residential care settings for
older persons and/or younger persons with physical
disabilities.
29
Table 5-1 lists the states that use each
authority for these populations. The HCBS waiver is
the most frequently used authority and the largest
source of nancing for Medicaid services in residen-
Table 5-1. Medicaid Authorities States Use to Provide Services in Residential Care
Settings for Older Adults and Younger Adults with Physical Disabilities
Waiver Only
1
State Plan State Plan and Waiver
Alaska
Arizona (§1115)
California (AL)
Colorado
Connecticut (AL)
Delaware (AL)
District of Columbia
Georgia
Hawaii (§1115)
Illinois (AL)
Indiana
Iowa
Kansas
Maryland
Mississippi (AL)
Minnesota
Montana
Nebraska
Nevada (AL)
New Hampshire
New Jersey
New Mexico
North Dakota
Ohio (AL)
Oklahoma
Oregon
Rhode Island (AL and §1115)
Tennessee
Texas
Utah
Virginia (AL)
Wisconsin
Wyoming (AL)
Maine
Massachusetts
Michigan
New York
North Carolina
South Carolina
Arkansas (AL)
Florida (AL and BW)
Idaho
Missouri (AL)
2
South Dakota
Vermont (§1115)
Washington
AL: Waiver services are provided only in residential care settings (13 states). §1115: Services covered
under a §1115 waiver (4 states).
1
Unless indicated as an §1115 or AL waiver, the states provide coverage under a broad HCBS waiver
(BW) that covers services in participants’ homes and in residential care settings (24 states and the
District of Columbia).
2
Missouri’s waiver was approved by CMS but had not been implemented by the end of 2009.

134 Understanding Medicaid Home and Community Services: A Primer
tial care settings, but more individuals in residential
care settings receive personal care services through
the State Plan than through an HCBS waiver.
Only four states use a §1115 waiver to cover ser-
vices in residential care settings for older adults and
younger adults with disabilities, and no states cur-
rently use the new §1915(i) HCBS authority for this
purpose, although it is possible to do so as several of
the services under this authority (e.g., personal care
and habilitation) can be provided in such settings.
From the inception of the waiver program in 1981,
states have used HCBS waivers to pay for services for
individuals with developmental disabilities in group
homes and foster homes as an alternative to ICFs/ID.
As a result, every state now uses the HCBS waiver (or
a §1115 waiver as in Arizona and Vermont) to provide
services and supports in residential care settings for
individuals with developmental disabilities. No states
use the State Plan Personal Care option to cover per-
sonal care in residential care settings for this popula-
tion because this benet is very limited compared to
residential habilitation services provided under HCBS
waivers.
Because all states use HCBS waivers—and none use
the State Plan Personal Care option—to cover ser-
vices and supports in residential care settings for
persons with developmental disabilities, the follow-
ing discussion regarding which Medicaid authority to
use focuses primarily on considerations when serving
older adults and younger adults with physical dis-
abilities. However, the discussion regarding consid-
erations when using HCBS waivers is also relevant for
the ID/DD population.
Which Authority to Use
The most common choice states face with regard
to covering services in residential care settings is
whether to use an HCBS waiver program, the State
Plan Personal Care option, or both. The primary factor
that will determine whether a state can use an HCBS
waiver is whether a state’s residential care settings are
permitted to serve a population that meets institu-
tional level-of-care criteria—nursing home or ICF/
ID. States that have several dierent types of facilities
serving dierent populations—those who meet insti-
tutional level-of-care criteria and those who do not—
may choose to use the waiver authority to nance
services in one type of residential care setting and the
State Plan Personal Care option in another.
For facilities serving individuals who meet nursing
home level-of-care criteria, the HCBS waiver authority
is advantageous in that states can broaden eligibility
by using the 300 percent of SSI income rule to reach
persons in the community who do not meet Med-
icaid’s community nancial eligibility criteria. (The
300 percent rule is explained later in this chapter and
in detail in Chapter 2.) The HCBS waiver also oers
states considerable exibility in dening the scope
and array of services to be provided as there are no
statutory denitions for services. However, since
waiver services are available only to beneciaries who
meet the state’s nursing home or ICF/ID level-of-care
criteria, serving people through a waiver will target
a more severely impaired population than can be
served through the State Plan Personal Care option.
Because states may set limits on the number of bene-
ciaries who can be served through waiver programs,
waivers also oer the advantage of predictable costs,
particularly for states concerned about utilization of a
new benet for older adults. The combination of insti-
tutional level-of-care eligibility criteria, a set number
of slots, and expenditure caps that are part of the cost
neutrality formula required for CMS approval will limit
the number of people potentially eligible.
The Boxes below contain examples of how two
states—North Carolina and Oregon—use dierent
Medicaid authorities to provide services in residential
care settings.
30
Considerations When Using the HCBS
Waiver Authority
The three factors that are important for states consid-
ering the HCBS waiver authority are discussed next.
135
Chapter 5: Providing Medicaid Services in Community Residential Settings
Coverage of Assisted Living through the Personal Care Benet: North Carolina
North Carolina covers personal care in adult care homes as a Medicaid State Plan service.
31
Target Population. Adult care homes serve adults of all ages with all types of disabilities, including developmen-
tal disabilities and those caused by mental illness. They are not licensed to serve individuals who need a nursing
home level of care. There are two types of adult care homes: those that serve all populations and those that
serve only persons age 65 or older. Adult care homes are divided into dierent types based on size—family care
homes for 2-6 residents and adult care homes for 7 or more residents.
Services. Adult care homes are required to provide three meals a day, transportation, activities, and housekeep-
ing services. The Medical Care Commission may limit what medical and functional care needs can be met in
adult care homes; for example, medication may be administered by designated, trained sta but nursing ser-
vices can only be provided by the residence on a case-by-case exception basis approved by the State’s Depart-
ment of Health and Human Services, or through licensed home care agencies. Unless a physician determines
otherwise, adult care homes may not serve people who are ventilator dependent or who require continuous
licensed nursing care.
Payment. The payment includes a at rate for basic personal care services with add-ons for residents with
specic ADL impairments. Residents with extensive or total impairments in eating, toileting, or both eating and
toileting qualify for a higher rate. In 2009, the basic payment was $17.50 a day for facilities with 30 or fewer beds
and $19.17 for facilities with more than 30 beds. The additional daily rate for residents with extensive or total im-
pairments in eating was $10.80 and in toileting was $3.86. Additional payment for residents needing assistance
with ambulation/locomotion was $2.76 a day. Eligibility for the additional payment is based on an assessment
by the adult care home, which is veried by a county case manager. (The State has a generous SSI state supple-
ment, which is added to the SSI Federal benet to cover room and board charges for residents of adult care
homes: $579 in 2009.)
136 Understanding Medicaid Home and Community Services: A Primer
Coverage of Assisted Living through the Waiver Program: Oregon
Oregon uses an HCBS waiver to cover multiple services in residential care settings. Two settings are licensed:
assisted living facilities and residential care facilities. The State has two classes of RCFs: Class I facilities provide
only ADL assistance. Class II RCFs oer a range of services and can serve people who need a nursing home level
of care. The Medicaid waiver program covers services in ALFs and Class II RCFs.
ALFs and Class II RCFs can serve the same population. When Oregon rst decided to regulate assisted living,
it chose not to replace existing RCF rules. Instead, it added a new licensing category for assisted living with
requirements that diered somewhat from its RCF rules. The State has since consolidated many requirements for
RCFs and ALFs, but maintains separate requirements for living units. The State does not allow providers to market
themselves as assisted living unless they oer residents private apartments and are licensed as assisted living.
Target Population. The waiver program serves adults age 18 or older. Individuals at risk of nursing home
placement and assisted living residents who were formerly private pay but who have spent down and become
eligible for Medicaid are given priority for assisted living services. Rather than set specic medical or functional
criteria governing when a resident is no longer appropriate for assisted living, Oregon’s regulations permit dis-
charge when the facility can no longer meet the resident’s needs or there is a “documented established pattern”
of noncompliance with the resident agreement.
32
Setting. The primary dierence between RCFs and ALFs is the physical setting. RCFs provide single or double
rooms with shared baths; individual kitchens are not required. ALFs must oer individual apartments with lock-
able doors, kitchen facilities, and private baths.
Services. Services provided by RCFs and ALFs include three meals a day and snacks, personal and other laundry
services, a program of social and recreational activities, assistance with ADLs, medication administration, and
household services (cleaning and bed making). Facilities must also provide or arrange for social and medical
transportation and ancillary services for related medical care (physicians, pharmacy, therapy, podiatry).
Payment. The Medicaid rate pays for the services ALFs provide under the licensing requirements. There are
ve levels of ALF payments based on residents’ acuity, which are based on a service priority score determined
through an assessment. The monthly payment rate in 2009 for level 1 was $1,002 and for level 5 was $2,355.
Medicaid also pays for services for persons living in Level II RCFs who meet the nursing home level-of-care crite-
ria. In 2009, the RCF base service rate for all clients was $1,249 per month. Depending on impairment level, there
are three add-on payments. The base payment plus one add-on was $1,491; base plus two add-ons was $1,733;
base plus three add-ons was $1,975. The add-on is based primarily on individuals’ need for assistance with ADLs.

137
Chapter 5: Providing Medicaid Services in Community Residential Settings
Level-of-Care Criteria and State Regulation
of Residential Care Facilities
HCBS waiver regulations require that any facility
in which waiver services are furnished must meet
applicable state standards regarding provider
qualications and methods to ensure oversight and
monitoring of the facilities. As noted above, states
must include a description of these standards and
provider qualications in the HCBS waiver applica-
tion.
33
When services are furnished by a residential
care facility, it must meet the standards for service
provision that are set forth in the approved waiver
documents.
Thus, states planning to cover services in residen-
tial care facilities through an HCBS waiver program
need to be sure that the admission and retention
provisions of state licensing or certication require-
ments permit facilities to serve individuals who
meet Medicaid’s nursing home or ICF/ID level-of-
care criteria. Licensing must also address a facility’s
qualications to provide the services needed by
Medicaid beneciaries.
States that use a waiver program to provide ser-
vices in residential care settings need to contract
with facilities that are willing and able to provide
the services needed by individuals who meet the
state’s Medicaid nursing facility level-of-care criteria,
which—if stringent—may be extensive.
Target Population
When determining which population to serve in
residential care settings, states need to consider
their policy goals and their current long-term care
system. Questions to ask include the following: Is
the new coverage intended to ll a gap in the cur-
rent set of options? Will the target population be
dierent from the population usually served in the
state’s residential care facilities? Is the new coverage
intended to enable people who cannot be served in
their homes to avoid institutionalization?
Once these questions are answered, the state must
decide which age groups will be served—those age
65 or older or younger adults with physical disabili-
ties, or both—and whether services will be de-
signed to address the specialized needs of specic
populations, for example, persons with dementia or
individuals with acquired brain injuries. It is crucial
to make certain that the state’s licensing and other
facility regulations match the needs of the target
population. As noted above, if the state wants to
target nursing home-eligible beneciaries, the
facilities need to be licensed or certied to serve a
population with a nursing home level of need.
When determining the target population for an
HCBS waiver serving individuals with develop-
mental disabilities, states may combine the entire
eligible population into one HCBS waiver, or may
choose to craft “specialty” waivers that target
specic populations, such as children or individu-
als with autism. At least seven states have separate
HCBS waivers serving individuals with autism. States
may choose to target waivers to specic sub-groups
within a larger population of eligible individuals as a
means to oer special ized and/or dierent services
to the sub-groups. The choice to use multiple waiv-
ers targeting distinct sets of eligible individuals is of
course related to state policy goals.
Licensing and Contracting Issues
State licensing rules set the minimum requirements
for Medicaid providers; for example, state regula-
tions may establish certain sta-to-resident ratios
or may specify awake overnight sta. However, the
Medicaid program may set more stringent stan-
dards if desired. For example, if licensing rules do
not include sucient provider requirements for resi-
dential care settings that serve people with demen-
tia, Medicaid contracting requirements may specify
additional training or other requirements. Similarly,
while a state may allow residential care facilities to
oer rooms shared by two, three, or more residents,
the Medicaid programs can choose to contract only
with facilities that oer private occupancy unless
the resident chooses to share a room or unit.
In states that are considering covering services in
“assisted living” facilities for older adults, it is im-
portant to recognize that “assisted living” can mean
more than just a setting for potentially cost-eec-
tive service delivery. It can refer to a philosophical
approach to residential care that supports privacy,
autonomy, and consumer choice. States that want
138 Understanding Medicaid Home and Community Services: A Primer
to oer residential care services that comport with
the assisted living philosophy will need to ensure
that their regulations and payment policies support
its basic tenets, most notably privacy and autono-
my. Several states do so—including North Dakota,
Oregon, and Washington—by requiring residential
care facilities that call themselves “assisted living,”
and want to contract with Medicaid, to oer apart-
ment-style units rather than bedrooms.
34
Enabling Medicaid Beneciaries
to Pay for Room and Board35
Medicaid beneciaries with limited income may
not be able to aord the room and board rates in
residential care settings, unless states take specic
steps to make them aordable. As noted earlier,
Medicaid pays for room and board only in institu-
tions, except in limited circumstances, for example,
when providing respite care. For Medicaid pur-
poses, room and board comprises real estate costs
(debt service; building maintenance, upkeep, and
improvements; utilities; and taxes) and food.
36
The
costs of preparing, serving, and cleaning up after
meals can be covered as a waiver service.
37
Although Medicaid beneciaries are responsible for
paying for room and board, states have a range of
options to help make the costs aordable.
Limit the amount facilities can charge Medicaid
clients for room and board to the Federal SSI ben-
et, which in 2010 is $674 per month minus a small
personal needs allowance.
Provide a state supplement to the SSI payment for
persons living in residential care settings, and limit
the amount these settings can charge to the com-
bined SSI plus state supple ment payment.
Use the 300 percent of SSI standard for HCBS waiver
eligibility, and set the maintenance allowance at
a level that allows residents to retain sucient
income to pay for room and board.
Allow family supplementation to increase the funds
available for room and board, particularly to pay the
dierence in cost between a shared and a private
room.
Each of these options is discussed below.
Limiting the Amount Facilities
Can Charge for Room and Board
States can limit the amount that can be charged
for room and board by setting a combined “rate”
for Medicaid beneciaries that includes service
costs and room and board costs, but the state only
pays for services. This approach essentially caps the
room and board rate that Medicaid beneciaries
pay. Other states simply limit by policy the amount
that facilities can charge Medicaid beneciaries for
room and board, usually capping the charge at the
Federal SSI payment for a single elderly beneciary
living in the community, plus a state supplemental
payment (SSP), if any. See Box below for a list of
states that limit room and board charges.
23 States That Limit Room and Board
Charges to the SSI/SSP Benet Level in
One or More Residential Care Settings
Arizona
California
Colorado
Delaware
District of Columbia
Georgia
Hawaii
Illinois
Indiana
Maine
Maryland
Montana
Nebraska
New Jersey
North Dakota
Ohio
Oklahoma
Oregon
South Carolina
Tennessee
Texas
Vermont
Washington
This approach guarantees that Medicaid benecia-
ries can aord room and board costs in facilities that
accept Medicaid. However, if providers feel that the
room and board rate is too low to cover costs, they

139
Chapter 5: Providing Medicaid Services in Community Residential Settings
may decide not to admit Medicaid beneciaries.
New Jersey has passed a law requiring that facilities
licensed after September 2001 set aside 10 percent
of their units to serve Medicaid residents within 3
years after licensing.
Providing State Supplements to
the SSI Payment
To increase access to residential facilities for SSI ben-
eciaries in areas with high housing costs, states can
create a special SSI state supplement for residents in
these facilities, and limit what providers may charge
to the amount of the Federal payment plus the state
supplement.
38
Many states have such SSP programs
to supplement the Federal SSI payment, which in
2010 is $674 a month; the payment is adjusted each
January based on the cost of living index. Individual
states may use a specic term to refer to their sup-
plement, and some use the term SSI to refer to both
the Federal payment and any state supplement.
States may pay dierent supplements based on
a person’s living arrangement. A few states have
developed a supplemental payment rate speci-
cally for SSI recipients in residential care facilities
to increase the amount of income they have to pay
for room and board. State supplements are totally
state-determined and vary widely. In 2009, the SSI
state supplement payment standards (including the
Federal payment of $674) ranged from $722 and
$735 a month in Vermont and New Hampshire, re-
spectively, to $1,275 a month in Hawaii and $1,350
in one area of Virginia.
39
Some policymakers might question the scal bene-
t of providing 100 percent state funding for a state
supplement to enable residents to pay for room and
board. However, it is important to consider the net
state cost for services provided in a residential care
facility rather than a nursing home.
40
If the program
diverts people from nursing homes or allows nurs-
ing home residents to move to a residential care
facility, states may be able to fund a fairly substan-
tial supplement to the Federal SSI payment and still
reduce their net cost. To determine if such a policy
would be budget neutral, states would have to de-
termine the number of people who would receive
the increased supplement and the combined cost
of the supplement and Medicaid services provided
in residential care settings.
Using the 300 Percent of SSI Standard and
Providing an Adequate Personal Maintenance
Allowance
States have the option to use more liberal income-
eligibility criteria for the waiver program—up to
300 percent of the Federal SSI payment—$2,022 per
month in 2010. (This option is discussed in detail in
Chapter 2.)
This option is attractive for HCBS waiver programs
that cover services in residential care settings, be-
cause it expands the program to include benecia-
ries who are better able to aord room and board
costs. To make this option eective, however, states
must allow eligible persons to retain enough of
their income to cover “maintenance needs,” includ-
ing the room and board charges in residential care
settings. Setting a higher maintenance allowance
may allow more beneciaries to be served in resi-
dential care settings; however, it will increase Med-
icaid’s service payment since it reduces the “excess
income” that is applied to the cost of services.
Under Medicaid’s post-eligibility treatment of
income rules for HCBS waivers, states are allowed to
use “reasonable standards” to establish the mainte-
nance allowance, and may vary the allowance based
on the beneciary’s circumstances. For example,
states can permit Medicaid beneciaries to keep
sucient income to pay for the needs of a depen-
dent, health care costs not covered by Medicaid,
and other necessary expenses.
States typically set a single maintenance needs
allowance for all HCBS waiver participants. Many
states set their maintenance needs allowance at 300
percent of the SSI Federal benet. Since 300 percent
of the SSI Federal benet is the highest amount of
income a person can have and still be subject to
share of cost requirements, setting the maintenance
needs allowance at that level allows waiver partici-
pants to keep all of their income to pay for living ex-
penses. It also eliminates the administrative burden
for states to calculate cost-sharing requirements.

140 Understanding Medicaid Home and Community Services: A Primer
If a state does not want to set a single maintenance
needs allowance, Medicaid rules allow states to set
dierent maintenance allowances for each individ-
ual, or for groups of individuals, if they believe that
dierent amounts are justied by the needs of the
individuals or groups.
Beneciaries living in residential care settings may
have dierent income needs depending on the type
of facility: private market-rate facility or subsidized
housing facility. The rent component of the monthly
fee charged by facilities built with low-income hous-
ing tax credits will be lower than the rent charged
by privately nanced facilities. Through tax credits,
rents can be reduced to around $400 per month. A
lower maintenance amount for individuals with rent
subsidies means more income is available to share
the cost of services.
Setting the maintenance allowance based on the
area’s average monthly charge for room and board
may be overly generous when applied to residents
in subsidized units. On the other hand, setting the
maintenance allowance based on the amount paid
by residents in subsidized units may be too low for
private market facilities and create access barriers.
If a state wants to improve access to both private
and subsidized residential care facilities, it can set a
separate maintenance allowance for each setting.
Income Supplementation by
Family Members or Trusts
Family members may be able and willing to help
with room and board costs when the beneciary is
unable to pay them. While this discussion focuses
on payments by family members, payments may
also be made by a special needs trust on behalf of
its named beneciary. Many families set up such
trusts for adult children with disabilities to ensure
that they will be adequately taken care of through-
out their lives.
Since Medicaid does not pay for room and board
in residential care settings, Federal rules regarding
supplementation in nursing homes do not apply
(i.e., families of nursing home residents may not
supplement Medicaid payments, which cover room
and board and services).
As presented in Table 5-2, 24 states and the District
of Columbia reported that they allow family supple-
mentation for individuals in residential care set-
tings, 14 states do not allow supplementation, and
2 states have no policy. The remaining states either
do not cover services in residential care
settings or did not report whether they have a
supplementation policy.
41
States are not allowed to
require supplementation.
In states that allow supplementation, family mem-
bers need to understand that the amount of the
supplement is considered in determining nancial
eligibility for SSI. Federal SSI regulations contain
provisions for treating unearned income during
the eligibility determination process, and, because
Medicaid income and resource rules for the “Aged,
Blind, and Disabled” follow SSI rules, the SSI rules
for treating unearned income apply to Medicaid
eligibility determinations as well, even if an “elderly,
blind, or disabled” person is not receiving SSI.
42
The
application of SSI rules is not required for individu-
als eligible for Medicaid through another categori-
cal group, such as pregnant women.
Under SSI rules, the entire amount of a family con-
tribution paid directly to an individual is counted
as unearned income. As a result, supplementation
can lead to a reduced SSI payment or the loss of
SSI altogether, and with it, potentially Medicaid as
well. Even if an individual is not receiving SSI, this
unearned income could cause him or her to lose
Medicaid if it raises countable income above the
Medicaid income limit.
If, however, the family contribution is paid directly
to a residential care facility on the beneciary’s be-
half, it is treated somewhat dierently (i.e., as an “in-
kind” payment). Under SSI (and therefore Medicaid)
rules, in-kind support and maintenance—no matter
how much—is valued at only one-third of the
monthly SSI benet, or approximately $225 in 2010.
This amount is also considered to be unearned
income, just as a direct payment from the family
to the individual would be, with similar potential
consequences. The dierence is that an in-kind pay-
ment cannot be valued at more than one-third
141
Chapter 5: Providing Medicaid Services in Community Residential Settings
Table 5-2. Family Supplementation Policy
Allow Supplementation No Policy Prohibit Supplementation
Alaska
Arizona
Colorado
Connecticut
Delaware
District of Columbia
Florida
Georgia
Kansas
Maine
Minnesota
Missouri
Nevada
New Hampshire
New Jersey
New Mexico
North Carolina
North Dakota
Oklahoma
Rhode Island
Tennessee
Utah
Washington
Wisconsin
Wyoming
Indiana
Massachusetts
California
Hawaii
Illinois
Maryland
Michigan
Montana
Nebraska
New York
Ohio
Oregon
South Carolina
South Dakota
Texas
Vermont
of the SSI benet, whereas the entire amount of a
direct payment to the individual is countable.
Another point worth noting is that if the family can
document that the actual amount of an in-kind
payment is less than one-third of the SSI monthly
payment, the actual amount of the payment will
be used instead of the higher one-third amount. Fi-
nally, some states have elected to not count in-kind
support and maintenance at all when determining
eligibility for Medicaid. The Medicaid state agency
should be able to provide information on whether a
state has elected to not count such support.
Because the Federal rule states that the maximum
reduction to an SSI payment is only one-third of the
benet, there is no limit on the amount of money
that can be paid to a facility on behalf of an SSI
beneciary. If a family chooses, they could pay for a
private room and board in a more expensive facility
without jeopardizing an individual’s eligibility for
SSI. However, the payment could result in the loss of
Medicaid eligibility.
To prevent beneciaries from losing Medicaid
eligibility, states could amend their State Plan, with
approval from CMS, to exempt in-kind income that
supports a person’s accommodations or services
not covered by the Medicaid payment in residential
care settings. Section 1902(r)(2) of the Social Secu-
rity Act allows states to use less restrictive income
and resource methodologies than are used by SSI
when determining eligibility for most Medicaid
eligibility groups. States can elect to disregard dif-
ferent kinds or greater amounts of income and/or
resources than SSI, giving states more exibility to
design and operate their Medicaid programs.
However, although a state may limit its less restric-
tive methodologies to eligibility groups it selects,

142 Understanding Medicaid Home and Community Services: A Primer
the group(s) must still be one of those specically
listed in §1902(r)(2); for example, buy-in groups for
working persons with disabilities, most poverty-
related groups, and the medically needy. States are
not permitted to carve out a subgroup of their own
denition (e.g., one based on place of residence).
Eect of Medically Needy Rules on the Ability
to Pay for Room and Board
States have the option of covering medically needy
beneciaries under their Medicaid programs.
The medically needy are persons who, except for
income, would qualify under one of the other
Medicaid eligibility groups covered under the State
Plan (such as people receiving SSI or the optional
aged and disabled poverty level group). Medicaid
payments can begin for medically needy persons
once they have “spent down”—that is, incurred
expenses for medical care in an amount at least
equal to the amount by which their income exceeds
the medically needy income level. As discussed in
the previous section, any family supplementation is
considered part of the excess income that must be
spent down. If it is paid to a residential care facility,
the one-third rule applies and it is still treated as
unearned income.
The medically needy eligibility option can allow
people who have income greater than 300 percent
of SSI to become eligible for Medicaid services. But
Federal law imposes two signicant constraints on
the use of this option:
The state must cover medically needy children and
pregnant women before it can elect to cover any
other medically needy group. Additionally, the state
may not place limits on who is eligible for Medicaid
by using such characteristics as diagnosis or place
of residence. Thus, it cannot use medically needy
policies to extend Medicaid services only to HCBS
waiver beneciaries in residential care settings.
The maximum income-eligibility limit that a state
medically needy program may use is based upon
its welfare program for families—levels that are
typically lower than SSI. The income level must be
the same for all medically needy groups in the state
(i.e., states are not permitted to establish higher
income-eligibility levels for selected subsets of the
medically needy, such as beneciaries in residential
care settings).
These rules have several implications that states
need to consider when trying to make the medi-
cally needy eligibility option work for higher income
individuals in residential care settings. First, these
individuals may nd it more dicult to incur suf-
cient medical expenses to meet the spend-down
requirements while living in the residential care set-
ting than they would in a nursing home. The higher
their “excess” income, the higher the amount of their
spend-down, which means that only beneciaries
with extremely high medical expenses may become
eligible for Medicaid.
Second, community providers are less willing to
deliver services during the spend-down period,
since payment cannot be guaranteed and collection
may be dicult. Third, spend-down rules combined
with low medically needy income-eligibility levels
mean that individuals may not have enough total
income to pay both the bills they incur under the
spend-down provision and room and board. Permit-
ting spend-down to a higher amount—such as 300
percent of SSI instead of a state’s medically needy
standard for HCBS waiver eligibility—requires a
change in the Medicaid statute.
In summary, room and board costs may present an
access barrier to residential care settings for Medic-
aid beneciaries unless states take specic steps to
make these costs aordable. Several observers have
suggested that the Medicaid program be allowed to
pay for room and board in residential care settings
as it does in nursing homes. To do so, Congress
would have to amend the Medicaid statute. It is
possible that states would not welcome this change
because currently the SSI benet, which pays for
room and board, is 100 percent Federal funding. If
Medicaid were to pay for room and board in resi-
dential care settings, states would be responsible
for part of the cost under Federal Medical Assistance
Percentage provisions. (See Chapter 2 for a detailed
discussion of Medicaid’s nancial eligibility rules.)
143
Chapter 5: Providing Medicaid Services in Community Residential Settings
Service Payment Rates:
Adequacy Concerns
Unless service rates are considered reasonable by
residential care settings, they will not be willing to
contract with Medicaid, particularly in states where
private pay rates are very high. It is important for
states to recognize that payment levels will likely
need to vary based on residents’ current needs
(called tiered rates). Doing so will enable people
whose condition deteriorates to stay in the setting
rather than having to move to a nursing home. A
number of states use tiered rates (including Arizona,
Delaware, Ohio, Oregon, Vermont, and Washington).
Rates set by case mix (as used in Minnesota, Maine,
Wisconsin, and New York) also create incentives to
accept people with high needs and retain people
whose needs increase. Flat rates, in contrast, tend to
force facilities to discharge residents whose needs
exceed what can be covered under the rate.
Many states use tiers or levels of payment in group
homes for individuals with developmental disabili-
ties to account for individual needs within a single
setting, allowing increased payments for individuals
who have intensive medical or behavioral support
needs requiring a higher stang ratio or special-
ized expertise. For example, Ohio uses payment
rates that account for the size of the setting, the
stang ratio, and residents’ specialized needs. This
allows for individualized services that are tailored
to the support needs of persons in group settings.
Alabama and Utah use an assessment process that
costs out the hours of support an individual needs,
while Missouri establishes rates by “category” of
facility, with higher payment rates going to settings
serving individuals with more intensive support
needs. As payment rates are set, consideration
should be given to what aspects of the supports are
included in the rate versus other supports that are
billed outside the rate.
Whatever the specic process, states will want to
allow for individualization of rates to ensure that
individuals receive the level of support appropriate
to their needs. This type of individualized rate can
also be applied to foster homes as well. For exam-
ple, some states operate “medical” foster homes that
support children with intensive medical needs. The
costs for operating these specialized homes—and
their highly specialized personnel—are reected in
the payment rates.
Payments to licensed foster care settings may
be tax exempt. If so, individualizing rates allows
states to adjust the payment rate to account for
the increased revenue to the provider because
they may not have to pay Federal income taxes.
�
As
with larger residential care settings, the foster care
payment rates can be individualized and tailored
to meet the needs of the individuals and/or target
group served.
Bundling Payments
Bundled rates are permitted for services that are by
design multi-component or, as a practical matter,
very dicult to break down into separate billing
components; for example, rates for a single worker
who supervises several residents and engages in
one-on-one interactions with them for varying
lengths of time. States are expected to have eec-
tive means to verify that bundled services are in
fact providing the claimed components. Monthly
rates are not as useful for this purpose as are daily
or, in some cases, hourly bundled rates, which can
account for resident absences from a facility for
varying amounts of time for other services, such as
osite vocational programs.

144 Understanding Medicaid Home and Community Services: A Primer
Resources
Since the Primer was rst published in 2000, numerous reports and other resources have become avail-
able on the Internet. This section includes key resources relevant to the use of Medicaid to pay for services
in residential care settings. Most of the publications cite additional resources, and the websites also have
links to other sources of information.
Publications
Mollica, R. (2009). State Medicaid Reimbursement Policies and Practices in Assisted Living. Washington, DC:
National Center for Assisted Living, American Health Care Association.
This report presents and updates information on state coverage of Medicaid services in assisted living/residen-
tial care settings and includes the source of coverage, the number of participating facilities, number of people
served, payment rates, and other data.
Available at http://www.ahcancal.org/ncal/resources/Documents/MedicaidAssistedLivingReport.pdf
Mollica, R.L., Simms-Kastelein, K., Cheek, M., Baldwin, C., Farnham, J., Reinhard, S., and
Accius, J. (2009). Building Adult Foster Care: What States Can Do. Washington, DC: AARP, Public Policy Insti-
tute.
This report examines the role of adult foster care within the long-term care system and oers guidance to
policy makers interested in developing or expanding this type of residential care.
Available at http://www.aarp.org/health/doctors-hospitals/info-09-2009/2009_13_building.html
CMS. (2008). Application for a §1915(c) Home and Community-Based Waiver [Version 3.5]: Instructions, Tech-
nical Guide and Review Criteria. Baltimore, MD: U.S. Department of Health and Human Services.
This publication contains extensive information concerning Federal policies that apply to the operation of an
HCBS waiver, including a section on paying for services in residential facilities. (Appendix C-2-c: Facilities Sub-
ject to §1616(e) of the Social Security Act.)
Available at https://www.hcbswaivers.net/CMS/faces/portal.jspunder links and downloads, entitled §1915(c)
Waiver Application and Accompanying Materials.
145
Chapter 5: Providing Medicaid Services in Community Residential Settings
Mollica, R., Sims-Kastelein, K., and O’Keee, J. (2007). Residential Care and Assisted Living Compendium:
2007. Washington, DC: U.S. Department of Health and Human Services, Oce of the Assistant Secretary for
Planning and Evaluation, Oce of Disability, Aging and Long-Term Care Policy.
This report provides information about regulations covering residential care/assisted living facilities in all 50
states and the District of Columbia. It also discusses Medicaid policy regarding coverage of services in these
facilities.
Available at http://aspe.hhs.gov/daltcp/reports/2007/07alcom.htm
Ireys, H.T., Pires, S., and Lee, M. (2006). Public Financing of Home and Community Services for Children and
Youth with Serious Emotional Disturbances: Selected Strategies. Washington, DC: U.S. Department of Health
and Human Services, Oce of the Assistant Secretary for Planning and Evaluation, Oce of Disability, Ag-
ing and Long-Term Care Policy.
This report describes important system-of-care principles that have shaped services for youth with serious
emotional disturbances, the role of the various agencies that serve these children, and the nancing mecha-
nisms many states use to fund services for this population. It covers the strengths and weaknesses of major
nancing mechanisms, including HCBS waivers, the Medicaid rehabilitation option, and provisions in the
Tax Equity and Fiscal Responsibility Act, also known as the Katie Beckett provision. The report also presents
information that can inform legislative eorts to strengthen the nancing of intensive home and community
services for youth with serious emotional disturbances and their families.
Available at http://aspe.hhs.gov/daltcp/reports/2006/youthSED.htm
Stanclie, R.J., and Lakin, C. (2004). Costs and Outcomes of Community Services for Persons with Intel-
lectual and Developmental Disabilities. Policy Research Brief 14(1). Minneapolis: University of Minnesota,
Research and Training Center on Community Living.
This Policy Research Brief reviews available research on the costs and outcomes of community service provi-
sion for people with intellectual disabilities and developmental disabilities, with a particular emphasis on
residential services. It focuses on a number of key issues related not only to public expenditures, but also to
funding systems, related policies and regulations, and their impact on service systems, on specic service
types, and on service users.
Available at http://ici.umn.edu/products/prb/151/151.pdf
146 Understanding Medicaid Home and Community Services: A Primer
Websites
Assisted Living Federation of America (ALFA)
The Assisted Living Federation of America is the largest national association exclusively dedicated to profes-
sionally operated assisted living communities for seniors. ALFA’s member-driven programs promote business
and operational excellence through national conferences, research, publications, and executive networks. In
addition, ALFA works to inuence public policy by advocating for informed choice, quality care, and accessibil-
ity for all Americans. The website includes links to publications and information about Federal and state policy.
Web address: http://www.alfa.org/alfa/Default.asp
Center for Excellence in Assisted Living
The Center for Excellence in Assisted Living is a non-prot collaborative of 11 national organizations that
builds upon the work of the Assisted Living Workgroup, which was formed to work with the U.S. Special Com-
mittee on Aging on a range of assisted living issues. The Center’s purpose is to promote high-quality assisted
living and to serve as a national clearinghouse for information about assisted living, including research nd-
ings, exemplary practices, training and education materials, and consumer materials.
Web address: http://www.theceal.org
The Clearinghouse for Home and Community Based Services
This site promotes the development and expansion of home and community-based services by gathering
resources and tools for research, policymaking, and program development into this one-stop website. The site
has over 2,000 resources that users can browse using the site’s search engine. For example, using the search
words “Medicaid” and “assisted living” yields 17 results, including several of the publications listed above.
Web address: http://www.hcbs.org/

147
Chapter 5: Providing Medicaid Services in Community Residential Settings
Endnotes: Citations, Additional Information,
and Web Addresses
1
Janet O’Keee and Robin Cooper co-authored this chapter. Some sections of this chapter draw liber-
ally from other published sources, which are referenced in the endnotes.
2
Medicaid-covered “institutional” services refer to specic services and settings as authorized in the
Social Security Act. While the term “institutional” is also commonly used to describe specic character-
istics of a facility—such as structuring its operation to accommodate the facility’s needs rather than
the residents’ choices—in Federal Medicaid statute and regulations the term institutional generally
has the following meanings:
(1)The service is institutional, that is, a provider accepts responsibility for residents’ overall care, and
furnishes food and shelter in addition to services; (2)the setting is institutional—subject to state licen-
sure requirements and survey and certication process; (3)payment is made through separate provi-
sions for institutional services; and (4)eligibility rules may be specic to institutional services.
Taken together, these requirements mean, among other things, that an institutional service such as
Medicaid nursing facilities can only be provided in a Medicaid-certied nursing facility, and only reim-
bursed under the Medi caid nursing facility benet. It is important to note that a facility does not have
to have many beds to be considered an institution, despite the popular image of institutions as being
large. (See endnote 5 regarding the minimum size of an ICF/ID.)
3
Come-in sta generally work 8-hour shifts (day, evening, night) but can also work 12-hour day or night
shifts.
4
ICFs/ID are considered institutions under Federal regulations. Although some ICFs/ID are large state-
operated facilities, the majority are now smaller. CMS regulations provide for a “community size” ICF/
ID option. Facilities that have 15 or fewer beds are considered “community” ICFs/ID, and facilities with
16 or more beds are considered to be “large.” A number of states operate community ICFs/ID, many of
which have few beds.
For example, California, Texas, Illinois, Indiana, and Louisiana, among other states, all have ICFs/ID that
serve six or fewer individuals. Thus, a state could potentially provide services under the HCBS waiver
in group homes that serve the same number of residents (or more) than an ICF/ID, so that the two
settings are the same in size. The dierence is that the ICF/ID setting provides the ICF/ID institutional
service, must comply with numerous Federal regulations, and receives the comprehensive institution-
al reimbursement, which includes payment for room and board.
5
CMS. (2008). Application for a §1915(c) Home and Community-Based Waiver [Version 3.5], Instructions,
Technical Guide and Review Criteria, Appendix C-2-c-ii, p. 117. See the Resources section of this chap-
ter for a web link to the application, instructions, and appendices.
6
Ibid.
7
Found at http://www.minnesotahelp.org/Public/taxonomy_glossary.aspx?code=BH-840.600-28.
8
Section 1616(e) of the Social Security Act requires that the state must “establish, maintain, and insure

148 Understanding Medicaid Home and Community Services: A Primer
the enforcement of standards for any category of institutions, foster homes, or group living arrange-
ments in which a signicant number of SSI recipients resides or is likely to reside. The standards must
be (a)appropriate to the needs of residents and the character of the facilities involved; and (b)govern
such matters as admission policies, safety, sanitation, and protection of civil rights.”
Section 1616(e) also requires states to maintain records of information concerning standards, proce-
dures available to ensure enforcement of the standards, and a list of waivers of standards and viola-
tions of standards by specic facilities. These records must be made available annually to the public.
States must certify annually to the Commissioner of Social Security that they are in compliance. Oce
of the Inspector General (March 31, 1997). Review of the Social Security Administration Procedures to
Ensure State Compliance with §1616(e) of the Social Security Act – A-01-96-62001. Available at http://
www.ssa.gov/oig/ADOBEPDF/audit_htms/96-62001.htm.
9
Mollica, R., Sims-Kastelein, K., and O’Keee, J. (2007). Residential Care and Assisted Living Compen-
dium: 2007. Washington, DC: U.S. Department of Health and Human Services, Oce of the Assistant
Secretary for Planning and Evaluation, Oce of Disability, Aging and Long-Term Care Policy. Available
at http://aspe.hhs.gov/daltcp/reports/2007/07alcom.htm.
10
CMS. (2008). Application for a §1915(c) Home and Community-Based Waiver [Version 3.5], Instructions,
Technical Guide and Review Criteria, pp. 168-169, and 265-266. See the Resources section of this chap-
ter for a web link to the application, instructions, and appendices.
11
Mollica, R., Booth, M., Gray, C., and Sims-Kastelein, K. (2008). Adult Foster Care: A Resource for Older
Adults. New Brunswick, NJ: Rutgers Center for Health Policy, p. 7. Available at http://www.hcbs.org/
moreInfo.php/doc/2273.
12
Alba, K., Prouty, R.W., and Lakin, K.C. (2007). Chapter 4: Number of Residential Settings and Residents
by Type of Living Arrangement on June 30, 2007. In Prouty, R.W., Alba, K., and Lakin, K.C. (Eds.). Resi-
dential Services for Persons with Developmental Disabilities: Status and Trends through 2007. Min-
neapolis: University of Minnesota, Research and Training Center on Community Living, Institute on
Community Integration, p. 45. Available at http://www.hcbs.org/moreInfo.php/doc/2312.
13
Mollica, R.L., Simms-Kastelein, K., Cheek, M., Baldwin, C., Farnham, J., Reinhard, S., and Accius, J. (2009).
Building Adult Foster Care: What States Can Do. Washington, DC: AARP, Public Policy Institute, p. 9.
Avail able at http://www.aarp.org/health/doctors-hospitals/info-09-2009/2009_13_building.html.
14
Supported living in an individual’s own home and any other type of residential supports a state wants
to cover are also subsumed under residential habilitation.
15
CMS. (2008). Application for a §1915(c) Home and Community-Based Waiver [Version 3.5], Instructions,
Technical Guide and Review Criteria, pp. 151-152. See the Resources section of this chapter for a web
link to the application, instructions, and appendices.
16
45 CFR 1355.20.
17
CMS. (2008). Application for a §1915(c) Home and Community-Based Waiver [Version 3.5], Instructions,
Technical Guide and Review Criteria, p. 131. See the Resources section of this chapter for a web link to
the application, instructions, and appendices.
18
Utah’s Community Supports Waiver for Individuals with Intellectual Disabilities and Related Condi-
tions, Waiver # 0158.90.r#.02.

149
Chapter 5: Providing Medicaid Services in Community Residential Settings
19
States do not have to include citations of state rules, which can change over time. The application
must also include the state’s quality assurance plans.
20
Hawes, C. (2001). Introduction. In Zimmerman, S., Sloan, P.D., and Eckert, K. (Eds.). Assisted Living:
Needs, Practices, and Policies in Residential Care for the Elderly. Baltimore, MD: The Johns Hopkins
University Press.
21
The supply of older residential care facilities that serve individuals eligible for SSI and Medicaid is
much larger than the supply of private pay assisted living facilities. Robert Newcomer, University of
California at San Francisco. Personal communication, November 25, 2009.
22
Mollica, R., Sims-Kastelein, K., and O’Keee, J. (2007), op. cit.
23
Mollica, R. (2009). State Medicaid Reimbursement Policies and Practices in Assisted Living. Washing-
ton, DC: National Center for Assisted Living; American Health Care Association. Available at http://
www.ahcancal.org/ncal/resources/Documents/MedicaidAssistedLivingReport.pdf. Hawes, C., Rose, M.,
and Phillips, C.D. (1999). A National Study of Assisted Living for the Frail Elderly: Results of a National
Survey of Facilities. U.S. Department of Health and Human Services, Oce of the Assistant Secretary
for Planning and Evaluation, Oce of Disability, Aging and Long-Term Care Policy. Available at http://
aspe.hhs.gov/daltcp/reports/facres.pdf.
24
The Guidance also notes that states may modify or supplement the core denition to reect the scope
of assisted living services furnished under the waiver.
25
CMS. (2008). Application for a §1915(c) Home and Community-Based Waiver [Version 3.5], Instructions,
Technical Guide and Review Criteria, pp. 117, 170. See the Resources section of this chapter for a web
link to the application, instructions, and appendices.
26
Ibid. Appendix C, Attachment: Core Service Denition, pp. 151-153.
27
This section draws liberally from Mollica, R., Sims-Kastelein, K., and O’Keee, J. (2007), op. cit.
28
An HCBS waiver may cover services provided in participants’ homes or in residential care settings.
Some states have implemented specialized assisted living waivers, which provide services only in resi-
dential care settings.
29
Mollica, R. (2009), op. cit. Individuals with developmental disabilities who meet a state’s nursing home
level-of-care criteria may also be served in Aged or Aged/Disabled HCBS waiver programs. But only
persons with developmental disabilities can be served in ID/DD waiver programs, because the level-
of-care criteria for ICFs/ID require a specic diagnosis of developmental disabilities to be eligible.
30
Information in the Boxes is mainly from Mollica, R. (2009), op. cit., and Mollica, R., Sims-Kastelein, K.,
and O’Keee, J. (2007), op. cit.
31
Licensing requirements adopted in 1995 and 1996 established the umbrella term of “assisted living
residences” for two types of residential care facilities: (1)licensed adult care homes and (2) multi-unit
assisted housing with services (which are not licensed, but must be registered with the State).
32
Residents may be asked to leave under the following conditions: (a)their needs exceed the level of
ADL services provided by the facility; (b)the resident’s behavior interferes with the rights and well-be-
ing of others or poses a danger to self and others; (c)the resident has a medical or nursing condition
that is complex, unstable or unpredictable and exceeds the level of health services the facility pro-
vides; or (d)the facility is unable to accomplish resident evacuation in accordance with OAR 411-054-

150 Understanding Medicaid Home and Community Services: A Primer
0090 (Fire and Life Safety).
33
As noted, above, states do not have to include citations of state rules, which can change over time. The
application must also include the state’s quality assurance plans.
34
Oregon and Washington also allow other types of residential care settings that contract with Medicaid
to have shared rooms.
35
The information in this section is taken verbatim from Mollica, R., Sims-Kastelein, K., and O’Keee, J.
(2007), op. cit.
36
Medicaid will pay for food costs in specic situations, such as meals served as part of an adult day
health program.
37
CMS. (2008). Application for a §1915(c) Home and Community-Based Waiver [Version 3.5], Instruc-
tions, Technical Guide and Review Criteria, Appendix I-5: Exclusion of Medicaid Payment for Room and
Board, pp. 265-266. See the Resources section of this chapter for a web link to the application, instruc-
tions, and appendices.
38
Many states have a state supplement for residential care settings that may be too low to cover more
intense services needs and higher capital costs in some residential care settings.
39
Mollica, R., (2009), op. cit.
40
The net cost to the state will depend on Medicaid payment rates for both nursing homes and services
in residential care facilities.
41
Mollica, R. (2009), op. cit.
42
Family contributions that do not aect SSI eligibility—and therefore do not aect Medicaid eligibil-
ity—might have an aect in 209(b) states because Medicaid eligibility in these states is not linked
to SSI eligibility. (When SSI replaced state-only programs of aid for elderly persons and persons with
disabilities, the change was expected to lead to large increases in the numbers of SSI beneciaries. The
209(b) option was enacted along with SSI in 1972 to enable states to limit large increases in Medicaid
enrollment and costs.
43
See IRS Code Section 131b1 that denes a qualied foster care payment as “a payment made pursu-
ant to a foster care program of a state or a political subdivision of the state: that is paid by a political
subdivision of a state, or a qualied foster care placement agency; and that is paid to the foster care
provider for caring for a qualied foster care individual in the foster care provider’s home, or a di-
culty of care payment.”

Chapter 6: Transitioning People from Institutions to the Community
151
Guide to Chapter 6
Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .153
Lessons from the Transitioning Experience with ICFs/ID . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .154
Nursing Home Transition Grants Program . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .156
General Factors to Consider for Transition Initiatives . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .157
Identifying and Addressing Administrative and Legal Barriers . . . . . . . . . . . . . . . . . . .157
Ensuring the Availability of a Comprehensive Range of
Home and Community Services . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .158
Developing Methods to Circumvent HCBS Waiver Waiting Lists . . . . . . . . . . . . . . . . .158
Identifying and Educating Residents
with the Desire and Potential for Transition . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .159
Involving and Collaborating with Key Stakeholders . . . . . . . . . . . . . . . . . . . . . . . . . . . . .161
Developing and Implementing Case Management/Service
Coordination Systems That Support Transition . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .162
Identifying and Addressing Housing Needs and Rental Assistance . . . . . . . . . . . . . .163
Providing Flexible Funding Mechanisms . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .165
Preventing Unnecessary Admissions and Avoidable Long Stays . . . . . . . . . . . . . . . . . . . . . . . . .166
Establishing a Quality Assurance System
That Eectively Balances Risk and Autonomy . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .166
Resources. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .168
Endnotes: Citations, Additional Information, and Web Addresses . . . . . . . . . . . . . . . . . . . . . . .171
153
Chapter 6: Transitioning People from Institutions to the Community
Chapter 6
Transitioning People from Institutions to the Community
The realization that many people with long-term care service and support needs can thrive in integrated commu-
nity settings and the requirements of the Supreme Court’s Olmstead decision have increased states’ commitment to
transition residents of intermediate care facilities for persons with intellectual disabilities (ICFs/ID), nursing facilities,
and other long-term care institutions to the community. This chapter begins with a brief overview of how states
have used Medicaid home and community-based services (HCBS) waiver programs to enable ICFs/ID residents to
transition to the community. It then discusses important factors states need to consider when planning transition
programs for persons in nursing facilities and options for using Medicaid to help cover certain transition costs.1
Introduction
After Medicaid’s enactment, the following decades saw an increase in the number of states developing alter-
natives to institutional care for persons with disabilities, in order to provide services and supports in the most
integrated setting appropriate to their needs. The Supreme Court decision—Olmstead v. L.C., nding that un-
necessary segregation of people with disabilities in institutions constitutes a form of discrimination under the
Americans with Disabilities Act (ADA)—gave legal weight and new urgency to this policy direction.
2
The Cen-
ters for Medicare & Medicaid (CMS) guidance, issued to states in January 2000, underscores the importance of
states’ eorts to move people out of nursing homes and other long-term care institutions into community set-
tings as a part of a state’s “comprehensive eectively working plan” for providing services to qualied persons
in the most integrated settings. (See the Resources section of this chapter for a link to the complete text of this
guidance.)
Transitioning people with disabilities from institutions to the community began in a serious way with the rec-
ognition that many people with intellectual disabilities and other developmental disabilities (ID/DD, hereafter
called developmental disabilities) were inappropriately placed in large public facilities and institutions. This
recognition, starting in the 1970s, led to successful eorts by many states to sharply reduce the number of
people living in large institutions (16 or more beds) by transitioning residents to a range of smaller, commu-
nity settings. This dramatic wave of deinstitutionalization set in motion the re alignment of state ID/DD service
systems from institutionally dominated to community-centered.
The rst section of this chapter provides a brief overview of the transition process for residents of ICFs/ID, dis-
tilling the lessons learned from this experience that apply to transition initiatives more generally. The second
section focuses on current Medicaid options for supporting transitions and discusses major factors states need
to consider when setting up transition programs—focusing primarily on the transition of nursing home resi-
dents—but also applicable to transitions from ICFs/ID and other institutions.
154 Understanding Medicaid Home and Community Services: A Primer
Lessons from the Transitioning
Experience with ICFs/ID
3
Medicaid funding for home and community ser-
vices and supports for persons with developmen-
tal disabilities, particularly through HCBS waiver
programs, has played a pivotal role in enabling a
substantial majority of states to reduce (or in some
cases, end completely) long-term care service
delivery in large state institutions.
4
Between 1970
and 2008, 40 states closed or initiated plans to close
more than 140 large public institutions.
5
Alaska and
Oregon have closed all of their state and non-state
ICF/ID programs and Vermont supports a single
private facility of six residents. Additionally, many
states ceased sponsoring additional ICF/ID develop-
ment.
Terminology
In the developmental disabilities service system,
ICFs/ID that serve a small number of residents—
from 15 to as few as 4—are called community
ICFs/ID, and the term “institution” is used only
for ICFs/ID with 16 or more residents. However,
for Medicaid purposes, ICFs/ID are considered
to be institutions, irrespective of the number of
people they serve.
Not all institutions that serve persons with
developmental disabilities are ICFs/ID. Prior to
coverage of ICFs/ID under Medicaid in the early
1970s, institutions were exclusively state funded.
While states converted virtually all of these insti-
tutions to ICFs/ID to take advantage of Federal
funding, a few privately funded institutions may
still be operating, as well as former ICFs/ID that
have lost their certication and are not receiving
Federal nding.
By the end of 2009, 10 states and the District of
Columbia had closed all of their large public institu-
tions for people with developmental disabilities.
6
In the private sector as well, the number of resi-
dents of both large and small ICFs/ID nationwide
has declined steadily since 1997. The decline in ICF/
ID utilization began about the same time that the
number of people with developmental disabilities
participating in HCBS waiver programs began to
grow very rapidly. Between 1992 and 2007, the
number of individuals participating in HCBS waiver
programs for people with developmental disabili-
ties grew by 703 percent.
7
A major reason for the
increased use of HCBS waivers is the exibility they
aord states to oer services and supports that can
accommodate individuals with a wide range of dif-
ferent needs in a targeted fashion without resorting
to institutionalization.
The successful transitioning of people with develop-
mental disabilities from institutions to the com-
munity demonstrates that waiver services can be
cost-eective substitutes for institutional services
for this population.
8
States that have been espe-
cially successful in closing large public facilities and
reducing reliance on ICFs/ID have taken many other
important steps to ensure that the needs of indi-
viduals with developmental disabilities can be met
in the home and community. Many of these steps
are equally applicable to beneciaries with other
disabilities being transitioned from nursing homes
and other institutions. These steps are
• Developing community-based crisis and
quick-response capabilities. In many states,
institutions provide backup services and sup-
ports for persons who are in crisis and need
emergency services. In the 10 states that have
closed all of their public institutions (as well as
the District of Columbia), each has addressed
the need for emergency support in dierent
ways. Maine established crisis response teams,
resource coordinators, and emergency place-
ment beds in small settings in each of its three
regions as part of the initiative to close its
Pineland Center facility, which had functioned
as a “crisis-placement” facility. By providing
resources in the community to respond to cri-
ses and working out permanent solutions for
the individual, a prime rationale for operating
Pineland was eliminated. Vermont established
the Vermont Crisis Intervention Network in
1992 to provide community-based emergency
support and assistance statewide. New Mexico
and Hawaii developed similar programs using
the same organizational model. The develop-
ment of an eective crisis response capability

155
Chapter 6: Transitioning People from Institutions to the Community
was instrumental in Oregon’s closing its Fair-
view facility in February 2000 and the Eastern
Oregon Training Center in 2009.
• Expanding community services to meet the
needs of individuals with multiple disabili-
ties and challenging conditions who require
particularly intensive support and assis-
tance. People with signicant needs are often
described as “requiring” institutional services.
States that have closed their institutional
programs have demonstrated that people with
even the most intensive support requirements
can lead productive and successful lives in
home and community settings when aorded
person-centered services and supports tai-
lored to their strengths and needs.
9
Many
states have found that the costs of community
services for people being transitioned from
institutional services can be higher on aver-
age than the costs of waiver services furnished
to persons who have not been institutional-
ized. This cost dierential may result because
as institutional populations have declined,
the proportion of institutionalized residents
with signicant and multiple disabilities has
increased, and these individuals require more
intensive services wherever they are served—
in an institution or the community. To ensure
sucient capacity to support these individu-
als, many states must enhance the infrastruc-
ture of community agencies.
10
• Providing higher than average funding al-
locations for individuals transitioning to the
community. States have taken steps to provide
needed services and supports in commu-
nity settings by permitting the development
of HCBS waiver service plans that allow an
individual’s costs to rise above the average for
institutions in that state. This allows states to
decide on the plausibility of transitioning for a
particular individual, without forcing individu-
als de facto to seek institutional care simply
because of an individual expenditure limit or
cap.
11
• Developing waivers targeting specic popu-
lations and groups. Although most states
accommodate transitioning individuals from
institutional settings through their existing
HCBS waiver programs, a limited number
operate distinct HCBS waiver programs for
people transitioning from institutional set-
tings. Georgia created a special HCBS waiver
program for individuals who transitioned to
the community during the State’s closure of
its 320-bed, Atlanta-based Brook Run facil-
ity in 1997. Closure of this facility resulted in
cost savings that enabled Georgia to provide
waiver services to 180 individuals in addition
to the persons transitioned from Brook Run.
The Washington State Division of Develop-
mental Disabilities developed and implement-
ed ve separate waiver programs designed to
support individuals at diering lev els of need.
Four types of waivers—Basic, Basic Plus, Core,
and Community Protection—furnish a variety
of supports at increasing intensity. A fth pro-
vides intensive in-home behavioral support to
children with signicant needs.
• Developing specialized “supports” waivers.
An increasing number of states to date have
developed and implemented distinctive HCBS
waiver programs—called supports waivers—
which oer a limited menu of specic servi ces
that operate in tandem with previously exist-
ing comprehensive waiver programs. De-
signed to limit Medicaid costs by preventing
out-of-home placement in 24-hour residential
programs or ICFs/ID, these waivers oer a
variety of exible in-home supports. Supports
waivers impose specic expenditure limits on
the amount of services provided and per-
person costs are signicantly less than those
found in comprehensive waivers. Supports
waivers typically emphasize participant direc-
tion and are intended to promote the use of
non-traditional, “natural supports” provided by
family, friends, and neighbors.
12
(See Chapter
4 for additional information about supports
waivers.)
• Expanding supports oered to individuals
and families. Family support services are cru-
cial for preventing unnecessary out-of-home
placements and are used by many states to
reduce reliance on institutional services. In
156 Understanding Medicaid Home and Community Services: A Primer
addition to supports waivers, states furnish
assistance to families through state general
fund programs and the provision of cash
subsidies or stipends. As a result of these and
other eorts, increasing numbers of individu-
als with developmental disabilities are able to
avoid institutional placement by receiving the
assistance they need in the home of a family
member. In 2007, the majority (55.8 percent) of
persons with developmental disabilities receiv-
ing publicly funded services lived in the home
of a family member.
13
Michigan, for example,
reduced the number of individuals served in
large public facilities from over 6,000 in 1977
to fewer than 300 in 1998—in large part by
implementing and sustaining family support
programs.
• Developing strong and locally centered com-
munity service systems. In developmental
dis abilities services, creating a strong infra-
structure at the community level has proven
to have a signicant impact on the ability to
avoid institutionalization and promote quality
services. An important component of Michi-
gan’s transition activities was its strengthening
of the State’s network of local governmental
Community Mental Health Service Programs
through its Section (§)1915(b)(c) managed
care waiver program. As part of its overall plan
to close its Brandon facility, Vermont placed
major emphasis on upgrading the skills of
its community workforce and maintains a
strong program to train community workers.
In Kansas, the state development al disabilities
authority and the State’s University Aliated
Program forged a partnership to improve
the training and skills of the community
workforce—a step that was instrumental in
enabling the State to transition many institu-
tional residents to the community.
• Expanding investments in quality assurance
and quality improvement capabilities. The
Medicaid HCBS waiver application requires
each state to submit a comprehensive qual-
ity management strategy outlining the ap-
proaches the state intends to use to assess,
improve, and safeguard the health and welfare
of waiver program participants.
14
Several states
are responding by improving current practice
through the utilization of standardized out-
come measurement tools such as the National
Core Indicators (NCI), which permit state-to-
state comparisons, or other instruments such
as the Participant Experience Survey. Penn-
sylvania launched a comprehensive quality
measurement system for community-based
services, which relies on information obtained
from individuals receiving support and their
families. The data are collected by individuals
who have no connection to entities deliver-
ing services. The Independent Monitoring for
Quality project combines both state-specic
and the NCI national outcome measurement
tools. (See the appendix for an overview of
CMS requirements for quality management
and improvement systems.)
Nursing Home Transition
Grants Program
During the 1990s, the system serving individuals
with developmental disabilities gained considerable
experience transitioning individuals from institu-
tions to the community. In contrast, most states
had little experience transitioning nursing home
residents to the community. To encourage states to
develop and implement nursing home transition
programs, in 1998 and 1999 the U.S. Department of
Health and Human Services (HHS) provided grants
to eight states through the Nursing Home Transition
Program.
By 1999, the Olmstead decision had increased state
interest in nursing home transition, and in Federal
scal year (FFY) 2001 and FFY 2002, under its Sys-
tems Change for Community Living Grants pro-
gram, CMS provided 33 Nursing Facility Transition
(NFT) grants to help states develop a sustainable
transition infrastructure, and to promote partner-
ships between state agencies and Independent
Living Centers (ILCs) to facilitate transitions.
15
In FY
2004, CMS awarded nine Systems Change Money
Follows the Person (MFP) grants to states to contin-
ue working on NFT initiatives with a specic focus
on developing and implementing MFP initiatives.
16
157
Chapter 6: Transitioning People from Institutions to the Community
Many of the lessons learned through this grants
program, and Grantees’ recommendations for ad-
dressing continuing transition barriers, have been
incorporated into the discussion that follows.
General Factors to Consider for
Transition Initiatives
Successful transitions depend fundamentally on the
ability to provide services and supports in the com-
munity that meet the needs of the person transi-
tioning. Persons leaving ICFs/ID have varying types
and levels of need. Residents of nursing facilities are
an even more heterogeneous group. Nursing facility
residents can include a 75-year-old with cogni-
tive impairment and multiple medical problems,
a 45-year-old with quadriplegia, and a 25-year-old
with a traumatic brain injury (TBI). While those tran-
sitioning will have some needs in common, they will
also require services and supports tailored to their
specic situations.
Whether a person currently resides in a nursing
facility or in an institution serving primarily those
with a developmental disability or mental illness,
the steps in planning or arranging for home and
community services are the same. In either case,
solid transitional planning is essential.
17
Because
each person has unique needs, the complexity and
cost of each individual’s transition process will vary.
For this reason, it is crucial that states design their
transition programs to operate with maximum
exibility. In addition to the numerous options for
providing home and community services, Medic-
aid also provides options to facilitate and support
transitions.
The remainder of this chapter will discuss the key
factors essential to implementing successful transi-
tion programs, along with related Medicaid policies
and service options. The key factors are
• Identifying and addressing administrative and
legal barriers to transition.
• Ensuring the availability of a comprehensive
range of home and community services.
• Developing methods to circumvent HCBS
waiver waiting lists.
• Identifying and educating residents with the
desire and the potential for transition.
• Involving and collaborating with key stake-
holders.
• Developing and implementing care manage-
ment/service coordination systems that sup-
port transition.
• Identifying and addressing housing needs and
rental assistance.
• Providing exible funding mechanisms.
States generally undertake many of these activi-
ties simultaneously. The chapter ends with a brief
discussion of how states can prevent unnecessary
admissions to institutions and avoidable long stays.
Identifying and Addressing
Administrative and Legal Barriers
States need to analyze their Medicaid regulations
and administrative policies to identify any institu-
tional bias that might make it dicult or impos-
sible for some people living in nursing homes to
be served in the community. For example, if a state
does not use the 300 percent of SSI income rule for
its HCBS waiver program, some institutional resi-
dents will not meet the nancial eligibility criteria
for waiver services, even though they can be appro-
priately served in the community. (See Chapter 2 for
a discussion of Medicaid’s nancial eligibility rules.)
In addition, if Medicaid’s maintenance needs allow-
ance is too low to permit individuals to pay for room
and board costs in the community, nursing home
residents may be unable, simply for nancial rea-
sons, to transition to the community—whether to
an independent living arrangement or a residential
care facility. (See Chapter 2 for a discussion about
nancial criteria and Chapter 5 for a discussion of
state policies to help Medicaid beneciaries aord
room and board costs.)
158 Understanding Medicaid Home and Community Services: A Primer
Ensuring the Availability of a
Comprehensive Range of Home
and Community Services18
Since persons transitioning from institutions have
widely varying needs, the transition process presup-
poses that a broad range of home and community
services and supports is available. Yet,
Medicaid HCBS waiver programs vary greatly in the
comprehensiveness of services they provide, and
in many states the home and community services
system does not provide the amount, duration, and
scope of services needed to enable people with
severe disabilities or extensive nursing needs to live
safely in the community.
New Service Developed to
Enable Transition
During implementation of its Systems Change
NFT grant, state sta in Rhode Island found
that lack of day services was a transition barrier
for persons with traumatic brain injury. Under
a contract with an adult day services provider,
grant sta established an adult day services pro-
gram for adults with severe cognitive disabili-
ties, many with traumatic brain injury. The new
program is now funded as a Medicaid State Plan
service under the Rehabilitation services option.
Some Systems Change NFT Grantees cited a lack
of services for specic populations as a transition
barrier; for example, when a state does not have a
TBI waiver and the services available in other waiver
programs do not meet the needs of persons with
traumatic brain injury. Other barriers Grantees cited
were (1)insucient funding for home modications
and assistive technology; (2)HCBS waiver programs
that do not provide all of the services a person
needs; (3)lack of mental health and substance
abuse services and supports; and (4) lack of agree-
ment among state agencies about who is respon-
sible for providing services for people with both
physical and mental impairments, making it dicult
to ensure adequate services for this population. The
lack of nurse delegation provisions that enable in-
dividuals with complex medical needs to be served
cost-eectively in the community can also be a bar-
rier as can the lack of experience of HCBS providers
in serving this population, which may make them
reluctant to do so.
Lack of home and community services prevents di-
version as well as transition. One NFT Grantee noted
that timely access to in-home services is essential
for diverting persons being discharged from hospi-
tals. In the absence of these services, hospital sta
will not discharge patients to their homes, sending
them instead to a nursing facility. Clearly, before
spending resources on transition activities, states
need to ensure that a comprehensive range of ser-
vices and supports are available in the community,
particularly for individuals with severe disabilities
and/or extensive nursing needs.
Developing Methods to Circumvent
HCBS Waiver Waiting Lists
19
Waiting lists for HCBS waiver services are a ma-
jor transition barrier. States have several options
available to deal with this problem. First, states can
prioritize their waiver waiting lists so that individu-
als wanting to transition are placed at the top of the
list (generally, after individuals who are at immedi-
ate risk of nursing home admission).
Second, states can increase the number of waiver
slots and designate them solely for people who are
transitioning. For example, Michigan authorized
new waiver slots for persons who are transitioning
if they have been in a nursing facility for more than
6 months. Exceptions to the 6-month rule may be
granted in a limited number of circumstances (e.g.,
if individuals are at risk of losing their housing). Ad-
ditionally, for each successful move to the commu-
nity, the State provides transition costs and waiver
services for one additional Medicaid nursing facility
resident without regard to their length of stay.
Third, if states are reluctant to increase the number
of waiver slots, they can appropriate state funds to
cover home and community services. When Geor-
gia’s Systems Change NFT grant ended, the State
appropriated $7.25 million for non-Medicaid cov-
ered transition expenses and the rst year of home
and community services for transitioning individu-
als for whom there were no waiver slots. The legis-
159
Chapter 6: Transitioning People from Institutions to the Community
lature specied a maximum of $50,000 per person
for up to 145 individuals. Only when individuals
have been supported with these funds for 1 year
does the State create a new waiver slot to continue
services.
Fourth, states can enact a global budget or an MFP
policy to allow Medicaid funds budgeted for institu-
tional services to be spent on home and community
services when institutional residents move to the
community.
Identifying and Educating Residents with the
Desire and Potential for Transition
States must rst establish the target population: all
individuals or specic groups, such as those under
age 60 who do not need a skilled level of care or
those who at admission are at risk of losing their
housing. Once the target population has been
selected, states must then develop feasible and
eective referral, screening, and assessment pro-
cedures to identify individuals who have the desire
and the potential to be transitioned successfully to
the community.
Money Follows the Person Demonstration
20
To further encourage states to implement nursing facility transition programs and MFP policies, the Decit
Reduction Act of 2005 authorized the Secretary of HHS to award up to $1.75 billion in special MFP demonstra-
tion grants to states over a 5-year period to support the transition of individuals from institutional settings to
the community.
21
All states were eligible to participate in the 5-year demonstration program and had to com-
mit to provide demonstration services for at least 2 years. As of 2009, 29 states and the District of Columbia had
MFP grants. The Patient Protection and Aordable Care Act of 2010 extended the demonstration program until
2016.
22
The MFP demonstration has four major objectives:
• Increase the use of home and community services in place of institutional services.
• Eliminate barriers or mechanisms that prevent Medicaid-eligible individuals from receiving appropriate
and necessary services and supports in the settings of their choice.
• Increase the ability of state Medicaid programs to ensure continued provision of services and supports to
eligible individuals who choose to move from an institutional to a community setting.
• Ensure that procedures are in place to ensure the quality of Medicaid home and community services, and
to provide for continuous quality improvement in the furnishing of these services.
As an incentive to states to participate, CMS will increase Federal Medicaid matching funds for home and com-
munity services for each person transitioned for a 1-year period, after which the state must ensure
that individuals transitioned will continue to receive HCBS as long as they are Medicaid eligible and need
the services.
To qualify for the enhanced Federal match, individuals must transition to community living arrangements that
they own or lease, their family home, or a community-based residential setting where no more than four unre-
lated people reside.
The MFP program is being rigorously evaluated and CMS is oering an ongoing series of reports completed as
part of the MFP national evaluation.
23

160 Understanding Medicaid Home and Community Services: A Primer
There is no single prole of a nursing facility resi-
dent who would be considered a good candidate
for transition. Individuals of all ages with many dif-
ferent diagnoses and varying disability levels have
successfully transitioned. However, some factors
are considered essential for an individual’s success-
ful transition: motivation for discharge, community
supports, and available housing. People who lost
their home during a nursing home stay and those
whose home is not accessible can nd it dicult to
transition.
Some states have used the nursing home minimum
data set (MDS) or other screening and assessment
tools to identify potential candidates.
25
The MDS is a
core set of screening and assessment elements that
forms the foundation of the comprehensive assess-
ment for nursing facility residents. By looking at
factors captured in these data sets—such as medi-
cal needs, functional status, desire to transition, and
length of stay—transition programs can screen for
potential candidates, who can then be further as-
sessed for transition.
Using MDS data in this manner, while a useful step,
is by no means sucient. Many individuals who
are good candidates for a transition program may
not show up in the initial screening, and some of
those who do may face insurmountable transition
barriers. Therefore, programs should not rely solely
on screening tools but should work with persons
and groups who know the nursing home residents.
Such knowledge can make them invaluable sources
of information to identify appropriate transition
candidates.
Minnesota enacted legislation in 2005 requiring
its Department of Human Services to develop
a methodology for sharing MDS data with
Independent Living Centers to assist them in
identifying institutional residents who want to
live in the community.
26
North Carolina added a transitions protocol to
the Medicaid Uniform Screening and Assess-
ment Tool, and obtained a Data Use Agreement
Amendment that allows the State to use MDS
data to identify those wanting to transition.
27
Nursing home ombudsmen, Independent Living
Centers, protection and advocacy organizations,
and other local groups and programs can also serve
as important partners in the identication process.
A number of states use Independent Living Centers
to both assist in the identication of individuals and
with the transition process. The expertise and capa-
bilities of such community organizations should be
tapped early on to ensure eective collaboration.
Based on the experience of Systems Change NFT
Grantees, the following methods have proved to
be most eective in identifying individuals with the
highest potential for community living: (1)targeted
outreach and education by local transition coali-
tions to nursing facility sta, including administra-
tors, social workers, discharge planners, and direc-
tors of nursing; (2)outreach activities for residents
of nursing facilities; and (3)education of and
collaboration with regional nursing facility ombuds-
men.
28
Money Follows the Person Policies: State Examples
Texas was one of the originators of the MFP concept. The State’s MFP policy enables individuals residing in
nursing facilities to move back to a community setting and to utilize their entitlement dollars to receive HCBS,
primarily through the Community-Based Alternatives waiver program. The Texas Health and Human Services
Commission implemented the program September 1, 2001, and the policy was subsequently codied into law.
The MFP policy has been highly successful in relocating individuals from nursing facilities to the community. As
of December 31, 2007, 12,461 individuals had transitioned from nursing facilities.
24
Maryland enacted the Money Follows the Individual Act, which requires admission to an HCBS waiver program
if (1)an individual is living in a nursing home at the time of the application for waiver services, (2)the nursing
home services for the individual were paid by Medicaid for at least 30 consecutive days immediately prior to
the application, (3)the individual meets all of the eligibility criteria for participation in the waiver program, and
(4)the home and community services to be provided to the individual will qualify for Federal matching funds.
161
Chapter 6: Transitioning People from Institutions to the Community
Use of Peers to Facilitate Transition
Utah developed a statewide network of trained
ILC transition coordinators and peer mentors
who can provide information to any nursing
home resident contacting an Independent Liv-
ing Center for transition services.
State transition program sta should anticipate
some resistance to transition activities among
nursing home sta and family members. Several
Systems Change NFT Grantees considered such
resistance to be a major transition barrier. Some
nursing facility sta do not believe that individuals
with extensive functional limitations or medical and
nursing needs can be safely served in the commu-
nity. In addition, some nursing facilities may actively
resist transition eorts, believing that such eorts
will decrease their occupancy rates and protabil-
ity. Even if families do not oppose their relative’s
transition, their ability to support it and/or provide
informal care depends on a wide range of factors,
including work commitments, available time and
money, distance from their home, and the age of
any dependent children. In some instances, family
members may not want to provide informal care,
particularly if the relative’s admission to a nurs-
ing facility followed many years of informal care at
home and caregiver “burnout.”
Dealing with resistance can require considerable
time and eort, and in some cases such resistance
may pose an insurmountable transition barrier,
particularly if the individual seeking transition has
extensive needs and no family or friends willing or
able to provide informal care. (See the Resources
section of this chapter for publications describing
nursing facility transition programs.)
Involving and Collaborating with
Key Stakeholders
29
To develop processes and procedures that will
result in the successful relocation of nursing home
residents who are appropriate for home and com-
munity settings, states need to take account of the
interests of multiple stakeholders. Stakeholders
include consumers, families, consumer advocates,
nursing facility administrators and discharge plan-
ners, HCBS providers, Independent Living Centers,
housing authorities, and state agency sta.
A good way of taking these interests into account,
and thus increasing an NFT program’s chance of
success, is to develop relationships and partner-
ships with these key stakeholders, particularly at the
direct service level (e.g., the community organiza-
tions that provide services and supports), which
can facilitate eective coordination of transition
activities. Involving nursing facility provider associa-
tions in one project’s work group helped the project
to succeed by allaying providers’ fears and gaining
their support. Project sta also made presenta-
tions to individual nursing facilities to introduce the
program and answer questions from administrators,
directors of nursing, and social services sta; this
strategy proved to be valuable, as about 85 percent
of the project’s referrals came from nursing facilities.
Some stakeholders can assist the state Medicaid
program with identifying the home and community
service infrastructure necessary for a successful
transition, and can help design service and support
systems. It is important that the key stakeholders
involved include individuals or groups with experi-
ence in moving people out of nursing facilities and
that they be involved at the earliest feasible point in
the process.
In general, states need to use two approaches to
develop a successful and sustainable transition
program: (1)a “top-down” approach that elicits the
involvement and support of the leadership of key
agencies to reduce barriers and urge cooperation;
and (2)a “bottom-up” approach of fostering coop-
erative sta relationships in the eld to facilitate
referrals and address specic transition issues. Al-
though eorts to involve stakeholders can be time
consuming, the resulting goodwill and improved
communication ultimately contribute to successful
transitions.
162 Understanding Medicaid Home and Community Services: A Primer
Collaborating with Key Stakeholders:
State Examples
New Jersey’s Community Choice counselors
work in all of the State’s nursing homes and have
developed invaluable collaborative relationships
with nursing home social workers and admission
sta. This collaboration enables dialogue and
cooperation, thereby facilitating the transition
process.
North Carolina established 16 regional coali-
tions to work on nursing facility transitions,
and the Divisions of Medical Assistance and
Vocational Rehabilitation Services, as well as
Independent Living Centers, use state, local, and
private resources to provide transition services.
Nebraska created transition partnerships
statewide among all the State’s Area Agencies
on Aging (AAAs) and nursing facilities to identify
residents who were likely candidates for transi-
tion and to facilitate successful transitions for
those candidates. The State also established a
statewide toll-free number for nursing facility
transition assistance that routes callers to the
appropriate AAA.
Developing and Implementing Case Manage-
ment/Service Coordination Systems That Sup-
port Transition
30
The primary service needed to ensure a success-
ful transition is case management, also called care
management, service coordination, transition
coordination, or relocation assistance. In general,
individuals with severe disabilities and medical
needs who have no informal care will require more
intensive case management than those with lesser
needs. Individuals without their own or family hous-
ing in the community will also require assistance in
nding aordable and accessible housing.
Transition case management is an intensive pro-
cess that includes a range of activities: identifying
and coordinating services, motivating participants,
working with participants’ families or friends, as-
sisting participants in nding housing and other
resources, and assessing participants’ living arrange-
ments for health and safety issues. The use of a per-
son-centered planning format—one that involves
all stakeholders in the transition—enables the de-
velopment of a cohesive transition and service plan,
which is essential to successful and safe transitions.
With regard to specic case management practices,
having transition sta present on the day of reloca-
tion can help to ensure a smooth transition.
Medicaid allows states to pay for case management
services related to transitioning an individual from
an institution, as long as they do not duplicate regu-
lar discharge planning services paid for through
Medicaid or another source. Medicaid-reimbursable
case management services that help to ensure a
successful transition include the following:
• Discussing options with the resident.
• Arranging visits to potential settings and as-
sisting the resident to obtain essential furni-
ture and household items.
• Providing education and training for the resi-
dent prior to discharge.
• Arranging transportation on moving day.
• Implementing a plan of care so that services
are available immediately when the individual
moves.
Three options are available for obtaining Medi caid
reimbursement for case management servi ces: case
management as a waiver service, the tar geted case
management option, and administrative claiming.
31
(The advantages and drawbacks of each of these
payment methods are described in Chapter 4.)
The targeted case management option is likely to
oer the most exibility because it can be targeted
specically to persons who are being transitioned.
The Federal statute denes targeted case manage-
ment as “services which assist an individual eligible
under the plan in gaining access to needed medical,
social, educational, and other services.” This deni-
tion enables states to coordinate a broad range of
activities and services outside the Medicaid pro-
gram, which are necessary for the optimal function-
ing of a Medicaid beneciary in the community.
State Plan targeted case management services must

163
Chapter 6: Transitioning People from Institutions to the Community
include the following four components: assessment
of need, plan of care development, referrals and
linkages, and monitoring and follow up activities.
States desiring to provide transition case manage-
ment services under the targeted case manage-
ment option may do so by amending their State
Plans accordingly. If a state does not plan to oer
the service to all Medicaid recipients, the amend-
ment must specify precisely the group or groups to
be served.
CMS policy regarding case management services
specically recognizes that some individuals may
require a considerable amount of time to transition
to the community. It is possible to obtain Medicaid
funding for case management services provided
during the last 180 consecutive days of a Medicaid-
eligible person’s institutional stay, if provided for
the purpose of community transition. When case
management services are provided under the tar-
geted case management option, states may specify
a shorter time period or other conditions under
which the services may be provided.
32
Case management furnished as a service under an
HCBS waiver program may also be provided to insti-
tutionalized persons during the last 180 consecutive
days prior to discharge. However, Federal nancial
participation (FFP) is available only on the date the
person leaves the institution and is enrolled in the
waiver. In these cases, the cumulative total amount
paid is claimed as a special single unit of transitional
case management. (See the Resource section of this
chapter for a link to CMS State Medicaid Director
letters providing guidance on this topic.)
Although Medicaid policy regarding case manage-
ment is exible and allows payment for services
over a 6-month period, states need to ensure that
the amount of case management it covers is su-
cient—particularly for nursing home residents who
lack housing, have weakened community connec-
tions, or are dependent on the institutional environ-
ment. In such instances, the individual’s needs may
exceed case managers’ ability and time to provide
the services needed. States need to ensure both a
sucient number of case managers and sucient
time for them to complete complex transitions.
Connecticut funds six full-time transition
coordinators to provide outreach and transition
services, and a toll-free line for nursing facil-
ity residents that gives them direct access to a
transition coordinator.
Ensuring adequate transition capacity may require
education and training for hospital and nursing
home discharge planners, nursing facility sta,
and community case managers about home and
community services, generally, and nursing facility
transition, specically.
Identifying and Addressing Housing Needs
and Rental Assistance
Lack of accessible, aordable, and safe housing
is a major transition barrier. Waiting lists for both
services and rental assistance present a major
coordination challenge. Individuals may receive a
rental assistance voucher after waiting a year but
be unable to use it because a waiver slot is not yet
available. Only those individuals with informal sup-
port may have the option of transitioning and then
waiting for waiver services. In some cases, individu-
als may remain in nursing facilities solely because
there are no other housing alternatives.
Housing requirements dier, depending on indi-
vidual needs. States have been working with their
regional and local housing authorities with vary-
ing degrees of success to come up with creative
solutions to housing problems. Stronger partner-
ships between health/long-term care and housing
authorities at both the state and Federal levels
are often cited as the most important need in the
search for comprehensive approaches to maintain-
ing people in the community.
Successfully addressing housing issues often
requires considerable time and eort. The services
of a dedicated housing coordinator are invaluable
in helping nursing facility residents nd suitable
housing. This individual can also work at the policy
level to increase awareness of the need for housing
for persons relocating and to address the need for
aordable, accessible housing for all persons with
disabilities.
164 Understanding Medicaid Home and Community Services: A Primer
If dedicated sta are not feasible, one way of nd-
ing aordable, accessible housing is to call housing
unit managers and developers to let them know
of unmet need and to impress on them the impor-
tance of notifying transition counselors of available
units. Once potential housing has been identied,
it is benecial to have nursing home residents visit
the prospective residence or apartment in order to
identify any potential problems or barriers in ad-
vance—for example, a physical layout that does not
accommodate their needs.
Some states are using Housing and Urban Devel-
opment (HUD) Section 8 rental vouchers for indi-
viduals who are transitioning to help them secure
aordable, accessible housing. Housing authorities
in some Maryland counties changed their prior-
ity criteria on housing voucher set-asides to allow
persons in a nursing facility who are on the housing
voucher list to move to the top of the list when they
become eligible for waiver services. Similarly, the
Spokane Housing Authority in Washington State has
designated individuals leaving nursing facilities as
“homeless,” enabling them to bypass a 2-year wait-
ing list for rental assistance vouchers. An Indepen-
dent Living Center in Spokane now has an ongoing
process for assisting nursing facility residents with
housing voucher applications. Waiver transition
funds or state general funds pay for this service.
33
Other states have created rental assistance pro-
grams for individuals seeking diversion or transition
from nursing facilities, such as Arkansas’s Bridge
Rental Assistance Program, which bridges the gap
between income and the cost of aordable apart-
ments for persons transitioning or being diverted
from nursing homes.
34
Arkansas’s Bridge Rental
Assistance Program
The Arkansas Supported Housing Oce and the
Governor’s Task Force on Supported Housing
recommended the creation of a rental assistance
program for individuals who are being diverted
or are transitioning from nursing homes. Under
the State’s Nursing Facility grant initiatives, Spa
Area Independent Living Services, the Arkansas
Development Finance Authority, and Arkansas
Rehabilitation Services developed and imple-
mented the Bridge Rental Assistance Program.
Individuals who apply for Section 8 vouchers
and are on a waiting list are provided a monthly
rental stipend for up to 2 years, while case
managers work with them to create and execute
a plan for housing self-suciency. The Bridge
Rental Assistance Program is being sustained
through funding from the Arkansas Develop-
ment Finance Authority.
35
Assessments for Accessibility
Environmental modications are often crucial to a
state’s ability to serve an individual in the commu-
nity. Federal nancial participation may be available
for the costs of assessing accessibility and the need
for modications in a person’s home or vehicle in
three ways. First, FFP may be claimed at the admin-
istrative rate for assessments to determine whether
the person’s home or vehicle requires modications
to safeguard the health and welfare of an HCBS
waiver participant. (Assessment costs incurred to
determine whether an individual’s needs can be
met under an HCBS waiver may qualify for FFP re-
gardless of whether or not the person is eventually
served under the waiver.)
Second, the cost of environmental assessment may
be included in the cost of environmental modica-
tions under an HCBS waiver. Third, the assessment
may be performed by another service provider,
such as a home health agency or an occupational
therapist; if so, FFP is available at the service match
rate for these providers when they perform the as-
sessment in addition to their other duties. (See the
Resource section of this chapter for the link to the

165
Chapter 6: Transitioning People from Institutions to the Community
State Medicaid Director letter regarding payment
of assessments for accessibility and environmental
modications.)
Providing Flexible Funding Mechanisms
Many resources are needed to help individuals relo-
cate from nursing facilities to community settings,
including but not limited to subsidized accessible
housing, transition funds, services and supports,
and a wide range of local community resources,
including transportation. To provide adequate
services for individuals who are transitioning, it may
be necessary to combine services from multiple
funding sources, for example, HCBS waiver services,
home health services, and state-funded programs.
Inexible funding streams and a lack of mechanisms
to coordinate funding can pose transition barriers.
Because Medicaid-eligible residents in institutions
have only a small monthly personal needs allow-
ance, they lack the nancial resources to pay for
one-time transition expenses, such as security de-
posits for rent, utilities, and phone service, and es-
sential furniture and household items. CMS permits
coverage of these one-time transition expenses
under HCBS waiver programs. The CMS HCBS waiver
application denes these expenses as Community
Transition Services:
Community Transition Services are non-recurring
set-up expenses for individuals who are transi-
tioning from an institutional or other provider-
operated living arrangement to a living arrange-
ment in a private residence where the person
is directly responsible for his or her own living
expenses.
Allowable expenses are those necessary to en-
able a person to establish a basic household
that do not constitute room and board and may
include (a)security deposits that are required
to obtain a lease on an apartment or home;
(b)essential household furnishings required to
occupy and use a community domicile, including
furniture, window coverings, food preparation
items, and bed/bath linens; (c)set-up fees or
deposits for utility or service access, including
telephone, electricity, heating and water; (d)ser-
vices necessary for the individual’s health
and safety such as pest eradication and one-
time cleaning prior to occupancy; (e)moving
expenses; (f)nec essary home accessibility ad-
aptations; and, (g)activities to assess need,
arrange for and procure needed resources.
Community Transition Services are furnished
only to the extent that they are reasonable and
necessary as determined through the service
plan development process, clearly identied
in the service plan, and the person is unable to
meet such expense or when the servi ces cannot
be obtained from other sources. Community
Transition Services do not include monthly
rental or mortgage expense; food, regular utility
charges; and/or household appliances or items
that are intended for purely diversional/recre-
ational purposes.
States are permitted to supplement or modify this
denition to reect the specic expenses they want
to include in their waiver program and may also list
expenses that are specically excluded. While Fed-
eral law prohibits Medicaid payment for room and
board, payment of a security deposit to a landlord is
not considered rent. Medicaid Community Transi-
tion Services may not be used to pay for furnishing
living arrangements that are owned or leased by a
waiver service provider where the provision of these
items and services are inherent in the service they
are already providing.
One-time transition expenses for waiver partici-
pants can be billed when the individual leaves the
institutional setting and becomes a waiver partici-
pant. For these expenses to be reimbursable, the in-
dividual must be reasonably expected to be eligible
for and to enroll in the waiver. If for any reason the
individual does not enroll in the waiver (e.g., due to
death or a signicant change in condition), transi-
tion expenses may be billed to
Medicaid as an administrative cost.
Some states have chosen to use state funding for
transition expenses. New Jersey began covering
transition expenses under the Enhanced Commu-
nity Options and Assisted Living waiver programs.
For persons ineligible for these waivers, transition
expenses can be covered through a special fund
established under the State’s Systems Change NFT
166 Understanding Medicaid Home and Community Services: A Primer
grant. Two other states—Ohio and Wyoming—have
also appropriated funds to cover one-time transi-
tion expenses not covered by
Medicaid.
36
South Carolina added a nursing facility transi-
tion services package to the Elderly and Dis-
abled waiver that covers housing and utility
deposits and basic furniture and appliances. All
items must be required by the service plan, and
total expenditures are capped at $1,000. The
State also enhanced coverage for environmental
modications for all waiver participants, and
now covers bath safety items and door widen-
ing.
37
Individuals who are receiving Medicaid-funded
institutional services have had to spend down their
assets and some may have credit issues that pre-
vent them from obtaining phone, utility, and other
services that require a good credit history. Transition
coordinators need to address this potential barrier
early in the planning process.
Preventing Unnecessary Admissions
and Avoidable Long Stays
Although transitioning people out of institutions
can save money over the long term, the process can
incur major costs, and not all may be reimbursable
by Medicaid. Given this, it makes sense for states
to consider strategies that will divert people from
entering institutions in the rst place and ensure
a quick return to the community if placement is
unavoidable.
The ICFs/ID experience illustrates that the best
transition program is one that makes sure that very
few people will need to be transitioned. In the ID/
DD eld, this is known as the front door/back door
connection. Little progress with transitioning can
be made as long as the front door to the institution
remains open; intervention before inappropriate
placement (i.e., diversion) is easier than intervention
after placement.
Establishing a Quality Assurance
System That Eectively Balances
Risk and Autonomy
Community living presents a dierent set of risks
from those associated with living in an institution.
Transition programs need to have a quality assur-
ance (QA) system that monitors and helps ensure
service quality and client safety, particularly in the
immediate period after transition and for the rst
few months. At the same time, however, such a
QA system must respect individuals’ autonomy by
acknowledging their choice to assume risk. The
balance is delicate and can be hard to achieve. Pro-
grams that use a participant direction model allow
individuals to assume more responsibility and ac-
countability than those that use an agency-directed
model. (See Chapter 7 for a full discussion of partici-
pant direction service delivery models).
The assurances CMS requires from states for ap-
proval of HCBS waiver services include “necessary
safeguards” to safeguard the “health and welfare” of
persons receiving services in the community. Since
HCBS waiver programs serve a diverse array of tar-
get populations, no one-size-ts-all application of
these QA requirements can be prescribed. (See the
Appendix for an overview of CMS requirements for
quality management and improvement systems.)
167
Chapter 6: Transitioning People from Institutions to the Community
Diversion Strategies: State Examples
Several states have recognized the need to prevent both unnecessary nursing facility admissions and unneces-
sarily long stays that result in a loss of housing.
Rhode Island developed a protocol for the State’s long-term care nurses—who conduct level-of-care determina-
tions and Level I Preadmission Screening and Resident Review (PASRR)
38
—to identify and refer individuals who
do not appear to be at risk for a long stay when admitted. Based on the success of this protocol, in 2005 the State
enacted a statute requiring that registered nurses (RNs) reevaluate all new nursing facility admissions 45 days
after admission. The RNs who perform level-of-care and PASRR determinations ag individuals who appear to
require only a short stay, and a computer-generated letter to this eect is sent to the resident and the nursing
facility. A computer-generated reminder is sent to the RNs 45 days after admission, instructing them to evaluate
the most recent MDS assessment to determine whether a continued stay is required.
39
Rhode Island also enacted a statute in 2004 requiring the Department of Human Services (DHS) to inform
nursing facility residents about home and community services that may enable them to live in a less restrictive
community setting or their own home. The law requires DHS to mail a brochure describing the range of available
services to all nursing facility residents whom the state long-term care nurses have identied as likely candidates
for discharge within several months of admission.
40
Nebraska operates a nursing facility preadmission program—Senior Care Options (SCO)—to ensure that
Medicaid applicants in need of nursing facility care receive information on alternative choices appropriate to
their level of care. SCO sta, located throughout the State, are trained to use the Blaylock Risk Assessment Scor-
ing System (BRASS) screening tool, an instrument that identies patients at risk for prolonged hospital stays at
admission and in need of discharge planning services; BRASS can also be used to identify individuals at risk for
long nursing home stays.
As a result of positive experience with the tool, the State changed its preadmission screening procedures. Every
AAA now employs the BRASS tool for preadmission screening to identify individuals who should be reassessed in
3 to 6 months. For these individuals, Medicaid provides only a short-term authorization to
enter a nursing home so that they will have to be reassessed to remain there. This change has led to active dis-
charge planning to return new admissions to the community, and has resulted in shorter nursing home stays.
41
Nebraska also allows service coordinators to authorize waiver services for individuals who will likely be eligible
for Medicaid coverage. Based on basic nancial information provided by the applicant, the service coordinator
consults with a Medicaid eligibility worker who can judge whether it appears that the applicant will be eligible
for Medicaid. If, ultimately, the applicant is not eligible, the State uses funds from the Social Services Block Grant
to pay for services, which has occurred only twice over a 2-year period.
42
New Jersey’s preadmission screening process for all nursing home admissions designates Medicaid beneciaries
as “Track One” or “Track Two” depending on whether they are likely to remain in the facility for a long or short pe-
riod of time. All short-term residents receive a letter indicating that they are certied for 6 or fewer months and
are contacted by Community Choice counselors who work with them to develop a relocation plan.
43

168 Understanding Medicaid Home and Community Services: A Primer
Resources
Since the Primer was rst published in 2000, numerous reports and other resources have become available
on the Internet. This section includes key resources relevant to transitions. Most of the publications cite ad-
ditional resources and the websites also have links to other information sources.
Publications
Centers for Medicare & Medicaid Services. (2008). Application for a §1915(c) Home and Community-
Based Waiver [Version 3.5]: Instructions, Technical Guide and Review Criteria.
This publication contains extensive information concerning Federal policies that apply to the operation of an
HCBS waiver, in particular, Appendix C-3: Waiver Services Specications, and C-3H: Services to Facilitate the
Transition of Institutionalized Persons to the Community.
Available at https://www.hcbswaivers.net/CMS/faces/portal.jsp under links and downloads, entitled §1915(c)
Waiver Application and Accompanying Materials.
O’Keee, J., O’Keee, C., Greene, A.M., and Anderson, W. (2008). Enduring Changes of the FY 2001 and FY
2002 Nursing Facility Transition Grantees. Baltimore, MD: Centers for Medicare & Medicaid Services.
This issue brief provides a summary overview of the accomplishments and enduring changes brought about
by all of the Systems Change NFT Grantees. Despite achieving many enduring systems improvements, Grant-
ees reported that many transition barriers remain. Grantees made recommendations to help states address
continuing barriers to nursing facility transition and diversion.
Available at http://www.hcbs.org/moreInfo.php/doc/2353
O’Keee, J., O’Keee, C., Osber, D., Siebenaler, K., and Brown, D. (2007). FY 2002 Nursing Facility Transi-
tion Grantees: Final Report. Baltimore, MD: Centers for Medicare & Medicaid Services.
This report provides an overview of the 16 FY 2002 Systems Change NFT Grantees’ initiatives to either establish
or improve NFT programs or to help develop some components of an NFT infrastructure. The report includes
lessons learned and recommendations that can guide states that are undertaking similar initiatives.
Available at http://www.hcbs.org/moreInfo.php/doc/2060
169
Chapter 6: Transitioning People from Institutions to the Community
O’Keee, J., O’Keee, C., Siebenaler, K., Brown, D., Anderson, W., Greene, A.M., and Osber, D. (2006). FY
2001 Nursing Facility Transition Grantees: Final Report. Baltimore, MD: Centers for Medicare & Medicaid
Services.
This report provides an overview of the 17 FY 2001 Systems Change NFT Grantees’ initiatives to either establish
or improve NFT programs or to help develop some components of an NFT infrastructure. The report includes
lessons learned and recommendations that can guide states that are undertaking similar initiatives. The report
was referenced on page 48 of the CMS MFP Demonstration Solicitation Document.
Available at http://www.hcbs.org/moreInfo.php/doc/1678
Siebenaler, K., O’Keee, J., Brown, D., and O’Keee, C. (2005). Nursing Facility Transition Initiatives of
the Fiscal Year 2001 and 2002 Grantees: Progress and Challenges. Baltimore, MD: Centers for Medicare &
Medicaid Services.
This report provides an overview of the NFT initiatives implemented by 18 of the FY 2001 and FY 2002 Systems
Change Grantees. It describes their diering approaches to nursing facility diversion and/or transition within
a framework of the key steps needed to create NFT programs that are integrated into a state’s long-term care
system. This report also identies the transition challenges and policy issues facing states and Independent
Living Centers, discusses lessons learned from grant initiatives, and recommends programmatic and policy
changes needed to support transitions.
Available at http://www.hcbs.org/moreInfo.php/doc/1308
Eiken, S., Holtz, D., and Steigman, D. (2005). Medicaid HCBS Waiver Payment for Community Transition
Services: State Examples. Cambridge, MA: Thomson Reuters.
This topic paper summarizes how states can use Medicaid to pay for most institutional transition program
costs. It also describes how states are currently using Medicaid HCBS waivers to pay for Community Transition
Services—temporary supports people need when trying to move, such as housing depos its, utility set-up fees,
and furniture.
Available at http://www.hcbs.org/moreInfo.php/doc/1192
Summer, L. (2005). Strategies to Keep Consumers Needing Long-Term Care in the Community and Out of
Nursing Facilities. Washington, DC: Kaiser Commission on Medicaid and the Uninsured.
In recent years, states have been trying to shift resources from institutions to home and community services.
This report examines transition and diversion policies and practices in eight states. It provides a sense of what
state Medicaid programs are doing or could be doing to promote diversion. The report has a 10-page execu-
tive summary.
Available at http://www.hcbs.org/moreInfo.php/doc/1442
170 Understanding Medicaid Home and Community Services: A Primer
Websites
Centers for Medicare & Medicaid Services
CMS issues State Medicaid Director letters to clarify Medicaid policy and provide guidance to states to ensure
consistency in its application. The initial Olmstead decision letter, dated January 14, 2000, and subsequent up-
dates, can be accessed at the following website by using the word “Olmstead” in the search criteria. In particu-
lar, Olmstead Update #3, July 25, 2000, includes Attachment 3-b, Community Transition, which discusses policy
changes related to case management services, assessments for accessibility, and environmental modications.
Web address: http://www.cms.hhs.gov/SMDL/SMD/list.asp#TopOfPage
In 2007, CMS awarded MFP grants to 30 states and the District of Columbia, proposing to transition 37,731 in-
dividuals out of institutional settings over a 5-year demonstration period. The MFP demonstration is the most
ambitious program to date aimed at helping Medicaid enrollees transition from long-term care institutions to
the community. A series of reports are being completed as part of the MFP national evaluation and are avail-
able at the following website.
Web address: http://www.cms.hhs.gov/DecitReductionAct/20_MFP.asp#TopOfPage
The Clearinghouse for Home and Community Based Services
This site promotes the development and expansion of HCBS by gathering resources and tools for research,
policymaking, and program development into this one-stop website. Under the topic Transition/Diversion
from Institutions, there are 302 publications and other resources, including all of the publications listed above,
and also many states’ promising practices for facilitating nursing facility to community transitions.
Web address: http://www.hcbs.org/
171
Chapter 6: Transitioning People from Institutions to the Community
Endnotes: Citations, Additional Information,
and Web Addresses
1
Gavin Kennedy, Gary Smith, and Janet O’Keee co-authored the original chapter. Janet O’Keee and
Charles Moseley updated the chapter.
2
The Court armed the rights of qualied individuals with disabilities to receive services in the most in-
tegrated settings appropriate to their needs. Under the Court’s decision, states are required in specic
circumstances to provide community services for persons with disabilities who would otherwise be
entitled to institutional services. See Introduction for more information on the Olmstead decision.
3
The information in this section is drawn from Prouty, R.W., Alba, K., and Lakin, K.C. (Eds.). (2008). Resi-
dential Services for Persons with Developmental Disabilities: Status and Trends through 2007. Min-
neapolis, MN: University of Minnesota Research and Training Center on Community Living, Institute
on Community Integration. Available at http://rtc.umn.edu/docs/risp2007.pdf. Additional print copies
may be requested by contacting Naomi Scott at [email protected] or 612-624-8246.
4
HCBS waiver programs are authorized under Section (§)1915(c) of the Social Security Act.
5
Braddock, D., Hemp, R., and Rizzolo, M.C. (2008). The State of the States in Developmental Disabilities,
2008. Boulder, CO and Washington, DC: Department of Psychiatry and Coleman Institute for Cognitive
Disabilities, University of Colorado, and American Association on Intellectual and Developmental Dis-
abilities.
6
New Hampshire, Vermont, Rhode Island, West Virginia, Maine, New Mexico, Alaska, Hawaii, Indiana,
and Oregon.
7
Prouty, R.W., Alba, K., and Lakin, K.C. (Eds.). (2008), op. cit.
8
Institutional services for persons with developmental disabilities are generally much more costly than
nursing home services.
9
Although the need for such intensive services may continue indenitely for some persons, for others,
the level of support required may decrease over time.
10
Additional Federal matching funds were provided to states transitioning people from institutions to
community services under the Federal MFP state demonstration grants to assist them with developing
the necessary community infrastructure, among other objectives.
11
While per capita service plans may exceed the average cost of institutional services, the aggregate
costs for the waiver program must meet Medicaid cost neutrality requirements.
12
Smith, G., Fortune, J., and Agosta, J. (2006). Gauging the Use of HCBS Supports Waivers for People with
Intellectual and Developmental Disabilities: Proles of State Supports Waivers. Washington, DC: U.S.
Department of Health and Human Services, Oce of the Assistant Secretary for Planning and Evalu-
ation, Oce of Disability, Aging, and Long-Term Care Policy. Available at http://aspe.hhs.gov/daltcp/
reports/2006/gauging.htm.

172 Understanding Medicaid Home and Community Services: A Primer
13
Prouty, R.W., Alba, K., and Lakin, K.C. (Eds.). (2008), op. cit.
14
Version 3.5. See the Resources section of this chapter for a web link to the waiver application, instruc-
tions, and technical guidance.
15
NFT grants were provided to state agencies—called State Program grants—and to Independent Liv-
ing Centers—called Independent Living Partnership (ILP) grants. The purpose of the ILP grants was to
capitalize on ILC expertise to develop outreach materials, identify and support nursing facility resi-
dents who want to transition, provide technical assistance, and supplement state transition infrastruc-
ture.
16
These are not the grants awarded through the MFP demonstration authorized under the Decit Re-
duction Act of 2005 (DRA-2005).
17
Additional challenges are involved when downsizing or closing an institutional facility, including en-
suring that any special services provided in the facility will be available to individuals after they have
left the institution, maintaining the quality of facility services and worker morale, assisting workers to
nd other employment, and addressing the “dual funding” problem (i.e., meeting the costs of main-
taining facility operations while underwriting the costs of community placement).
18
Information in this section draws liberally from O’Keee, J., O’Keee, C., Greene, A.M., and Anderson,
W. (2008). Enduring Changes of the FY 2001 and FY 2002 Nursing Facility Transition Grantees. Balti-
more, MD: Centers for Medicare & Medicaid Services. Available at http://www.hcbs.org/moreInfo.php/
doc/2353.
19
Information in this section draws liberally from O’Keee, J., O’Keee, C., Greene, A.M., and Anderson,
W. (2008), op. cit.
20
See CMS Press Release, available at http://www.hcbs.org/moreInfo.php/doc/1909. See also CMS
website about the MFP demonstration at http://www.cms.hhs.gov/DecitReductionAct/20_MFP.
asp#TopOfPage.
21
Section 6071 of DRA-2005.
22
P.L. 111-148(signed on March 23, 2010) and the Health Care and Education Reconciliation Act of 2010
(signed on March 30, 2010).
23
The reports and other information concerning the MFP demonstration can be found at http://www.
cms.hhs.gov/DecitReductionAct/20_MFP.asp.
24
Texas Health and Human Services Commission. Medicaid Reform Strategies for Texas. February 2007.
25
Federal law mandates use of the MDS for all residents of facilities that are certied to participate in
Medicare or Medicaid skilled nursing facilities and hospital-based skilled nursing units. These facilities
are required to conduct comprehensive, accurate, standardized, and reproducible assessments of each
resident’s functional capacity, using a Resident Assessment Instrument (RAI). The RAI consists of the
MDS, Resident Assessment Protocols, and Triggers.
26
O’Keee, J., O’Keee, C., Greene, A.M., and Anderson, W. (2008), op. cit.
27
Ibid.
28
O’Keee, J., O’Keee, C., Osber, D., Siebenaler, K., and Brown, D. (2007). FY 2002 Nursing Facility Tran-
sition Grantees: Final Report. Baltimore, MD: Centers for Medicare & Medicaid Services. Available at
http://www.hcbs.org/moreInfo.php/doc/2060.

173
Chapter 6: Transitioning People from Institutions to the Community
29
Information in this section draws liberally from O’Keee, J., O’Keee, C., Osber, D., Siebenaler, K., and
Brown, D. (2007), op. cit.
30
Ibid.
31
Case management can also be provided as an integral and inseparable part of another covered ser-
vice.
32
Medicaid funding is not available for targeted case management services provided to persons who are
receiving services in an institution for mental disease, except for services provided to elderly individu-
als and children under the age of 21 who are receiving inpatient services.
33
O’Keee, J., O’Keee, C., Greene, A.M., and Anderson, W. (2008), op. cit.
34
Ibid.
35
O’Keee, J., O’Keee, C., Osber, D., Siebenaler, K., and Brown, D. (2007), op. cit.
36
Ibid.
37
Ibid.
38
Medicaid regulations require states to maintain a program to screen nursing facility applicants and
residents for serious mental illness and intellectual disability. The program’s intent is to ensure that
individuals are placed in the most appropriate setting and have access to specialized mental health
services where appropriate. To do this, the program uses a progressive screening process to assess
whether applicants for nursing facilities have a mental illness or an intellectual disability, and if the
nursing facility is an appropriate placement.
The rst test, Level I, screens for potential mental illness. All those who test “positive” must receive a
more in-depth screen—Level II—that more accurately identies mental illness and assesses whether
the individual needs specialized services and nursing facility level of care. Linkins, K., Lucca, A., Hous-
man, M., and Smith, S. (2006). PASRR Screening for Mental Illness in Nursing Facility Applicants and
Residents. Report prepared for the U.S. Department of Health and Human Services, Substance Abuse
and Mental Health Services Administration, Center for Mental Health Services. Available at http://
download.ncadi.samhsa.gov/ken/msword/SMA05-4039.doc.
39
O’Keee, J., O’Keee, C., Greene, A.M., and Anderson, W. (2008), op. cit.
40
O’Keee, J., O’Keee, C., Osber, D., Siebenaler, K., and Brown, D. (2007), op. cit.
41
O’Keee, J., O’Keee, C., Greene, A.M., and Anderson, W. (2008), op. cit.
42
Example taken verbatim from the Executive Summary of Summer, L. (2005). Strategies to Keep Con-
sumers Needing Long-Term Care in the Community and Out of Nursing Facilities. Washington, DC:
Kaiser Commission on Medicaid and the Uninsured. Available at http://www.hcbs.org/moreInfo.php/
doc/1442.
43
Ibid.

174 Understanding Medicaid Home and Community Services: A Primer

Chapter 7: Participant-Directed Services and Supports
175
Guide to Chapter 7
Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .177
Evolution of Participant Direction of Medicaid HCBS . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .178
Basic Features of Participant Direction of Medicaid HCBS . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .179
Federal Medicaid Statutory Authorities . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .180
1. State Plan Coverage of Personal Care . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .181
2. HCBS Waiver Authority . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .183
3. State Plan Coverage of HCBS . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .185
4. State Plan Coverage of Participant-Directed Personal Assistance Services . . . . .186
5. State Plan Community First Choice Option . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .188
Service Planning and Authorization . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .189
Use of Representatives . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .190
Individualized Backup Plans . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .190
Building Flexibility into the Service Plan While Ensuring Equitable Budgets . . . . . .191
Employing Family Members . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .192
Non-Personal Care Services . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .192
Furnishing Assistance to Individuals in Managing and Directing Services . . . . . . . . . . . . . . .193
Information and Assistance . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .193
Financial Management Services . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .195
Performance of Skilled Nursing Tasks . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .199
Resources. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .200
Endnotes: Citations, Additional Information, and Web Addresses . . . . . . . . . . . . . . . . . . . . . . .203
177
Chapter 7: Participant-Directed Services and Supports
Chapter 7
Participant-Directed Services and Supports
Like those without disabilities, individuals with disabilities want and expect to control their own lives. This includes
having a direct say about the home and community services and supports they receive through the Medicaid pro-
gram and the individuals who provide them. Virtually every state now has at least one participant direction pro-
gram under Medicaid that provides options for individuals to direct and manage their own services and supports,
with the assistance of family members when needed. Participant-directed services are an alternative to—and can
be oered alongside—the traditional service delivery model. This chapter describes the main features of partici-
pant-directed home and community services, and the interplay between participant direction options and Medicaid
policy. It focuses on services furnished through ve Medicaid authorities, including Section (§)1915(c) waivers, the
§1915(i) Home and Community-Based Services (HCBS) State Plan benet, and §1915(j) Participant-Directed Per-
sonal Assistance Services. Medicaid gives states the authority to provide a full range of options for participant direc-
tion—on a continuum from less to more control and responsibility.
1
Introduction
Participant direction, referred to alternatively as consumer direction, self-direction, and participant-driven
supports, is a service model that oers individuals and their families the opportunity, support, and authority
to choose the services they need and direct the individuals who provide them.
2
Participant direction principles
have broad applicability for individuals of all ages who need long-term care services and supports (hereafter
called services and supports) due to physical or cognitive impairments, including those caused by serious
mental illness, a developmental condition, or dementia.
Participant direction has been demonstrated to promote positive outcomes for individuals and their families,
improve participant satisfaction, and increase access to needed services.
3
Participant direction service models
can be a means to involve individuals and families in quality assurance and improvement eorts, promote ef-
fective service delivery, and improve participant satisfaction with services.
4
For individuals with intellectual disabilities and other developmental disabilities (hereafter referred to as
developmental disabilities), participant-directed services are considered an essential element of self-determi-
nation, the philosophy that continues to reshape the provision of services and supports for this population.
A key principle of self-determination is that individuals should have the authority to direct and manage their
own lives, including their services. Individuals may invite and enlist friends and family members to assist them
in directing and managing services.
5
An individual’s legal representative or surrogate decision maker may also
provide assistance and advice and perform some service management tasks (as they can for all individuals
who need assistance to direct their services).
178 Understanding Medicaid Home and Community Services: A Primer
Participant direction models can operate side by
side with traditional service delivery models, so
individuals and families can choose the extent to
which they wish to manage their services. Those
who want to exercise a high level of control can se-
lect participant direction options, while others can
have services and supports managed by a provider
agency.
Evolution of Participant Direction of
Medicaid HCBS
Participant direction of Medicaid home and com-
munity services began in the 1970s when a few
states launched Medicaid personal assistance/atten-
dant services programs that authorized Medicaid
participants to hire, train, supervise, and dismiss
their workers.
6
During the 1980s and 1990s, the
number of states that authorized Medicaid partici-
pants to manage their workers grew—both through
the Medicaid State Plan Personal Care optional
benet and, starting in 1981, through §1915(c)
home and community-based services waivers
(hereafter referred to as HCBS waivers). In 1997, the
Centers for Medicare & Medicaid Services (CMS)
released formal guidance (discussed in more detail
below) acknowledging that states could employ a
“participant-directed service delivery model” for the
delivery of personal care/assistance services under
the Medicaid State Plan.
In 1995, the Robert Wood Johnson Foundation
(RWJF) and the U.S. Department of Health and Hu-
man Services (HHS) launched the National Cash and
Counseling Evaluation Demonstration.
7
Its aim was
to test a broader approach to participant direction
that gave participants the authority to manage an
individual budget and the latitude to use this bud-
get to purchase goods and services to meet their
service and support needs. The demonstration also
gave participants the option of receiving allowances
in cash to purchase services and supports, or have
their funds deposited with an entity that would per-
form nancial transactions under their direction.
8
In the same year, RWJF also launched its Self-Deter-
mination for People with Developmental Disabilities
Program.
9
RWJF awarded grants to 18 states to cre-
ate pilot programs that gave individuals and fami-
lies a leadership role in the design of person-cen-
tered service plans along with choice and control
over an individual budget to carry out the service
plan. These pilots also featured the provision of in-
dependent counseling services (specically referred
to as Support Broker services) to assist participants
in selecting and managing services, along with s-
cal intermediaries to serve as their agents to handle
employment-related tasks. The Self-Determination
pilots operated within the regulatory connes of
the HCBS waiver program and, therefore, did not
permit individuals or their representatives to receive
any benets directly as “cash.”
In response to the favorable early evaluation results
from the Cash and Counseling Demonstration, ex-
perience garnered through the Self-Determination
pilots, and rapidly growing state interest in oer-
ing participant direction options, CMS launched
its Independence Plus initiative in 2002, which
provided guidance to the states about incorporat-
ing employer and budget authority into a waiver
program.
10
CMS also issued separate templates for
Independence Plus programs operating under the
HCBS and §1115 waiver authorities.
In 2005, CMS extensively modied its standard
HCBS waiver application so that states could include
a participant direction option in any HCBS waiver,
eliminating the need for a separate Independence
Plus waiver. The new waiver application built upon
the predecessor Independence Plus waiver tem-
plate and further claried the Federal policies that
apply when a participant direction option is imple-
mented in an HCBS waiver. To date, at least 37 states
have a participant direction option in one or more
HCBS waivers.
11
However, some states oer only the
employer authority and some have experienced
slow enrollment in participant direction options.
In the Decit Reduction Act of 2005 (DRA-2005),
Congress added two statutory provisions that oer
states additional options to incorporate participant
direction into the delivery of Medicaid HCBS with-
out having to seek Federal waivers.
12
These provi-
sions are discussed in more detail below.
13
In the
space of about 10 years, Federal Medicaid policy has
evolved to provide states with several options to
aord Medicaid participants wide-ranging authority
179
Chapter 7: Participant-Directed Services and Supports
to direct their services and supports, including the
option to direct an individual budget.
Basic Features of Participant
Direction of Medicaid HCBS
The sections below describe in detail the legal
authorities that permit incorporation of participant
direction into the delivery of Medicaid HCBS. While
each authority has unique elements, certain basic
features of participant direction cut across the au-
thorities. These features are described next.
Individual Election of Participant Direction. The
various authorities have dierent requirements re-
garding the provision of alternatives to participant
direction.
• When a state oers participant direction
through an HCBS waiver program, it must
provide that participants may opt into or out
of directing their services, that is, a state must
oer a “provider-managed” service delivery
option alongside the participant direction
option and ensure there are no service breaks
during transition periods.
• Participant direction programs operated
under the State Plan Personal Care benet
are not required to use a particular service
delivery model or to oer more than one
service delivery model; nor are they required
to specify policies for voluntary or involuntary
transition from participant-directed services to
other types of service delivery, such as agency-
provided services.
• If a state chooses to use the §1915(j) authority
to permit self-direction of State Plan personal
care services, it must ensure that participants
may opt into or out of directing their services
and that a traditional service delivery option
is available. Because traditional service
delivery models vary, they are not specied
here. If a state uses the §1915(j) authority in
conjunction with the HCBS waiver authority,
the requirements of the latter authority must
be met.
• Under §1915(i), CMS requires states to have
policies to facilitate voluntary or involuntary
transitions from participant-directed services
to non-participant-directed service delivery
models.
Participant-Led Service Planning Process. Anoth-
er important feature is positioning the participant
(or a personally-selected personal representative) to
lead the person-centered service planning process.
This includes giving participants the authority to
select who participates in the process (e.g., family
members and friends), and ensuring that partici-
pants’ service plans reect their preferences and
goals. Participants are expected to have the author-
ity to select their services and supports, in addition
to exercising free choice of provider, a long-stand-
ing right under Federal Medicaid law.
14
Managing Workers. All of the pertinent Medi caid
authorities allow participants to select, hire, super-
vise, and manage their workers—called the Employ-
er Authority. Under this authority, a state may recog-
nize Medicaid participants (or their representatives)
as the legal (“common law”) employers of their
workers and provide for the use of Fiscal/Employer
Agents (F/EAs) to pay workers and le payroll taxes
on their behalf. A state also may elect to use a “co-
employer” model whereby an organization serves as
the primary or legal employer of participant-hired
workers, while the individual or their representative
serves as the secondary or managing employer.
15
This co-employer model is commonly referred to as
the Agency with Choice model.
Individual Authority Over Service Delivery.
Participant direction of Medicaid services and sup-
ports also allows participants to determine how and
when services are delivered. This includes specify-
ing the elements of services that will be delivered
(within the approved scope of the service(s) that the
state oers), scheduling the delivery of services, and
establishing any additional special qualications for
the workers or agencies that provide services.
16
Individual Budget. Under the §1915(c) and
§1915(j) authorities, participants may be provided
an individual budget that includes some or all of
their service and support funding and the ability to
exercise decision-making authority and manage-
180 Understanding Medicaid Home and Community Services: A Primer
ment responsibility to purchase goods and services
authorized in the service plan—called the Budget
Authority.
17
Participants, with the aid of counselors
(i.e., information and assistance providers) and the
nancial management services entity, assume re-
sponsibility for managing their individual budgets.
Supports for Participant Direction. The §1915(c)
and §1915(j) authorities specically require states
to provide certain key supports to participants who
direct their services: nancial management services
and information and assistance. The proposed rule
for the §1915(i) authority also addresses the provi-
sion of these two support services. However, its
requirements are not included here because at the
time of publication, the rule had not yet been nal-
ized.
• Financial management services. These
services include performing nancial
transactions on behalf of participants (e.g.,
paying workers that participants employ,
deducting payroll taxes, and under the
§1915(c) and §1915(j) authorities, facilitating
the purchase of other goods and services)
along with tracking expenditures against the
individual bud get.
• Information and assistance in directing
services and supports. Medicaid funding is
available to reimburse the costs of personal-
ized assistance to participants in directing
their services. Such assistance may include
(a)counseling participants about available
services and supports, (b)helping them
to acquire the skills to create and manage
the individual budget and to manage their
individually employed workers, (c)assisting
them in locating workers and services, and
(d)accessing other benets and community
resources. States use various terms for this
type of assistance, including counseling,
supports brokerage, supports coordination, or
consulting.
Safeguards. Finally, states are expected to provide
safeguards on behalf of participants who direct
their services. These include ensuring that services
are not interrupted when an individual elects to
transition from participant direction to provider-
managed services, guarding against the premature
depletion of the individual budget, and ensuring
that participants have an individualized backup
plan to handle breakdowns in service delivery.
Under the applicable authorities, states have con-
siderable latitude in how they implement each of
these participant direction features.
Federal Medicaid Statutory Authorities
There are ve principal Medicaid authorities under
which states may implement participant direction
of home and community services. (A sixth author-
ity—a §1115 waiver—is available under certain
conditions
18
[see Box].)
Four of the ve are Medicaid State Plan authori-
ties. A state can add participant direction options
under the State Plan by submitting a State Plan
amendment to CMS for review and approval. Once
approved, it becomes part of the state’s Medicaid
program unless subsequently altered by the state.
The fth is a waiver authority, that is, states can
request waivers of Federal statutory provisions in
order to furnish services in a fashion not otherwise
permitted under the Medicaid State Plan.
181
Chapter 7: Participant-Directed Services and Supports
Section 1115 Waivers
19
Before the enactment of the §1915(j) authority,
Federal law did not easily accommodate the
incorporation of the full range of participant
direction options into the delivery of personal
care services furnished through the Medicaid
State Plan. As a consequence, the §1115
authority had to be invoked when a state was
interested in implementing a wide-ranging
participant direction option (including budget
authority) for State Plan personal care services.
20
With the availability of the §1915(j) and other
authorities for implementing participant
direction options, states now have little or no
reason to invoke the §1115 waiver authority
solely to initiate a participant-directed services
option for Medicaid HCBS except in so far
as participant direction is a component of a
broader Medicaid reform proposal. As a general
matter, §1115 waivers may only be used to
test service delivery approaches that are not
otherwise feasible under Medicaid law.
Table 7-1 summarizes the key features of participant
direction programs under four of the ve principal
Medicaid authorities. The remainder of this section
describes the basic scope of each authority and
how it can be applied with respect to participant
direction.
1. State Plan Coverage of Personal Care
Under §1905(a)(24) of the Social Security Act, a state
has the option to cover personal care servi ces under
its Medicaid State Plan. (See Chapter 1 and Chapter
7 for more information about this authority.) Thirty-
two states cover personal care under their Medicaid
State Plans.
21
When personal care is covered under
the Medicaid State Plan, it must be provided to all
Medicaid participants who require such services.
Because Personal Care is an optional State Plan ben-
et, a state may impose limitations on the amount,
frequency, and duration of the services that it pro-
vides to eligible participants.
Participant Direction of Personal Care
In 1997, CMS issued revised guidance concerning
the provision of personal care under the
Medicaid State Plan.
22
In this guidance, CMS con-
rmed that states have the option to use a partici-
pant direction model, where “the Medicaid bene-
ciary may hire their own provider, train the provider
according to their personal preferences, supervise
and direct the provision of the personal care ser-
vices and, if necessary, re the provider.” States may
also permit family members or others specied in
the service plan to direct the provider on behalf of
the individual receiving the services.
Many states that cover personal care under the
Medicaid State Plan authorize participant-directed
services.
23
In some states (e.g., Maine and Massachu-
setts), third-party entities (often Independent Living
Centers) facilitate participant direction by perform-
ing payroll and related employment functions on
behalf of program participants (hereafter, called
participants) who select and manage their workers.
Elsewhere (e.g., California and Michigan), the state
itself or its claims payment contractor performs
payroll and tax-ling functions as the participant’s
employer-agent.
There are two main limitations concerning the
extent to which participant direction can be used
in conjunction with the delivery of personal care
under the Medicaid State Plan.
• When personal care is covered under §1905(a)
(24), the budget authority may not be
used and personal care dollars may not be
redirected or cashed out (i.e., converted to a
budget) to purchase other types of goods and
services. Medicaid dollars may only be used to
pay for the provision of personal care.
• Legally responsible relatives (i.e., parents of
minor children and spouses) may not be paid
to provide personal care. However, other
relatives (at a state’s option) can be paid to
provide personal care.
182 Understanding Medicaid Home and Community Services: A Primer
Table 7-1. Participant Direction Features of the Optional Medicaid Authorities
Features §1905(a)(24)
State Plan
Personal Care
Services
§1915(c)
Home and
Community-Based
Services Waiver
§1915(i)
State Plan Home
and Community-
Based Services
§1915(j)
Self-Directed
Personal
Assistance
Services
Employer Authority Allowed Allowed Allowed Required
Budget Authority Not allowed Allowed Allowed Required
Cash Payments to
Participants
Not allowed Not Allowed Not allowed Allowed
Direction by
Representative
Allowed Allowed Allowed Allowed
Hiring of Legally
Responsible
Individuals
Not allowed Allowed Allowed Allowed
Information &
Assistance
Not required Required Required Required
Financial
Management
Services
Fiscal employer
agent services only
are required
Required Required Required, except
for those receiving
the cash option
Limitation on services
that can be directed
Not applicable;
personal care is the
sole service
Allowed Allowed Not allowed
Availability of
Non-Traditional Goods
and Services
Not allowed Allowed Allowed Allowed
Comparability Cannot be waived Can be waived Can be waived Can be waived
Statewideness Cannot be waived Can be waived Cannot be waived Can be waived
Availability of Non-
Participant-Directed
Services
Not required Required Not Required
Required
24

183
Chapter 7: Participant-Directed Services and Supports
These limitations may be overcome when a state
elects to furnish participant-directed personal care
under provision §1915(j) of the Social Security Act
(described below).
2. HCBS Waiver Authority
Under the provisions of §1915(c) of the Social
Security Act, a state may obtain Federal waivers to
furnish home and community services to partici-
pants who require the level of care that is provided
in a Medicaid-reimbursable institutional setting but
choose to be supported in the community. All states
except Arizona and Vermont operate HCBS waiv-
ers.
25
(For more information about this authority, see
Chapter 1 and Chapter 4.)
Participant Direction of Waiver Services
Since the inception of the HCBS waiver program in
1981, some states allowed participants to exercise
the employer authority (e.g., Oregon, Wisconsin,
Washington). As previously noted,
in 2002 the CMS Independence Plus initiative
spelled out for the rst time the essential features
for incorporating participant direction into the
delivery of waiver services.
26
As part of the initiative,
CMS issued a stand-alone Independence Plus HCBS
waiver application template for states interested
in implementing participant direction of waiver
services
27
In 2004, CMS undertook a major revision of the
standard HCBS waiver application.
28
The revised ap-
plication, released in 2005 (and the most recent up-
date, released in 2008), requires states to describe in
detail the critical operational features of their HCBS
waivers and places a stronger emphasis on waiver
service quality assurance/quality management than
did the previous application.
29
In conjunction with
the release of the new application, CMS also re-
leased comprehensive technical guidance to states
concerning various dimensions of the design and
operation of HCBS waivers.
30
An important feature of the revised HCBS waiver ap-
plication is the inclusion of a distinct part (Appendix
E) that is devoted to participant direction of waiver
services.
31
Appendix E is designed to permit a state
to incorporate participant direction into the opera-
tion of any HCBS waiver.
When states elect to include a participant direction
option in an HCBS waiver, they have the latitude to
shape the option along several dimensions, includ-
ing
• Limited Implementation of Participant
Direction. A state may elect to oer the
participant direction option in all parts of the
state or limit it to specic areas or regions,
for example, to create a pilot in a specic
geographic area to evaluate the program
design before expanding it statewide.
• Availability of Participant Direction by
Types of Living Arrangement. A state may
decide to make its participant direction option
available to all waiver program participants
(hereafter called participants) or limit the
option to specied groups of participants,
such as persons who live with their families or
in their own homes
.32
• Direction by a Representative. A state
may allow services to be directed by a
representative selected by the participant.
• Limitation of Services That May Be
Participant Directed. A state may specify
which waiver services—some or all—may be
directed by participants.
• Election of Employer and/or Budget
Authority. A state may elect to oer
participants the employer authority or the
budget authority—or both—over the services
they may direct. In each instance, a state
may limit the extent of the authority that
participants may exercise.
• Employer Authority. A state has the option
to oer two models of the employer authority:
(1)“co-employer” model—also known as
the “agency with choice” model, where a
third party serves as the primary or legal

184 Understanding Medicaid Home and Community Services: A Primer
employer of workers that the participant
selects to furnish services and the individual
or representative serves as the secondary or
managing employer; and/or (2)a “common
law employer” model, where the participant
or his/her representative is the legal employer
of workers.
33
Regardless of the employer
authority model used, the state may not
permit payment to individuals who are
ineligible to participate as providers in the
Federal Medicaid program.
34
• Budget Authority. A state has the option to
allow participants to exercise decision-making
authority and management responsibility
for an individual budget to purchase goods
and services authorized in the service plan.
When a state oers budget authority, it may
specify whether participants are aorded the
exibility to shift funds among authorized
services within the total amount of the budget
without prior review and approval; desired
purchases that are not in the service plan,
however, must be formally added.
• Coverage of Individual Directed Goods
and Services. A state may elect to include
the coverage of non-traditional “individual
directed goods and services” in its waiver.
35
Under this service coverage, participants may
identify and purchase goods and services
from their individual budgets that are not
otherwise covered under the HCBS waiver
or the Medicaid State Plan; for example,
appliances that substitute for or reduce the
need for paid assistance, such as a microwave
oven. Coverage of non-traditional goods
and services is only an option for waiver
participants who exercise budget authority.
36
The criteria for allowable goods and services
is articulated in a State Medicaid Director
Letter.
37
As part of its design of an HCBS waiver participant
direction option, a state must also address the fol-
lowing topics:
• Information About Participant Direction.
A state must describe how it will inform
waiver participants about the benets,
responsibilities, and potential risks of directing
their services as compared to continuing
to receive services in the traditional service
system.
38
• Financial Management Services. A
state must provide for the provision of
nancial management services on behalf of
participants who direct their waiver services.
The HCBS waiver statute does not permit the
payment of Medicaid dollars directly to waiver
participants through the use of a “cash option.”
Thus, the use of an intermediary to perform
nancial transactions on behalf of participants
is required under the HCBS waiver authority.
States have the latitude to contract for
nancial management services as a Medicaid
administrative function or to oer them as a
waiver service.
39
• Information and Assistance to Support
Participant Direction. Similarly, a state
must make information and assistance
available to participants who direct their
services and wish to avail themselves of
such assistance. This assistance may take the
form of a distinct waiver service or it can be
covered as an administrative activity.
40
For
example, assistance might be provided to
help participants locate workers or to develop
the service plan. The type and extent of the
supports that must be available to participants
depends on the nature of the participant
direction opportunities provided under the
waiver.
• Budget Safeguards. A state must put
mechanisms in place to ag situations when
a waiver participant might overspend and
prematurely deplete the individual budget,
and intervene as appropriate. It is also
important that states monitor budgets to
identify under-spending, as this may be an
indication of inadequate service delivery.
• Transition. A state must allow waiver
participants who voluntarily decide to
discontinue participant direction to transition
to traditional models of service delivery,
which can include agency-delivered services.

185
Chapter 7: Participant-Directed Services and Supports
In particular, a state must ensure that such
participants continue to receive critical
services during the transition period.
• Termination from Participant Direction
Option. Finally, a state must describe the
circumstances under which it will terminate
participants’ use of the participant direction
option and provide for their transition to
traditional modes of service delivery. As with
vol untary transitions, a state must ensure
the participants continue to receive critical
services during the transition period.
States have considerable latitude in determining
how they will address these requirements.
Additional HCBS waiver operational dimensions re-
late to participant direction of waiver services. These
include service planning (and associated risk assess-
ment processes) and some elements of quality man-
agement. CMS does not require states to develop
processes concerning these generic dimensions
of waiver operations that are specically keyed to
participant direction. However, when a state oers
a participant-directed services option, CMS expects
that such processes will take into account any spe-
cial considerations related to participant direction.
For example, when participants assume the role
of employer and a professional service provider is
no longer overseeing service delivery, participants
themselves must assume the responsibility of man-
aging sta and assessing quality.
Some states have elected to deliver HCBS in tan-
dem with the provision of State Plan services by
operating a §1915(b)/§1915(c) concurrent waiver
program.
41
Such waivers use a managed care model
to coordinate the provision of services to Medicaid
participants. Participant direction may be incor-
porated into this type of waiver program.
42
(See
Chapter 8 for a discussion of Medicaid managed
care authorities.)
3. State Plan Coverage of HCBS
Section 6086 of the DRA-2005 added §1915(i) to the
Social Security Act, eective January 2007.
43
This
provision permits a state to oer HCBS under its
Medicaid State Plan without having to secure Fed-
eral approval of a waiver. Section 1915(i) was sub-
sequently amended by the Patient Protection and
Aordable Care Act of 2010 (hereafter called the
Aordable Care Act). The amendments only aect
one of the DRA-2005 provisions related to partici-
pant direction: states may now oer “other” services
(as they can in §1915(c) waivers), which means that
participants will have the exibility to purchase a
wide range of “goods and services” to reduce their
dependence, as long as they are included in the
service plan. CMS has not yet published a nal rule
for the §1915(i) authority.
Participant Direction of State Plan HCBS
The §1915(i) authority specically allows states to
incorporate a participant direction option for the
delivery of State Plan HCBS.
44
Under the statute,
participant-directed services are dened as HCBS
“which are planned and purchased under the direc-
tion and control of such individual or the individu-
al’s authorized representative.”
States that elect to incorporate a participant direc-
tion option in the provision of State Plan HCBS must
address the following:
• Assessment. The state must provide for a
process to assess the “needs, capabilities, and
preferences” of the individual.
• Service Plan. The state must have a person-
centered service plan development process
that is directed by the individual or the
individual’s authorized representative. The
pro cess must (1)build upon the individual’s
capacity to engage in activities that promote
community life; (2)respect the individual’s
preferences, choices, and abilities; and
(3)involve families, friends, and professionals
as desired or required by the individual
or his/her authorized representative. The
service plan must also include appropriate
risk management techniques that recognize
the roles and sharing of responsibilities in
obtaining services in a participant-directed
manner and ensure the appropriateness of
the service plan based on the resources and
capabilities of the individual or the individual’s
authorized representative.

186 Understanding Medicaid Home and Community Services: A Primer
• Limitation of Services That May Be
Participant Directed. A state must specify
which of the services it oers under its §1915(i)
benet may be directed by participants. The
service plan must specify the services that
participants or their representatives will self-
direct, the methods by which they will self-
direct, and the supports that are available to
the participant.
• Methods of Participant Direction. A state
must also specify the methods by which
participants may direct their services. States
may elect to oer participants the employer
and/or budget authority along similar lines as
allowed under the HCBS waiver authority.
• Participant-Directed Budget. States may
o er participants a participant-directed
budget that identies the dollar value of the
services and supports under the control and
direction of the individual or the individual’s
authorized representative. When a state oers
a participant-directed budget, it must specify
the methods by which the budget is calculated
and provide for a process to adjust the
budget based on changes in an individual’s
assessment and service plan.
45
• Financial Management Services. A state may
provide nancial management services as an
administrative activity to support participants
who elect to direct their services or contract
with an outside entity to provide these
services.
In most respects, the elements of a participant di-
rection option under §1915(i) closely parallel those
in HCBS waivers.
4. State Plan Coverage of Participant-
Directed Personal Assistance Services
Section 6087 of DRA-2005 added §1915(j) to the
Social Security Act, eective January 2007.
46
This
authority permits a state to institute a participant-
directed services option that includes the disburse-
ment of cash prospectively to participants who
direct their personal assistance services.
47
(While
specic statutes use dierent terms—personal care
and personal assistance—the service provided is
the same.) Absent the §1915(j) authority, partici-
pant direction of Medicaid State Plan personal care
services is limited to use of the employer authority,
as previously discussed.
The §1915(j) authority also allows states to permit
participants who direct their services under the
State Plan Personal Care benet to use individual
budgets to purchase non-traditional goods and
services other than personal care/assistance, to
the extent that expenditures would otherwise be
made for human assistance. (States already have
the authority under §1915(c) to allow HCBS waiver
participants to purchase a broad range of goods
and services.)
States may use the §1915(j) authority only in a State
Plan Personal Care program or in HCBS waiver pro-
grams already in operation (i.e., states may not oer
participant-directed services under the §1915(j)
authority except through an existing State Plan Per-
sonal Care program or an HCBS waiver program).
Especially with respect to Medicaid State Plan
personal care services, this authority is specically
intended to relieve states of the need to operate
§1115 waivers in order to oer participants wide-
ranging authority to direct their personal care ser-
vices, including using their personal care budget to
purchase other goods and services, as long as they
substitute for or reduce the need for paid personal
assistance.
In September 2007, CMS issued a State Medicaid
Director Letter that provides guidance to states con-
cerning this Medicaid State Plan option.
48
The letter
is accompanied by a Medicaid State Plan amend-
ment pre-print that states may submit in order to
invoke this authority.
49
The rule was nalized on
October 3, 2008.
50
So far, seven states—Alabama,
Oregon, Florida, Texas, New Jersey, California, and
Arkansas—have secured CMS approval of a State
Plan amendment under this authority, and several
other states have submitted their draft amend-
ments to CMS and requested technical assistance.

187
Chapter 7: Participant-Directed Services and Supports
Key Features of the §1915(j) Authority
The authority has the following major features:
• Disregard of Statewideness and
Comparability. A state may elect to make
its participant direction option available
statewide or in specied parts of the state, and
may limit the number of persons who direct
their services under this option.
• Limitations on Participants Who May Self-
Direct. The participant direction option may
only be oered to participants who live with
their families or in housing that they own or
lease, not to those whose living arrangement
is owned, operated, or controlled by a service
provider. States also have the latitude to
make participant direction available to all
participants (subject to the preceding limits)
or only to specied groups of participants.
• Election of Participant Direction. A state
must provide information and counseling
regarding participant direction to individuals
so they can make an informed choice about
whether to direct their services and supports.
A state also must allow participants to
voluntarily terminate participant direction and
return to receiving provider-managed services.
When a person voluntarily ends participant
direction (or the state determines that
participant direction should be terminated
involuntarily), the state must ensure that the
individual continues to receive critical services
during the transition period.
• Use of a Representative. A state may permit
the individual to appoint a representative
to direct services, but the person acting as a
representative is prohibited from providing
personal assistance services to that individual.
• Service Plan. The state must fashion a
person-centered service planning process
that includes an assessment of the individual’s
needs, strengths, and preferences and that
“…(a)builds upon the participant’s capacity to
engage in activities that promote community
life and that respects the participant’s
preferences, choices, and abilities; and (b)in-
volves families, friends, and professionals
in the planning or delivery of services or
supports as desired or required by the
participant.”
• Quality Assurance and Risk Management.
The state must develop appropriate quality
assurance methods and employ processes
that identify and address risks. The risk
management plan must be developed in
concert with the participant.
• Individual Budget. The state must provide
an individual budget to each participant who
elects to direct his/her services. The amount
of this budget must be determined through
the uniform application of a methodology
developed by the state.
• Cash Option. A state may elect to disburse
cash prospectively to self-directing
participants to directly purchase services.
Participants who elect this option are also
permitted to pay their workers and le the
employer share of payroll taxes, subject only to
retrospective oversight to ensure compliance
with labor and tax law requirements. There is
no comparable cash option available under
the State Plan Personal Care option, the HCBS
waiver program, or Medicaid State Plan HCBS
coverage.
51
• Purchase of Non-traditional Goods
and Services. A state may elect to permit
participants who self-direct to “to acquire
items that increase independence (such as a
microwave oven or an accessibility ramp) or
substitute for human assistance, to the extent
that expenditures would otherwise be made
for the human assistance.” In other words,
participants may be given the authority to use
their individual budgets to purchase goods
and services other than personal assistance, as
long as they substitute for or reduce the need
for paid personal assistance. On November 19,
2009, CMS issued a State Medicaid Director
Letter to provide guidance on this provision.
Among other clarications, the Letter stated
that “the services, supports, and items that
are purchased with a service budget must be

188 Understanding Medicaid Home and Community Services: A Primer
linked to an assessed participant need or goal
established in the service plan.”
52
• Availability of Ongoing Assistance in
Participant Direction. The state must
make ongoing training, assistance, and
counseling available to participants who
direct their personal assistants through the
use of a counselor and other information and
assistance methods.
• Providers. Under this authority, participants
can “choose as a paid service provider, any
individual capable of providing the assigned
tasks including legally liable relatives,” as long
as they meet applicable state requirements,
such as those related to training and criminal
background checks.
• Financial Management Services. A state
must arrange for the provision of nancial
management services on behalf of self-
directing participants (except those who have
elected the cash option, if available).
53
The
state may obtain such services from vendors or
elect to provide the services itself. The costs of
these services are eligible for Federal nancial
participation only as an administrative
expense. As noted above, under an HCBS
waiver, they can be reimbursed as either a
service or an administrative expense.
While this authority shares some of the features of
participant direction that are available under the
HCBS waiver and Medicaid State Plan HCBS options,
it goes beyond those options by permitting states
to oer an individual the option to receive some or
all of the benet directly in cash.
5. State Plan Community
First Choice Option
Section 2401 of the Aordable Care Act amends
§1915 of the Social Security Act by adding a new
subsection (k), eective October 2011, to allow
states to provide “Community-based Attendant Ser-
vices and Supports”—called the Community First
Choice Option.
Under this new benet, services and supports may
be provided through an agency-provider model
or “other” model, both of which require that par-
ticipants or their representatives select, manage,
and dismiss workers. An “other” model is dened as
methods, other than an agency-provider model, for
the provision of consumer-controlled services and
supports. Such models may include the provision
of vouchers, direct cash payments, or the use of a
scal agent to assist in obtaining services, as long
as the model allows for the services to be “selected,
managed, and dismissed by the individual, or, as
appropriate, with assistance from the individual’s
representative,” and to be “controlled, to the maxi-
mum extent possible, by the individual…regardless
of who may act as the employer of record.” Services
must be provided by qualied individuals, although
the law allows providers to be “family members,”
and gives the Secretary of HHS latitude to dene
the term.
Employers must adhere to the provisions of the Fair
Labor Standards Act of 1938 and applicable Federal
and state laws regarding income and payroll taxes,
unemployment and workers compensation insur-
ance, general liability insurance, and occupational
health and safety.
Key Participant Direction Features of the
§1915(k) Authority
The authority has the following major features:
• Use of a Representative. Participants may ap-
point a representative to direct services.
• Service Plan. The state must fashion a person-
centered service planning process based on a
functional needs assessment.
• Purchase of Non-Traditional Goods and
Services. In addition to assistance with
Activities of Daily Living and Instrumental
Activities of Daily Living, permissible services
may include… “the use of beepers or other
electronic devices” and “voluntary training
on how to select, manage, and dismiss
attendants.” Expenditures for transition costs
involved in moving from an institution to
the community, including deposits for the
rst month’s payment for rent and utilities,
189
Chapter 7: Participant-Directed Services and Supports
bedding, basic kitchen supplies, and other
necessities, can also be funded through
this authority. The authority also allows
“expenditures relating to a need identied
in an individual’s person-centered plan of
services that increase independence or
substitute for human assistance, to the extent
that expenditures would otherwise be made
for the human assistance.”
Service Planning and Authorization
Participant direction service models use the needs
assessment and service planning processes as fun-
damental activities to safeguard participants’ health
and welfare, and to ensure that the services and
supports provided enable participants to meet their
individual community living goals. The participant
direction model diers from professional-directed
service models by arming that the participant
is the center of—and leads—the service planning
process. Person-centered planning (PCP) is a critical
component of participant-directed service plan-
ning, which enables and helps the individual to
identify and access a personalized mix of paid and
non-paid services and supports. While PCP methods
used to be associated only with service planning
for persons with developmental disabilities, these
methods are now employed for individuals with any
type of disability, and CMS encourages and sup-
ports the use of person/family-centered planning
methods in service plan development.
With the exception of home health services, Medic-
aid policy does not dictate that service plans must
be prepared by medical, clinical, or case manage-
ment professionals. Whether for waiver services
authorized in a plan of care or personal care services
under the optional State Plan benet, states have
considerable latitude with regard to empower-
ing the individual to manage authorized services.
Under the Personal Care option, for example, many
states already allow participants to determine when
authorized service hours are to be furnished and to
alter the schedule to meet their needs.
In an HCBS waiver program, states may also per mit
participants to manage the service schedule or alter
the mix of authorized services to meet their chang-
ing needs without having to develop an entirely
new service plan. However, the statutory require-
ment that “services be provided pursuant to a writ-
ten plan of care” must continue to be met.
Federal law requires that the services individuals
receive through an HCBS waiver program be pro-
vided pursuant to a plan of care.
54
Neither Federal
law nor regulations specify the process by which
this plan of care is to be developed. The plan of
care must meet the requirements spelled out in the
State Medicaid Manual and the Technical Guide for
HCBS waivers, as well as requirements included in
the state’s approved HCBS waiver request. Eective
service plan development processes are essential to
ensure that waiver participants will receive the ser-
vices and supports they need and want in order to
successfully live and thrive in the community. States
must specify in their waiver application how the
participant-centered plan will be developed as well
as how the state will monitor the service planning
process to ensure that it is person centered.
At one time, Federal regulations dictated that the
§1905(a) optional State Plan Personal Care benet
be authorized by a physician and supervised by
nursing personnel. In the Omnibus Reconciliation
Act of 1993, states were specically authorized
to use alternative service authorization methods,
including those that do not require the involvement
of medical personnel. This policy change enables
states to adopt alternative approaches to personal
care service planning. A common approach is to
delegate this task to case managers who are re-
sponsible for assessing eligibility and authorizing
services.
55
Section 1915(i) highlights service planning as a
fundamental component of participant direction,
intended to both safeguard health and welfare, as
well as ensure meaningful involvement of partici-
pants in identifying and selecting the services and
supports they need. Section 1915(j)(5)(B) emphasiz-
es the assessment and service planning process by
requiring an assessment of the participant’s “needs,
strengths, and preferences” for personal assistance
services.

190 Understanding Medicaid Home and Community Services: A Primer
Use of Representatives
All individuals, regardless of their impairments, can
be successful in directing their services with the
proper supports. People with serious illnesses and
those with cognitive impairment—including im-
pairment due to dementia, stroke, traumatic brain
injury, and developmental disabilities—are capable
of expressing preferences, but may need assistance
to manage their services and budget. Most par-
ticipant direction programs permit participants to
designate a representative to assist them in these
tasks. Representatives can ensure that participants’
preferences are known and respected and can man-
age tasks that participants would perform if they
were able.
Some programs allow participants to use represen-
tatives without formally designating them as such,
but have criteria that individuals must meet to be
a representative, such as demonstrating a strong
commitment to the participant’s well-being and
being interested in and able to carry out program
responsibilities and requirements.
56
Although for-
mal designation requires individuals to complete a
form acknowledging acceptance of the duties and
responsibilities of a representative, there is no legal
transfer of authority or responsibility with respect
to personal decision making or nancial matters
from the participant to the representative (as would
be the case if an individual were to grant power-of-
attorney or a court were to appoint a guardian.)
Program requirements for person-centered plan-
ning also apply to representatives, who must
re-present the best interests of participants and
ascertain and act in accordance with their prefer-
ences—unless they are impractical.
57
The use of a representative under the §1915(j)
authority is at the option of the state. This author-
ity provides that representatives include “(1)a
minor child’s parent or guardian; (2)an individual
recognized under state law to act on behalf of an
incapacitated adult; (3)a state-mandated represen-
tative, after approval by CMS of the state criteria, if
the participant has demonstrated, after additional
counseling, information, training, or assistance, the
inability to self-direct personal assistance services.”
58
The statutory language of §1915(i) gives states the
option to allow an individual or the individual’s rep-
resentative to elect to receive self-directed HCBS.
59
An issue intrinsic to the use of representatives is
avoiding a conict of interest. Most programs that
allow representatives generally do not permit them
to be paid either as workers or for serving as repre-
sentatives. However, exceptions can be made under
extraordinary circumstances (e.g., lack of work-
ers in isolated areas or the inability of workers to
understand individuals with speech impairments).
The nal rule for §1915(j) stipulates that a person
acting as a representative for a participant directing
their personal assistance services is prohibited from
acting as a provider of such services.
60
The HCBS
waiver application (version 3.5) instructions provide
guidance on the use of representatives. (See the
Resources section of this chapter for a link to the
application.)
Individualized Backup Plans
A key component of person-centered service plan-
ning is a risk assessment process to identify issues
or situations that can jeopardize health and welfare
and to develop an individualized backup plan that
species actions to prevent them or address them
if they occur. For example, a backup plan should
designate individuals to be called—and in which
order—if workers do not arrive when scheduled.
Backup plans should also address methods for han-
dling any critical incidents that may occur, such as a
serious injury, abuse, neglect, or exploitation.
Every participant receiving home and community
services—whether through the traditional agency-
delivered service system or a participant direction
program—should be educated about the avail-
ability of backup resources and have a backup plan
individually tailored to their needs and preferences.
Appendix D-1(e) of the HCBS waiver application
(version 3.5) requires states to specify how poten-
tial risks to participants will be assessed during the
development of the service plan and how strategies
to mitigate risk will be incorporated into the service
plan, subject to participants’ needs and preferences.
In addition, states must describe how the service

191
Chapter 7: Participant-Directed Services and Supports
plan development process will address the need for
backup plans and the arrangements that are used
for backup must be included. These requirements
apply to both traditional and participant direction
programs.
Section 1915(j) regulations also emphasize the
importance of developing backup plans. Identify-
ing actual and potential risks—and determining
how they will be handled—should be accomplished
through discussion and negotiation among persons
involved in the service planning process.
If the backup plan includes calling individuals who
are willing and able to work at short notice, such
as neighbors, all of their payroll paperwork must
be on le in advance. Similarly, if it includes call-
ing a traditional service agency, the agency should
be informed that they are listed on a participant’s
backup plan and should be provided with informa-
tion about the participant’s needs.
Typically, backup plans include the names and
contact information of individuals or entities to be
called in a specic order; for example, family and
friends may be called rst, and a counselor or case
manager called only if family and friends are unable
to provide backup. Some states have developed
an Emergency Backup Person Designation Form to
identify individuals as emergency backup person-
nel; individuals designated are required to sign
the form demonstrating their willingness to serve
in this capacity. The eectiveness of backup plans
should be tested periodically and changes made as
needed.
Building Flexibility into the Service Plan
While Ensuring Equitable Budgets
In programs that allow participants to exercise bud-
get authority, purchases must be clearly linked to an
assessed need that is identied in the service plan.
61
Typically, purchases either increase independence
or address a personal care need. While some pro-
grams only allow participants to purchase personal
care services, others allow them to purchase a range
of services, including skilled nursing, rehabilitative
therapies, and supported employment services.
The exibility aorded to participants to purchase
goods and services varies by program. Programs
may require pre-approval of non-traditional servic-
es, such as purchase and maintenance of a service
dog, or they may develop a list of allowable items
and a prior authorization process to approve the
purchase of items not on the list. Other programs
allow participants signicant exibility and consider
any purchase that fosters community inclusion as
allowable.
States also can build exibility into the service
menu and individual service plans by combining
certain services (e.g., personal care, homemaker, re-
spite, non-medical transportation, and compan ion
services) into one service category in the waiver ap-
plication. This could allow participants to use their
budgets to purchase the specic services they need
to address their needs without having to formally
alter the service plan.
Programs that allow participants broad discretion
to purchase goods and services—within Federal pa-
rameters—must ensure that nancial accountability
is maintained through the application of consistent
methods to determine both needs and allowable
purchases to meet those needs. States must dem-
onstrate to CMS that statewide procedures are in
place to assess need and ensure access to services,
even in states where counties or local entities play a
strong role in the operation of the waiver.
Uniform use of a standardized assessment pro-
cess—and training to ensure its consistent use—
will enable states to ensure equitable funding of
individual budgets and help them to determine
whether budgets are being calculated accurately
using a consistent method. It is also important that
states implement procedures to ensure that funds
go to enrolled or otherwise eligible providers.
The methods states use to perform the assessment
vary greatly and often dier within a state according
to the population being served. In programs serv-
ing persons with developmental disabilities, many
states use standardized assessment processes and
instruments that are nationally tested and accred-
ited, such as the Supports Intensity Scale. In pro-
grams serving elderly persons and younger adults
with physical disabilities, assessment instruments

192 Understanding Medicaid Home and Community Services: A Primer
are generally state specic, but typically assess
ADLs and IADLs, as well as nursing needs, cognitive
impairment, and behavioral issues.
62
A few states use the comprehensive Minimum Data
Set–Home Care assessment instrument, which as-
sesses multiple factors that determine the need for
services, including cognition; vision; hearing and
communication; mood/behavior; social function-
ing; informal support services; physical functioning
(including IADLs and ADLs); continence; medical
conditions and medications; and the living environ-
ment.
63
Employing Family Members
All of the participant direction Medicaid authori-
ties allow participants to hire friends and relatives
to provide personal care services. States also have
the option under the HCBS waiver authority, and
§1915(i) and §1915(j), to allow participants to hire
legally responsible relatives (i.e., spouses, and
parents and legal guardians of minor children)
within certain parameters.
64
Generally, to be a paid
personal care provider, a legally responsible relative
has to be providing services that a spouse or parent
would not be providing for a non-disabled spouse
or minor child; for example, feeding a 15-year-old
child or bathing a spouse. Medicaid prohibits the
hiring of legally responsible relatives in participant
direction programs under the Medicaid State Plan
Personal Care benet.
Non-Personal Care Services
Relatives—including legally responsible relatives—
may be hired to provide non-personal care services
when they are dicult to obtain from other sources.
The rules that pertain to paying relatives to provide
non-personal care services are not substantially
dierent from the rules for obtaining such services
from other sources. The relative must meet what-
ever provider qualications the state may have
established and charge no more than any other
provider. For example, if a minor child has extensive
medical needs and requires skilled nursing services,
a parent who is a licensed nurse could provide the
service as long as she or he meets the state’s pro-
vider qualications.
Within the broad parameters of Federal policy, it is
up to states to dene the particular circumstances
under which relatives will be paid to furnish services
to participants. States can take various factors into
account, including the availability of other sources
for the same services, costs of family member ser-
vices versus costs of purchasing such services from
conventional sources, and specic circumstances
with respect to participants. See Box for Minnesota’s
provisions regarding payment of family members.
Minnesota’s Family Payment Policies
65
Minnesota does not allow legally responsible
relatives (i.e., spouses or parents of minor
children) to be reimbursed for personal care,
which they are legally obligated to provide to a
spouse or child.
Additional provisions are available under
the consumer-directed community supports
waiver service to allow spouses and parents of
minor children to provide “personal support
services”—within state-set limits in hours, rate
of pay, and scope of tasks.
The State allows services provided by other
relatives or friends to be reimbursed only if:
(1) they meet the qualications for providers
of care,
(2) the State has strict controls to ensure that
payment is made to the relative or friend
as providers only in return for specic
services rendered, and
(3) adequate justication exists for the
relative or friend to provide the service
(e.g., lack of qualied providers in remote
areas). Medicaid payment may be made
to qualied parents of minor children
or to spouses for extraordinary services
requiring specialized nursing skills that
they are not legally obligated to provide.
193
Chapter 7: Participant-Directed Services and Supports
Furnishing Assistance to
Individuals in Managing and
Directing Services
Participants who are interested in directing their
services may need or want assistance to do so. The
§1915(c) HCBS waiver authority and the §1915(j)
State Plan authority require states to furnish two
support services to participants directing their
services: (1)information and assistance, and (2)-
nancial management services. (The proposed rule
for §1915(i) also addresses the provision of these
two support services. However, it is not included
here because at the time of publication, it had not
yet been nalized.)
These support services are necessary to ensure
that individuals have a support system to ensure
they are able to manage their services and bud-
gets. The extent to which such supports are utilized
depends on the capacity, preferences, and needs of
each individual and may vary in scope and timing.
While their main purpose is to facilitate participant
direction, these supports also provide important
protections and safeguards for those directing their
own services. Financial management services also
provide scal accountability for state budget sta,
by helping participants to manage the individual
budget and by issuing payments on behalf of the
state.
Information and Assistance
Many terms are used to describe the provision of
information and assistance, including counseling,
supports brokerage, service coordination, and ser-
vice consultation. This Primer uses the term counsel-
ing. States have broad exibility to design counsel-
ing services in a manner that suits their program,
as long as they meet the intent of the service: to
provide detailed information to enable individuals
to make informed decisions about whether partici-
pant direction is right for them, and if it is, to assist
them in obtaining and managing their services.
CMS views the roles and responsibilities of the
counselor as fundamentally dierent from those of
a case manager. See Table 7-2 for a comparison of
services provided by counselors and traditional case
managers.
The case manager’s role to oversee and monitor ser-
vice delivery is often required to ensure that Medic-
aid or other public programs meet state and Federal
health and welfare requirements, and the case man-
agement system is often a key component of states’
quality management systems. Consequently, many
programs use both case managers and counselors
to assist participants, and in such cases it is essential
that they understand each other’s respective roles
and responsibilities, work collaboratively, and avoid
duplication of services. Participants also need to
understand the dierence between the two roles.
Some programs have one person perform the
responsibilities of both roles—either transferring
case management functions to counselors, or
having case managers assume the counselor role.
Whichever approach a state uses, the individuals
providing these services—whether counseling, case
management, or both—need to meet all applicable
job requirements. Prior to approval of a participant
direction waiver program, Federal reviewers will ask,
at a minimum, the following questions:
1. Does the program provide participants with
information about (a)its benets, (b)their
responsibilities under the program, and
(c)their liability if employment-related taxes
and workman’s compensation insurance
premiums are not paid?
2. Who provides the above information and what
is the process for providing it?
3. Who oversees the provision of information and
assistance?
4. Is the information provided in a timely manner
to permit informed decision making?
5. If both counselors and traditional case
managers are involved, how will their
functions be coordinated and how does the
program prevent duplication of services?
194 Understanding Medicaid Home and Community Services: A Primer
Table 7-2. Examples of Typical Activities of Counselors and Traditional Case Managers
Counselors Traditional Case Managers
Provide information about
• the person-centered planning process
• participants’ rights
• resources, choices, and options
• responsibilities, risks and/or liabilities associated
with participant direction and decision making
• program limitations or restrictions
• how to report changes in condition and needs
• recognizing and reporting critical events, abuse,
or neglect
• the availability of criminal background checks
and processes for conducting reference checks
Provide assistance with
• dening needs, preferences, and goals
• developing and managing the individual budget
• developing a backup plan
• identifying and obtaining services, supports, and
resources
• recruiting, hiring, and managing workers
• obtaining training in practical skills related to
personnel management (e.g., negotiating rates,
arranging schedules, training workers, and
making changes)
• assessing the quality of services received
• Explain the program process, and eligibility
criteria
• Present information about various settings
for service delivery: institutional, home, or
community-based; and service options:
traditional agency or participant direction
• Conduct an assessment to determine
eligibility for services and to develop
a service plan, and match needs with
resources
• Implement the service plan
• Monitor the provision of services
• Assess the quality of services
• Ensure cost/budget neutrality, if required
• Revise the service plan when changes
occur
• Perform periodic assessments and
eligibility determinations

195
Chapter 7: Participant-Directed Services and Supports
For detailed information about counseling services,
see the Resources section of this chapter for a link
to the chapter on Counseling in the Self-Direction
Handbook.
Financial Management Services
66
CMS denes Financial Management Services (FMS)
as follows:
Service/function that assists the family
or participant to (a)manage and direct
the distribution of funds contained in the
participant-directed budget; (b)facilitate the
employment of sta by the family or participant
by performing as the participant’s agent such
employer responsibilities as processing payroll,
withholding and ling Federal, state, and local
taxes, and making tax payments to appropriate
tax authorities; and (c)performing scal
accounting and making expenditure reports
to the participant and/or family and state
authorities.
67
The provision of nancial management services is
essential when implementing participant direction
programs for several reasons.
• Under the §1905(a) State Plan Personal Care
benet, the HCBS waiver authority, and the
§1915(i) authority, payments for services can
not be made directly to participants, either
to reimburse them for expenses incurred
or to enable them to directly pay a service
provider. Rather, payments on the participant’s
behalf must be made by an intermediary
organization (i.e., either a qualied Medicaid
provider or an entity under administrative
contract with the state).
68
• Under the §1915(j) authority, CMS does not
require states to mandate the use of nancial
management services for participants
who elect the “cash” option. Instead,
these participants may choose to retain
responsibility for some or all of their scal and
employer-related responsibilities. However,
even if participants choose to receive some
benets in cash and distribute workers’ payroll
checks directly, they may still choose to have
an FMS organization manage the Federal and
state tax lings and deposits and generate
payroll checks for their workers.
69
• Some FMS organizations may act as a neutral
bank for receiving and disbursing public funds
(i.e., Fiscal/Employer Agents)
.70
• Financial management services provide scal
accountability for state and local government
agencies, and safeguards for individuals
enrolled in participant direction programs
and their workers, by ensuring that payroll,
71
workers’ compensation insurance policy
management, and vendor payment tasks are
performed accurately and in accordance with
Federal, state, and local rules and regulations,
and in a timely manner.
• Some FMS organizations (i.e., Fiscal/Em ployer
Agents) assist program sta and participants
by providing a variety of nancial reports
related to the receipt of public funds, service
use, and payments. These reports inform
participants about their service use and
related expenditures and also act as a scal
and/or fraud monitoring tool for them and for
program sta.
• At the request of participants who are acting
as their workers’ managing employer, an FMS
provider who has a joint/co-employment
arrangement with participants (as in the
Agency with Choice or Public Authority/
Workforce Council models) can also provide
worker-related services (e.g., recruitment,
training, and supervision, and the provision of
emergency backup sta).
72
FMS Models
States principally use two FMS models to imple-
ment Medicaid and state-funded participant direc-
tion programs: the Fiscal/Employer Agent (F/EA)
model and the Agency with Choice model. The F/EA
model includes two specic types: Government F/
EA and Vendor F/EA. All of these models are de-
scribed below.

196 Understanding Medicaid Home and Community Services: A Primer
1. Fiscal/Employer Agent Model
Fiscal/Employer Agents are most eective for imple-
menting participant direction programs, particularly
those that allow participants to have individual
budgets, for several reasons. First, using an F/EA
provides participants a high degree of choice and
control over their workers as their common law
employers, while reducing their employer-related
burden by managing the payroll and bill payment
tasks. Second, using an F/EA provides safeguards
for participants by ensuring that all required taxes
are paid and all Department of Labor and workers’
compensation insurance requirements are met.
Third, using an F/EA can provide scal account-
ability for states. Both the Government and Vendor
F/EA models operate under §3504 of the Internal
Revenue Service (IRS) code.
73
Government Fiscal/Employer Agents. When
states implement participant direction programs
using a Government F/EA, the costs associated with
providing nancial management services must be
billed as an administrative expense for the pur-
pose of claiming Federal Medicaid matching funds
because participants’ freedom of choice of provider
is limited.
74
Thus, when evaluating the feasibility of
implementing a Government F/EA, a state’s Med-
icaid agency and program sta should assess the
economic impact of using this model on the receipt
of Federal Medicaid matching funds and the admin-
istrative costs to the state associated with monitor-
ing multiple F/EA providers.
Vendor Fiscal/Employer Agents. When states
implement participant direction programs using a
Vendor F/EA, states may engage vendor entities–ei-
ther under contract or as qualied Medicaid service
providers, or both—who have the knowledge,
experience, resources, and the infrastructure neces-
sary to provide eective scal services. This model
enables states to negotiate cost-eective fees for F/
EA services rendered, rather than providing these
services in-house. States also have the option to
(1)select a discrete number of Vendor F/EAs, using a
competitive solicitation process, and bill F/EA costs
as an administrative expense (at a uniform Federal
matching funds rate of 50 percent); or (2)develop
Medicaid F/EA provider standards and provide
freedom of choice of provider to participants, and
bill F/EA costs as a service expense for the purpose
of claiming Federal matching funds (at a Federal
matching funds rate that ranges from 50 to 83 per-
cent).
75
For Vendor F/EA services to be reimbursed as a
waiver service, states must meet a number of Fed-
eral requirements. States must develop a service
denition that includes a set of provider qualica-
tions and the tasks that will be performed by the
Vendor F/EA and any reporting agent. States must
verify a provider’s qualications before services are
initiated, and must provide a detailed description
of the frequency and methods by which provider
qualications will be re-veried and ongoing perfor-
mance will be monitored.
States must treat Vendor F/EAs as they would any
Medicaid service provider. States may not arbi-
trarily limit the number of Vendor F/EAs available
to participants as this would restrict their freedom
of choice of provider and disqualify the state from
claiming Vendor F/EA expenses as a waiver service
for Federal matching funds purposes. Finally, states
must monitor Vendor F/EAs and any reporting
agents’ performance on an ongoing basis.
A signicant number of states limit the number
of Vendor F/EA providers and forgo the receipt
of Federal service matching funds, called Federal
Medical Assistance Percentage (FMAP), in order to
obtain the cost eciencies from working with and
monitoring fewer F/EA providers.
76
The majority use
some type of competitive solicitation process to
select one or more Vendor F/EA providers.
However, some states report challenges related
to this strategy, such as (1)the need to write an
eective solicitation document that accurately and
completely reects F/EA requirements; (2)the need
to evaluate F/EA knowledge and experience for
proposal review and vendor selection purposes;
(3)interruptions in the continuity of F/EA provid-
ers because a satisfactory F/EA provider must rebid
at the end of each contract period and may not be
reselected (e.g., if they are not the lowest bidder,
which may be a priority for a state’s purchase and
property department responsible for managing the
solicitation process); (4)the resources and time re-
quired to complete a solicitation, including address-

197
Chapter 7: Participant-Directed Services and Supports
ing any bidder challenges; and (5)developing and
executing eective performance-based contracts.
Other states provide freedom of choice of F/EA
service providers for participants in order to receive
Federal service matching funds.
77
Again, some of
these states have experienced challenges, such
as (1)having sucient knowledge of Federal and
state F/EA requirements and operations to prepare
Medicaid standards and execute Medicaid provider
agreements eectively; (2)preparing eective pro-
tocols for certifying F/EA providers as Medicaid pro-
viders and monitoring their performance through
periodic re-certication; (3)having the sta and -
nancial resources necessary to conduct F/EA certi-
cations and recertication/performance monitoring
in a timely and eective manner; and (4)having the
cost of monitoring F/EA performance exceed the
additional amount a state may receive in Medicaid
service match versus administrative match. Given
this last challenge, states should determine how
much it will cost them to monitor the performance of
signicant numbers of F/EAs, as this amount may well
exceed the funds they would receive through FMAP.
Establishing Reimbursement for F/EA Servi ces.
States need to establish reasonable and adequate
reimbursement for Vendor F/EA services (and Gov-
ernment F/EA services that are subcontracted to a
subagent or reporting agent) that reect the costs
of providing these services. CMS has approved a
variety of methods for determining reimbursement
for nancial management services, including the
basic transaction-based reimbursement method
and the modied transaction-based (per member
per month or per member per day) reimbursement
method. A method that is not approved by CMS
is the percent of budget reimbursement method,
which reimburses on the basis of a percentage
of the total dollar volume of services that an FMS
entity processes. This approach is not approved be-
cause it does not reect the actual cost of providing
the F/EA service. 78
For a detailed description of the various F/EA mod-
els and their advantages and challenges, see the
Resources section of this chapter for a link to the
chapter on Fiscal/Employer Agent Services in the
Self-Direction Handbook.
2. Agency with Choice Model
In contrast to the F/EA models described above, the
Agency with Choice FMS model operates under a
co-employment arrangement whereby employer
status is shared by the participant and an agency.
For IRS purposes and other considerations, the
agency is the primary or legal employer and o-
cially hires the worker(s), processes human resource
forms, and manages the payroll tasks. They also
monitor the participant’s health and welfare, en-
sure that intended services are provided, and may
provide guidance on recruiting, training, managing,
and discharging workers. The participant or his/
her representative is the secondary or managing
employer. In this role, the participant or representa-
tive recruits, interviews, and selects workers, and
then refers them to an agency for the completion
of employment/payroll paperwork. In addition, the
participant or representative trains, manages, and
discharges workers (to the extent they wish to).
To be considered a bona de participant direction
model, agencies operating under this model must
give participants meaningful choice and control
over their workers—the authority to select, train,
manage, and dismiss, as well as directing the tasks
they perform. Key elements of an eective Agency
with Choice program include (1)a strong commit-
ment to the philosophy of participant direction;
(2)a high level of choice and control aorded
participants and their representatives; and (3)com-
prehensive support services, such as employer-re-
lated skills training that covers worker recruitment,
selection, management, evaluation, and discharge;
assistance with recruiting, hiring, and discharging
workers when requested; and guidance on conduct-
ing criminal background checks, if not required by a
participant-directed services program.
Each of the ve Medicaid participant direction
authorities acknowledge the Agency with Choice
model as an option for participant direction pro-
grams and it may be used to fulll FMS responsibili-
ties for participants exercising employer authority,
budget authority, or both. CMS provides some
basic information on Agency with Choice models in
the Waiver Application Instructions and Technical
Guidance.
79
Some states have established specic

198 Understanding Medicaid Home and Community Services: A Primer
requirements for this model (e.g., New Hampshire
and Pennsylvania).
In 2003, New Hampshire implemented regulations
for “Other Qualied Agencies” that outline the re-
quirements for entities to be certied as such in the
State.
80
This is the name the State uses for Agency
with Choice FMS providers that furnish nancial
management services to participants in the State’s
Choices for Independence HCBS waiver who are
directing their personal care services. Eective July
1, 2008, Pennsylvania published an Oce of Devel-
opmental Programs Administrative Bulletin entitled,
Agency with Choice Financial Management Services.
Among other things, the Bulletin outlines the re-
quirements for agencies to operate as Agency with
Choice FMS providers for individuals enrolled in the
State’s Medicaid Consolidated and Person/Family-
Directed Supports waivers.
Consumer Choice and Provider Qualications
Section 1902(a)(23) of the Social Security Act
requires that Medicaid enrollees must be free to
choose among all willing and qualied providers.
This statutory requirement applies to all Medicaid-
funded services, including services furnished
through HCBS waiver programs. The Act allows the
Secretary of HHS to grant states a waiver of free-
dom of choice only in certain circumstances, and
then only when other safeguards are in eect that
preserve consumer choice.
Free choice of providers is absolutely necessary for
individuals to direct their own services and supports
(with the exception of FMS providers and counsel-
ors).
81
However, the Medicaid freedom of choice
statutory requirement extends only to “qualied”
providers, and therein lies the source of limitations
and/or complications when seeking to implement
participant direction programs. Federal Medicaid
law (whether under the Medicaid State Plan or
through an HCBS waiver program) requires that a
state establish required provider qualications and
agree to enroll all willing providers who meet such
qualications.
These qualications must be reasonable (i.e., they
must relate to provision of the service), and they
also must comport with state law. Within these
stipulations, states have considerable latitude in
establishing the qualications required of provid-
ers of home and community services. The broader
these requirements, the greater will be the number
of people who will qualify to provide services. Some
states, however, limit provision of personal care
services to entities that are licensed as “home care”
or “home health agencies” or have been licensed to
furnish community developmental disability servic-
es. This means, in turn, that individuals who provide
home and community services and supports must
be employees of such provider organizations. When
provider qualications are expressed in this fashion,
they can pose barriers to promoting participant-
directed servi ces.
Some of these barriers arise from state Nurse Prac-
tice Acts provisions, which sometimes dictate that
even non-health care related personal assistance
be provided under the supervision of a nurse (and,
not atypically, nurses who themselves must be
employees of a licensed home care or home health
agency). Thus, a central task for states interested in
promoting participant-directed services is a thor-
ough assessment of their provider qualications to
determine whether they need to broaden the types
of organizations and individuals who may qualify as
providers.
It is not necessary to limit providers to traditional
service agencies. Provider qualications may be
expressed solely with respect to the competencies
and skills individual workers must possess. Many
types of Medicaid home and community services
may be furnished by friends, neighbors, and fam-
ily members—including spouses and parents of
minor children under some authorities, at the state’s
option. In various states, families are encouraged to
seek out individuals in their communities who can
provide some types of services and supports for
people with developmental disabilities.
Revising provider qualications can be vital not only
in promoting participant-directed services but also
in expanding the potential sources of services and
supports for people with disabilities more generally.
However, no providers on the Oce of the Inspec-
tor General excluded provider lists may furnish
Medicaid services, whether directed by participants
or provided by agencies.

199
Chapter 7: Participant-Directed Services and Supports
Performance of Skilled Nursing Tasks
Although the principles underlying participant
direction support a social rather than a medical
service model, avoiding the medical model can be
complicated by state laws and regulations con-
cerning the performance of “skilled nursing tasks.”
Federal Medicaid policy does not dictate who must
perform skilled nursing tasks, merely that such tasks
be performed in compliance with applicable state
laws. But state laws and regulations often dictate
that such tasks be performed by or closely super-
vised by a licensed nurse—thereby creating obsta-
cles to participant direction service models. Liability
concerns—particularly when participants have ex-
tensive medical and nursing needs—can also stand
in the way of promoting participant direction.
To avoid duplicating Home Health benets already
available through Medicare or under the Medicaid
State Plan, many HCBS waiver programs do not oer
skilled nursing or rehabilitative therapies. However,
“skilled” paraprofessional services may still be pro-
vided by personal care workers under HCBS waivers
or under the State Plan Personal Care benet—as
long as the services are provided in conformity with
the state’s Nurse Practice Act. A 1999 CMS State
Medicaid Manual transmittal specically states that
Services such as those delegated by nurses or
physicians to personal care attendants may be
provided so long as the delegation is in keeping
with state law or regulation and the services
t within the personal care services benet
covered under a state’s plan. Services such as
assistance with medications would be allowed
if they are permissible in states’ Nurse Practice
Acts, although states need to ensure that the
personal care assistant is properly trained to
provide medication administration and/or
management
.82
This policy and its applicability to State Plan Person-
al Care programs and HCBS waiver programs were
rearmed in a July 2000 State Medicaid Director
Letter.
83
Most states restrict performance of medical or
skilled nursing tasks to licensed medical profession-
als, although most physician and nurse licensing
laws do permit individuals to be trained to perform
these tasks for themselves or for close family mem-
bers. Federal Medicaid law references state licens-
ing laws by requiring that Medicaid State Plans
comply with all “applicable” state and local statutes.
Under the Nurse Practice Acts in most states, tasks
that require nursing judgment—such as medica-
tion administration—and tasks considered to be
invasive procedures—such as catheterization and
injections—may be performed only by paid person-
nel who are registered nurses or persons supervised
by registered nurses.
Issues related to the performance of skilled nursing
tasks stem from concerns about quality assurance
and liability. (See the Appendix for an overview of
CMS requirements for quality management and
improvement systems.)
See the Resources section of this chapter for a link
to the chapter on Self-Direction and Health Care
in Developing and Implementing Self-Direction
Programs and Policies: A Handbook, which includes
a detailed discussion of liability issues related to
the performance and delegation of skilled nurs-
ing tasks, and ways in which states have addressed
them.
200 Understanding Medicaid Home and Community Services: A Primer
Resources
Since the Primer was rst published in 2000, numerous reports and other resources have become available
on the Internet. This section includes key resources relevant to participant direction. Most of the publica-
tions cite additional resources and the websites also have links to other sources of information.
Publications
Crisp, S., Doty, P., Flanagan, S., Smith, G., O’Keee, J., et al. (2009). Developing and Implementing Self-Di-
rection Programs and Policies: A Handbook. Chestnut Hill, MA: National Resource Center for Participant-
Directed Services.
This publication was developed to provide state sta, policymakers, service providers, program participants,
and other stakeholders with a single comprehensive source of information about participant direction pro-
grams and policies.
Available as the full handbook at http://www.cashandcounseling.org/resources/handbook
Available as individual chapters using the following links:
Chapter 1: Self-Direction
http://www.cashandcounseling.org/resources/pdf/cc-01.pdf
Chapter 2: Legal Authority
http://www.cashandcounseling.org/resources/pdf/cc-02.pdf
Chapter 3: Involving Participants
http://www.cashandcounseling.org/resources/pdf/cc-03.pdf
Chapter 4: Enrollment
http://www.cashandcounseling.org/resources/pdf/cc-04.pdf
Chapter 5: Individual Budgeting
http://www.cashandcounseling.org/resources/pdf/cc-05.pdf
Chapter 6: Counseling
http://www.cashandcounseling.org/resources/pdf/cc-06.pdf
Chapter 7: Fiscal/Employer Agent Services
http://www.cashandcounseling.org/resources/pdf/cc-07.pdf
Chapter 8: Quality Management in Self-Direction Programs
http://www.cashandcounseling.org/resources/pdf/cc-08.pdf
Chapter 9: Self-Direction and Health Care
http://www.cashandcounseling.org/resources/pdf/cc-09.pdf

201
Chapter 7: Participant-Directed Services and Supports
Chapter 10: Looking Ahead
http://www.cashandcounseling.org/resources/pdf/cc-10.pdf
Appendix I: Using Strategic Communications
http://www.cashandcounseling.org/resources/pdf/cc-app1.pdf
Appendix II: The Consumer Direction Module
http://www.cashandcounseling.org/resources/pdf/cc-app2.pdf
Appendix III: History of Self-Direction
http://www.cashandcounseling.org/resources/pdf/cc-app3.pdf
CMS State Medicaid Director Letter (November 19, 2009). Implementation of §6087 of DRA §1915(j).
This letter provides guidance on the implementation of §6087 of the Decit Reduction Act of 2005, Public Law
Number 109-171. Section 6087, the “Optional Choice of Self-Directed Personal Assistance Services (PAS) (Cash
and Counseling),” amended §1915 of the Social Security Act by adding a new subsection (j). The guidance also
applies to §1915(c) HCBS waiver programs when states oer the self-direction opportunity and permit partici-
pants to purchase “Individual Directed Goods and Services.” The letter oers information on (1)Background,
(2)Medicaid Authorities, (3)Criteria, (4)Support and Monitoring, and (5)Compliance with the Guidance.
Available at http://www.cms.hhs.gov/SMDL/SMD/ItemDetail.asp?ItemID=CMS1230894
CMS. (2008). Application for a §1915(c) Home and Community-Based Waiver [Version 3.5]: Instructions,
Technical Guide and Review Criteria.
The Application contains extensive information concerning Federal policies that apply to the operation of an
HCBS waiver, in particular, Appendix E: Participant Direction of Services, which addresses how the waiver af-
fords participants the opportunity to direct some or all of their waiver services. The addition of Appendix E to
the waiver application recognizes that participant direction is an increasingly common feature of waivers.
Available at https://www.hcbswaivers.net/CMS/faces/portal.jsp under links and downloads, entitled §1915(c)
Waiver Application and Accompanying Materials.
Brown, R., Lepidus Carlson, B., Dale, S., Foster, L., Phillips, B., and Schore, J. (2007). Cash & Counseling:
Improving the Lives of Medicaid Beneciaries Who Need Personal Care or Home and Community-Based
Services. Princeton, NJ: Mathematica Policy Research, Inc.
This report summarizes the ndings from 5 years of research by Mathematica Policy Research, Inc. on how
each of the three Cash and Counseling Demonstration states implemented its program, and on how the pro-
grams have aected participants, their paid and unpaid caregivers, and Medicaid costs.
202 Understanding Medicaid Home and Community Services: A Primer
Available at http://www.cashandcounseling.org/resources/20070910-145713/index_html
Websites
National Association of State Medicaid Directors
This website contains information about the Medicaid program, including all State Medicaid Director Letters
issued since 2004, links to state Medicaid websites, information about Medicaid statutory and regulatory is-
sues, and current Federal legislative and policy initiatives.
Web address: http://www.nasmd.org/Home/home_news.asp
Cash and Counseling National Program Oce
This website contains extensive, wide-ranging resources concerning participant direction.
Web address: http://www.cashandcounseling.org/
National Resource Center for Participant-Directed Services (NRCPDS)
Drawing on over a decade of experience with participant direction and experience as a National Program Of-
ce for the Cash and Counseling project, the NRCPDS provides technical assistance to develop and improve
participant direction programs, regardless of funding source. The website contains extensive resources on
participant direction.
Web address: http://www.bc.edu/schools/gssw/nrcpds/
The Clearinghouse for Home and Community Based Services
This site promotes the development and expansion of HCBS by gathering resources and tools for research,
policymaking, and program development into this one-stop website. Under the topic Consumer/Participant
Direction, there are 520 publications, including policy alerts and briefs, promising practices, and reports.
Web address: http://www.hcbs.org/
203
Chapter 7: Participant-Directed Services and Supports
Endnotes: Citations, Additional Information,
and Web Addresses
1
The original chapter was co-authored by Gary Smith, Pamela Doty, and Janet O’Keee. The informa-
tion in this chapter is drawn from several sources. The section on consumer choice and provider quali-
cations is from the original Primer chapter. The sections on Basic Features of Participant Direction of
Medicaid HCBS and Federal Medicaid Statutory Authorities, authored by Gary Smith, are taken verba-
tim from Chapter 2 of the publication Developing and Implementing Self-Direction Programs and Poli-
cies: A Handbook. (See the Resources section of this chapter for the full citation, including web links to
the entire document and to the individual chapters.) The section on Financial Management Services
(FMS) is a brief condensation of information in Chapter 7, Fiscal/Employer Agent Services, authored by
Susan Flanagan in the same publication. Suzanne Crisp and Janet O’Keee updated all other sections.
2
Family involvement is not always needed or appropriate, but many participants desire or require it.
3
Brown, R., Lepidus Carlson, B., Dale, S., Foster, L., Phillips, B., and Schore, J. (2007). Cash & Counseling:
Improving the Lives of Medicaid Beneciaries Who Need Personal Care or Home and Community-
Based Servi ces. Princeton, NJ: Mathematica Policy Research, Inc. Available at http://www.cashand-
counseling.org/resources/20070910-145713/index_html.
4
Phillips, B. et al. (2003). Lessons from the Implementation of Cash and Counseling in Arkansas, Florida
and New Jersey. Washington, DC: Department of Health and Human Services, Assistant Secretary for
Planning and Evaluation. Available at http://aspe.hhs.gov/daltcp/reports/cclesson.htm.
5
In the developmental disabilities eld, the term “circle of support” is used to describe such informal
supports.
6
Doty, P., Kasper, J., and Litvak, S. (1996). Consumer-Directed Models of Personal Care: Lessons from
Medi caid. The Milbank Quarterly, 74(3):377-409. Available at http://aspe.hhs.gov/daltcp/reports/les-
sons.htm.
7
CMS collaborated with Arkansas, Florida, and New Jersey to design programs under the §1115 Re-
search and Demonstration waiver authority (hereafter referred to as the §1115 waiver authority) to
implement the demonstration and to evaluate the benets of this approach. The demonstration
was launched in the three states between 1998 and 2000, using a random assignment social experi-
mental design to address selection bias, which yielded robust data about the positive benets of the
Cash and Counseling approach to participant direction. Phillips, B. et al. (2003), op. cit. Several more
reports about the results of the demonstrations are located at http://aspe.hhs.gov/_/topic/topic.
cfm?topic=Consumer%20Choice.
8
Notably, fewer than a dozen participants in all three states selected the cash option. Pamela Doty, Of-
ce of the Assistant Secretary for Planning and Evaluation. Personal communication, July 2008.
9
More information about this program is available at http://www.rwjf.org/reports/npreports/sdpdd.
htm.

204 Understanding Medicaid Home and Community Services: A Primer
10
A few states oered employer authority prior to the Independence Plus initiative.
11
CMS. (2008). Application for a §1915(c) Home and Community-Based Waiver [Version 3.5] Instructions,
Technical Guide and Review Criteria. See the Resources section of this chapter for a web link to the ap-
plication instructions.
12
P.L. 109-171.
13
The DRA-2005 also provides that states may oer participants in Money Follows the Person (MFP)
demonstrations the authority to direct their services and supports. Section 6071 of DRA-2005 also au-
thorized the Secretary of HHS to award $1.75 billion in special MFP demonstration grants over a 5-year
period to states to support the transition of individuals from institutional settings to the community.
These grant funds may be used to pay for special transition services to facilitate community place-
ment. States are also eligible to receive an enhanced Federal Medical Assistance Percentage (FMAP) for
a 1-year period for the costs of HCBS furnished to persons who move to the community.
After 1 year, the state must ensure that individuals will continue to receive HCBS through the Medicaid
State Plan and/or an HCBS waiver. In order to qualify for the enhanced FMAP, individuals must transi-
tion to community living arrangements that they own or lease, their family home, or a community-
based residential setting where no more than four unrelated people reside. CMS has awarded MFP
grants to 31 states to support the transition of individuals from nursing facilities, intermediate care
facilities for persons with intellectual disabilities, and other institutional settings to the community.
Section 6071(c) of DRA-2005 specically provides that a state may oer MFP demonstration partici-
pants the authority to direct their HCBS. The participant direction elements of the MFP authority
closely parallel the participant direction provisions contained in the §1915(i) HCBS State Plan author-
ity. These elements include providing for a person-centered service plan development process and the
option for the state to give participants choice and control over an individual budget. More informa-
tion concerning MFP is located at http://www.cms.hhs.gov/DecitReductionAct/20_MFP.asp
14
As provided in §1902(a)(23) of the Social Security Act, participants may select any qualied and willing
provider to furnish services. A signicant number of states restrict freedom of choice of FMS provider
because the cost of monitoring large numbers of FMS providers often outweighs the benet of receiv-
ing a higher FMAP matching payment.
15
The terms primary and secondary employer are often used in states’ unemployment statutes to de-
scribe the role of employers under a “co-employer” model.
16
Individuals may establish additional qualications as long as they do not contradict those that the
state has established. For example, a person may require that the worker can communicate in sign
language.
17
CMS. (2008). Application for a §1915(c) Home and Community-Based Waiver [Version 3.5] Instructions,
Technical Guide and Review Criteria, p. 195. See the Resources section of this chapter for a web link to
the application instructions.
18
Home and community services may be delivered under additional authorities and through vari-
ous service delivery arrangements. For example, the delivery of Medicaid health and long-term care
services may be integrated under the §1915(a) authority. HCBS also may be included in managed care
programs oered under the provisions of §1932 of the Social Security Act. The Medicare Prescription
Drug, Improvement, and Modernization Act of 2003 created a new type of Medicare coordinated
care health plan, the Medicare Special Needs Plan (SNP). SNPs may be created to “wrap around” the

205
Chapter 7: Participant-Directed Services and Supports
delivery of health and long-term care services for persons who are dually eligible for Medicare and
Medicaid. Section 6044 of the DRA-2005 gives states the option to create alternative Medicaid benet
packages, including tailored benets to meet participants’ special health needs. As a general matter,
participant direction options may be employed in conjunction with these other authorities or service
delivery arrangements.
19
Section 1115 of the Social Security Act gives the Secretary of HHS wide-ranging authority to grant
states waivers of Federal Social Security Act provisions for the purpose of demonstrating and evaluat-
ing alternative approaches to service delivery. When a state is interested in testing such alternative
approaches, this waiver authority provides states with a means to obtain relief from statutory require-
ments that stand in the way of implementing them. A state is required to develop a research strategy
to assess the extent to which its alternative approach results in improved or more ecient delivery of
services to participants. In recent years, states principally have employed this authority to restructure
the delivery of Medicaid health care services rather than long-term care services. The authority also
has been employed to expand eligibility for Medicaid services. Section 1115 waivers operate under
“budget neutrality” requirements (i.e., expenditures can be no higher under the waiver than they
would otherwise have been).
20
It was necessary to use this authority in the Cash and Counseling demonstrations, which oered par-
ticipants a cash option, permitted participants to redirect personal care/assistance funds to purchase
other goods and services, and allowed payment of legally responsible relatives for services.
21
Source: Mary Sowers, CMS. Personal communication, December 11, 2009.
22
Centers for Medicare & Medicaid Services. (2005). Medicaid-At-A-Glance: 2005. Available at http://
www.cms.hhs.gov/MedicaidGenInfo/downloads/MedicaidAtAGlance2005.pdf.
23
The exact number of states is not known.
24
Must provide option to transition to traditional services under §1905(a)(24) and §1915(c) authorities.
25
These two states furnish HCBS to Medicaid participants under the §1115 waiver authority.
26
CMS stressed the use of person-centered planning, provided guidance to states on establishing
individual budgets, dened requirements for supporting participants who direct their services (e.g.,
through the provision of nancial management services and information and assistance services), and
provided guidance on how states could permit waiver program participants to exercise choice and
control over the selection of workers and their individual budgets.
27
CMS also issued a §1115 waiver template for the same purpose.
28
CMS worked in collaboration with several state agency associations that have operational responsibili-
ty for HCBS delivery: the National Association of State Directors of Developmental Disabilities Services,
the National Association of State Units on Aging, the National Association of State Medicaid Directors,
the National Association of State Head Injury Administrators, and the Alliance of Cash and Counseling
States.
29
The Version 3.3 HCBS waiver application was released in November 2005 but has since been replaced
by subsequent versions. Version 3.5 was issued in January 2008. CMS continually updates the waiver
application and the current version is also being updated. Version 3.6 is expected to be released in late
2010 or early 2011. With respect to participant direction, there are no substantive dierences in the
treatment of participant direction among the various versions of the application.

206 Understanding Medicaid Home and Community Services: A Primer
30
CMS. (2008). Application for a §1915(c) Home and Community-Based Waiver [Version 3.5] Instructions,
Technical Guide and Review Criteria. See the Resources section of this chapter for a web link to the ap-
plication instructions.
31
Appendix E built upon the participant direction elements that were contained in the predecessor
Independence Plus waiver application template.
32
Waiver of comparability has traditionally been interpreted to mean that states can have multiple
waivers oering dierent kinds of services for dierent populations. However, there has also been a
legal interpretation by General Counsel that there can be no waiver of comparability within waivers.
Unlike the §1915(j) authority, HCBS waiver rules do not have an explicit prohibition on self-direction
for group home residents. However, as a practical matter, group home residents can not direct their
services if they are provided by facility sta or outside sta through arrangements with the facility.
Basically, if waiver participants choose to live in a group residential service setting, by denition they
are choosing to use services they can not direct. However, it is technically possible that “some” services
not provided by the facility could be self-directed.
33
It is important to specify that a representative may be the common law or managing employer be-
cause in both cases, the employer must be someone who can successfully participate in an unemploy-
ment or worker’s compensation appeal.
34
State Medicaid Director Letter regarding how to check for excluded providers, available at http://www.
cms.gov/smdl/downloads/SMD061208.pdf.
35
In the Instructions, Technical Guide, and Review Criteria that accompanies the HCBS waiver applica-
tion, p.172, CMS has dened Individual Directed Goods and Services as “services, equipment or sup-
plies not otherwise provided through this waiver or through the Medicaid State Plan that address an
identied need in the service plan (including improving and maintaining the participant’s opportuni-
ties for full membership in the community) and meet the following requirements: the item or service
would decrease the need for other Medicaid services; AND/OR promote inclusion in the community;
AND/OR increase the participant’s safety in the home environment; AND, the participant does not
have the funds to purchase the item or service or the item or service is not available through another
source. Individual Directed Goods and Services are purchased from the participant-directed budget.
Experimental or prohibited treatments are excluded. Individual Directed Goods and Services must be
documented in the service plan.”
36
A few states extend the coverage of Individual Directed Goods and Services to waiver participants
who do not formally self-direct. More commonly, the coverage is conned to individuals who self-
direct and exercise budget authority. For example, West Virginia includes this coverage in its Personal
Options participant direction program in its Medicaid HCBS waiver for older persons and individuals
with disabilities. Waiver participants may save up to $1,000 from their budget to purchase participant-
directed goods and services. For more information, go to http://www.cashandcounseling.org/resourc-
es/20070611-111748.
37
Issued on November 19, 2009. Available at http://www.cms.hhs.gov/SMDL/downloads/SMD111909.
pdf.
38
Participant direction programs pose dierent risks than do traditional service delivery programs. In
both programs, a risk always exists that workers will not show up. But when participants assume the
role of employer and a professional service provider is no longer overseeing service delivery, partici-
pants themselves must assume the responsibility of managing sta and assessing quality. Participants

207
Chapter 7: Participant-Directed Services and Supports
who employ their workers may also be liable if employment-related taxes and workers compensation
insurance premiums are not paid. Consequently, CMS requires states to (1)institute safeguards and
supports to minimize participants’ potential liability (including the use of strong scal employer agent
models), and (2)develop quality management and improvement systems sucient to safeguard the
health and welfare of individuals in participant direction programs. States must also continue to meet
all other statutory assurances required when operating a waiver program.
39
When nancial management services are furnished as a Medicaid administrative activity, costs are
reimbursable at the standard 50 percent administrative claiming rate for federal nancial participa-
tion. Under this option, a state may limit the number of FMS entities, for example, by selecting them
through a competitive process. When nancial management services are furnished as a waiver service,
the costs are reimbursable at the state’s services claiming rate, which may be higher than 50 percent
and any willing and qualied provider must be permitted to furnish nancial management services.
When the services are covered as a waiver service, a state also may designate the FMS provider as an
“organized health care delivery system.” Such a designation may simplify compliance with Medicaid
provider agreement requirements. There is an extensive discussion of the provision of nancial man-
agement services as an administrative activity or as a covered waiver service in the CMS HCBS Waiver
Application Instructions, Technical Guide, and Review Criteria, including managing provider agree-
ments. See the Resources section of this chapter for a web link to the Application Instructions.
40
Another option for providing counseling services to self-directing HCBS waiver participants is the
use of targeted case management services (paid as a State Plan service). See the Resources section of
this chapter for additional information on counseling services and Chapter 4 for information on the
targeted case management option.
41
The §1915(b) waiver authority permits a state to obtain a freedom of choice waiver in order to limit the
providers of Medicaid State Plan services. Some states (e.g., Michigan and Wisconsin), and sometimes
jurisdictions within a state, operate programs under concurrent §1915(b)/§1915(c) waivers. For exam-
ple, the North Carolina Piedmont Cardinal Health Plan operates under concurrent §1915(b)/§1915(c)
waivers to provide mental health and developmental disabilities services in a ve-county area.
See also Chapter 9: Incorporating Self-Direction Options in Managed Care Plans from the publication
Developing and Implementing Self-Direction Programs and Policies: A Handbook. See the Resources
section of this chapter for the full citation and web link to the chapter.
42
A state can restrict freedom of choice of nancial management services entities and information and
assistance providers in a (b)(c) waiver program and receive Federal matching funds under the service
rate rather than the administrative rate, as long as the service is included in the approved §1915(b)(4)
request.
43
The text of §1915(i) is located at http://www.paelderlaw.com/pdf/DRA_Provisions.pdf.
44
Section 1915(i)(1)(G)(iii) of the Social Security Act.
45
See Chapter 5, Individual Budgeting from the publication Developing and Implementing Self-Direc-
tion Programs and Policies: A Handbook. See the Resources section of this chapter for the full citation
and web link to the chapter.
46
The authority denes participant direction as follows: “The participant (or in the case of a participant
who is a minor child, the participant’s parent or guardian, or in the case of an incapacitated adult,
another individual recognized by state law to act on behalf of the participant) exercises choice and

208 Understanding Medicaid Home and Community Services: A Primer
control over the budget, planning, and purchase of participant-directed personal assistance services,
including the amount, duration, scope, provider, and location of service provision.” The text of §1915(j)
is located at http://www.paelderlaw.com/pdf/DRA_Provisions.pdf.
47
Dierent Medicaid authorities use dierent terms to describe the same service. As noted previously,
the terms personal assistance, personal care, and attendant services encompass the same service: as-
sistance performing activities of daily living (ADLs) and instrumental activities of daily living (IADLs).
48
Available at http://www.cms.hhs.gov/SMDL/downloads/SMD091307.pdf. The letter provides guidance
on the implementation of Section 6087, Optional Participant Direction Personal Assistance Services
Program of the Decit Reduction Act of 2005.
49
Available at http://www.cms.hhs.gov/SMDL/downloads/SMD091307Encl.pdf.
50
On October 3, 2008, CMS published a nal rule in the Federal Register (73 Fed. Reg. 57,854) providing
guidance to states that choose to administer self-directed personal assistance services through their
Medicaid State Plan, as authorized by the DRA-2005. Available at http://edocket.access.gpo.gov/2008/
E8-23102.htm.
51
A cash option would be allowed under a §1115 waiver, but CMS is no longer approving the use of this
authority solely to implement participant-directed services options. However, if a participant direction
program is a component of a broader Medicaid reform proposal, the authority could be used.
52
Available at http://www.cms.hhs.gov/SMDL/downloads/SMD111909.pdf.
53
Under the §1915(j) authority, CMS does not require states to mandate the use of nancial manage-
ment services for participants who elect the “cash” option. Instead, these participants may choose to
retain responsibility for some or all of their scal and employer-related responsibilities. Individuals
who receive cash benets have the option to hire an FMS provider or a private accountant to perform
employer tasks, such as payment of payroll taxes. Participants who choose to perform these tasks
themselves must comply with all applicable employment and tax laws.
54
42 CFR Subpart G—Home and Community-Based Services: Waiver Requirements. Available at http://
law.justia.com/us/cfr/title42/42-3.0.1.1.10.7.html.
55
The service plan is based on a needs assessment that determines how many hours of aide services will
be authorized for payment. Some states also require specication of tasks the aide will perform, and in
some of these states the number of hours authorized is determined by the time allocated for particu-
lar tasks, such as bathing, dressing, and meal preparation.
56
Some states require the representative to be a legal entity, such as a guardian, which limits partici-
pants’ choice of representatives.
57
If representatives serve their own interests rather than those of participants, the counselor may advise
a change of representative.
58
At §441.480.
59
Statute available at http://www.ssa.gov/OP_Home/ssact/title19/1915.htm.
60
Federal Register, 73(193):57885 (444.480).
61
CMS. (2008). Application for a §1915(c) Home and Community-Based Waiver [Version 3.5], Instructions,

209
Chapter 7: Participant-Directed Services and Supports
Technical Guide and Review Criteria. p.173. See the Resources section of this chapter for a web link to
the application instructions.
62
O’Keee, J. (1996). Determining the Need for Long-Term Care Services: An Analysis of Health and Func-
tional Eligibility Criteria in Medicaid Home and Community-Based Waiver Programs. Washington, DC:
AARP Public Policy Institute.
63
Available at http://www.hhsc.state.tx.us/Contract/529060406/nal/Attachment_H.pdf.
64
They may also do so under the §1115 waiver authority.
65
Kathy Kelly, Minnesota Department of Human Services, Disability Services Division, Supervisor of
Policy Implementation in the Home & Community Living Services Group. Personal communication,
January 27, 2010.
66
This section is condensed from Chapter 7 on Fiscal/Employer Agent Services, authored by Susan Fla-
nagan, Ph.D., M.P.H., from the publication Developing and Implementing Self-Direction Programs and
Policies: A Handbook. See the Resources section of this chapter for the full citation and web link to the
chapter.
67
CMS. (2008). Application for a §1915(c) Home and Community-Based Waiver [Version 3.5], Instruc-
tions, Technical Guide and Review Criteria. Appendix C: Participant Services, Attachment: Core Services
Denitions, Section D, Services in Support of Participant Direction, #2 Financial Management Services,
p. 176. See the Resources section of this chapter for a web link to the application instructions.
68
Ibid. Appendix E, Overview: Financial Management Services, p. 201.
69
Medicaid funds may also be disbursed directly to participants in programs under the §1115 authority.
However, as stated above, CMS will generally not approve a §1115 waiver solely to oer a participant
direction program.
70
The term “neutral bank” is used because the F/EA is not providing direct care services to participants
so it is “neutral” about which providers they use. Prior to the use of F/EAs, some participants with de-
velopmental disabilities found it dicult to move between/among agency service providers because
their Medicaid benet was often allocated to one service organization for the scal year, which had a
nancial interest in who provided services to participants.
71
Payroll includes, but is not limited to, the collection and processing of worker timesheets; making sure
that workers are paid in accordance with Federal and state labor laws; the withholding, ling, and pay-
ment of Federal and state income tax withholding and employment taxes, and locality taxes; process-
ing of the advanced Federal earned income credit, when applicable, and any garnishments, liens, or
levies against workers pay, as required; and generating and distributing payroll checks.
72
When participants are not able or willing to act solely as their workers’ employer, their representatives
can assume this role if they are willing to do so.
73
Flanagan, S.A., and Green, P.S. (2000). Fiscal Intermediaries: Reducing the burden of consumer-directed
support. Generations, 24(111):94-95. This publication describes the development of Fiscal/Employer
Agents and various issues regarding their use.
74
Participants’ choice of provider is limited because, per IRS regulations, only one entity (a Government
F/EA, or its reporting agent or subagent if it chooses to use one) can le and deposit the required
Federal taxes for participants and their workers under the same entity name and Federal Employer

210 Understanding Medicaid Home and Community Services: A Primer
Identication Number on the required IRS Forms.
75
However, if a state implements a Medicaid State Plan participant direction program in accordance
with §1915(j) of the Social Security Act, the costs associated with Vendor F/EA services must be billed
as an administrative expense for the purpose of claiming Federal matching funds.
76
States that limit the number of Vendor F/EA providers available to participants include, but are not
limited to, Alabama, Arkansas, Arizona, Connecticut, Florida, Idaho, Iowa, Illinois, Maryland, Massachu-
setts, Kansas (WORK Program), Missouri, Nevada, New Jersey, New Mexico, Pennsylvania, Tennessee,
Virginia, Vermont, and West Virginia. States that restrict participant choice of F/EA provider, including
states that implement Government F/EAs or Medicaid State Plan amendments in accordance with
§1915(i) and §1915(j) of the Social Security Act, are reimbursed for F/EA costs at the Federal adminis-
trative matching rate.
Alabama has implemented a pilot participant direction program under its Medicaid State Plan by
using the §1915(j) authority. New Jersey converted its Personal Preference Program from operating
under a Medicaid §1115 waiver to the §1915(j) authority eective July 1, 2008. The Missouri Division of
Developmental Disabilities has implemented a Government F/EA and performs all tasks internally. Ne-
vada plans to implement a participant-directed services pilot for individuals with developmental dis-
abilities living in rural areas sometime in 2010. West Virginia’s Bureau of Medical Services and Florida’s
Department of Elder Aairs and Agency for Persons with Disabilities have implemented a Government
F/EA and use a subagent.
77
States include, but are not limited to, Pennsylvania (53 percent Medicaid service match rate), Michigan
(58.10 percent Medicaid service match rate), Minnesota (50 percent Medicaid service match rate), and
Rhode Island (52.35 percent service match rate).
78
CMS. (2008). Application for a §1915(c) Home and Community-Based Waiver [Version 3.5], Instruc-
tions, Technical Guide and Review Criteria. Appendix E, Item E-1-i: Provision of Financial Management
Services, p.205. See the Resources section of this chapter for a web link to the application instructions.
79
Ibid.
80
Chapter He-P600, Part He-P601, Certication of Other Qualied Agencies.
81
The administrative burden for states of having multiple FMS providers is signicant and the cost often
exceeds the funds a state receives through the receipt of FMAP. In addition, the potential liability as-
sociated with poor performance by FMS providers increases when they do not have enough business
to stay current with Federal and state requirements. For example, if a state has 75 FMS providers, but
only 25 are regularly serving clients and 50 are not serving anyone, those without clients are at risk of
not staying up-to-date with Federal and state requirements. A similar situation can occur with having
too many counselors (i.e., information and assistance providers). New Jersey’s Personal Preference Pro-
gram found that only a small number of counseling agencies were serving the majority of consumers
while the others were serving very few consumers and were not keeping up with requirements.
82
Medicaid Manual Transmittal Part 4, N. 73, September 17, 1999. Available online as part of the State
Medicaid Manual, Chapter 4: Services, 4444 to 4658, at http://www.cms.hhs.gov/Manuals/PBM/item-
detail.asp?lterType=none<erByDID=-99&sortByDID=1&sortOrder=ascending&itemID=CMS02192
7&intNumPerPage=10.
83
Available at http://www.cms.hhs.gov/smdl/downloads/smd072500b.pdf.

Chapter 8: Medicaid Authorities for Delivering Home and Community Services through Risk-Based Managed Care Systems
211
Guide to Chapter 8
Evolution of Medicaid Long-Term Care in Managed Care Systems . . . . . . . . . . . . . . . . . . . . . . .213
Early Growth of Medicaid Managed Care . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .214
Recent Trends . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .214
Reasons for Developing MLTC Programs . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .215
Challenges to Implementing MLTC Programs . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .216
Medicaid Authorities . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .216
Section 1115 Waivers . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .219
Concurrent §1915(b) and §1915(c) Waivers . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .220
Section 1915(a) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .221
Section 1932(a) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .222
Section 1934 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .222
Medicare Special Needs Plans . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .223
Section 1915(i) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .224
All Quality and Other Requirements of Each Authority Must Be Met . . . . . . . . . . . . .224
Resources. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .225
Endnotes: Citations, Additional Information, and Web Addresses . . . . . . . . . . . . . . . . . . . . . . .229
213
Chapter 8: Medicaid Authorities for Delivering Home and Community Services through Risk-Based Managed Care Systems
Chapter 8
Medicaid Authorities for Delivering
Home and Community Services through
Risk-Based Managed Care Systems
Managed care is an approach to nancing and delivering health care that aims to enhance value by controlling
costs while improving quality. Risk-based managed care is dened as a nancing and delivery system in which a
contractor is paid a set monthly fee per person enrolled (called a capitation rate), and bears nancial risk for provid-
ing a dened package of services to the enrolled population. Forty-six states use risk-based Medicaid managed care;
it is the most commonly used approach for organizing and nancing primary and acute health care. But, apart from
the Program of All-inclusive Care for the Elderly (PACE) model, only 11 states have applied risk-based managed care
approaches in the delivery of long-term care—either institutional or home and community services and supports.
Recently, however, the number of people receiving these services and supports through managed care delivery
systems has grown signicantly.
This chapter discusses the Medicaid authorities that states can use to provide home and community services
through risk-based managed care delivery systems. It briey decribes the history of programs that include long-term
care services in managed care arrangements, and discusses how Medicaid authorities have evolved over time. Be-
cause the majority of Medicaid-eligible individuals who need long-term care also have Medicare coverage—known
as people who are dually eligible—some programs are designed to integrate Medicaid and Medicare funding for
these beneciaries. Thus, this chapter also briey discusses the Medicare authority for integrated service delivery
models
.1
Evolution of Medicaid Long-Term Care in Managed Care Systems
Prototype Medicaid managed care programs that include long-term care services and supports go back to the
1980s, when the PACE demonstration grew out of San Francisco’s innovative On Lok program, and the Arizona
Long-Term Care System (ALTCS) was implemented. Both of these programs were implemented under the Sec-
tion (§)1115 Research and Demonstration waiver authority (hereafter referred to as a §1115 waiver).
PACE and ALTCS are very dierent programs, but they have one important feature in common: their contrac-
tors receive a monthly capitation fee per member regardless of the amount of services their members use. This
contrasts with the usual fee-for-service approach used to pay for home and community-based services (HCBS).
214 Understanding Medicaid Home and Community Services: A Primer
Thirty states now operate PACE sites under a §1934
State Plan amendment, and ALTCS continues to
operate as a statewide demonstration program
under a §1115 waiver. (More information about
these programs and the authorities under which
they operate is provided later in this chapter.) De-
spite the early eorts of these enduring programs,
it was several years before a few other states began
fashioning managed long-term care (MLTC) models
of their own.
Early Growth of Medicaid
Managed Care
In the 1980s, many states were implementing
Medicaid managed health care. Their eorts were
focused on the largest groups of beneciares: fami-
lies and children who qualied for Medicaid based
on their eligibility for cash assistance through Aid to
Families with Dependent Children (now Temporary
Assistance to Needy Families). Individuals eligible
for Medicaid through Supplemental Security In-
come (SSI) typically were excluded from managed
health care, or included on a voluntary basis.
2
When
SSI-related groups were included, their long-term
care services were almost always “carved out” and
continued to be delivered through the traditional
fee-for-service system. This was in part because
early Medicaid man aged care programs were build-
ing on the exper ience of commercial managed care
organizations (MCOs) that provided only primary
and acute health care.
Growth of Medicaid managed health care accel-
erated in the 1990s. By 1998, state survey data
showed that a majority of Medicaid beneciaries
were enrolled in some form of Medicaid managed
care. About two-thirds of Medicaid managed care
enrollment was in risk-based commercial or Medic-
aid-only MCOs.
3
The remaining third were enrolled
in primary care case management, which assigns
primary care providers to members but does not
capitate payments.
In the 1990s, a number of states began applying
risk-based managed care strategies to the provi-
sion of long-term care services. These included both
Medicaid-only models, which focused exclusively
on Medicaid-funded services, and integrated mod-
els, which included both Medicaid and Medicare
services for persons who were dually eligible. New
integrated programs were implemented in two
states: the Wisconsin Partnership Program (1995)
and Minnesota Senior Health Options (1997). Three
Medicaid-only programs were launched in the
same period: New York Managed Long-Term Care
(1997), Texas Star+Plus (1998), and Florida Diversion
(1998).
4
The Balanced Budget Act (BBA) of 1997 included
signicant changes to Federal Medicaid managed
care policy. For the rst time, Federal law allowed
states under certain conditions to implement man-
datory Medicaid managed care programs without
the need for Federal waivers (i.e., a state could
require certain Medicaid participants to enroll in a
new managed care program). However, individuals
eligible for both Medicaid and Medicare (hereafter
called dually eligible persons) and children with
special health and/or long-term care needs were
specically excluded from those provisions. The
change in Federal policy recognized that managed
care had become the dominant delivery system for
families and children, but was still relatively untest-
ed among SSI-eligible groups.
Recent Trends
Facilitated by the policy changes in the BBA, Med-
icaid managed care for families and children has
continued to grow in the past decade. By June 2008,
the Centers for Medicare & Medi caid Services (CMS)
reported that 71 percent of Medicaid enrollees were
in managed health care of some type in 48 states,
including risk-based arrangements and primary
care case management.
5
As about two-thirds of the
managed care enrollment is in risk-based arrange-
ments in 46 states, risk-based arrangements are the
dominant form of Medicaid managed care.
6
How-
ever, populations receiving long-term services have
largely continued to be excluded from states’ Med-
icaid managed care initiatives. For example, one sur-
vey showed that 90 percent of states with managed
care service delivery models excluded persons in
215
Chapter 8: Medicaid Authorities for Delivering Home and Community Services through Risk-Based Managed Care Systems
long-term institutional settings, 73 percent exclud-
ed dually eligible persons, and 71 percent excluded
persons receiving home and community services.
7
As a percentage of overall Medicaid managed care
programs, MLTC continues to be small, but a num-
ber of new Medicaid-only and integrated MLTC
initiatives have been implemented since 2000 and
some of the early MLTC programs have grown sub-
stantially. In 2000, Wisconsin piloted its Medicaid-
only Family Care Program in ve areas of the State
and by 2009 had almost completed its statewide
expansion. In 2001, building on its experience with
Senior Health Options, Minnesota launched its
Disability Health Options, an integrated Medicaid-
Medicare program for adults with physical disabili-
ties, and in 2005, expanded Senior Health Options
statewide. Texas has also engaged in a multi-region
expansion of Star+Plus.
In 2004, Massachusetts implemented the integrated
Senior Care Options program, and in 2008, New
Mexico began implementing its Coordinated Long
Term Services program, a mandatory, statewide
Medicaid managed care program with an estimated
38,000 persons enrolled. Hawaii implemented Quest
Expanded Access in 2009, adding an estimated
39,000 persons to the national MLTC enrollment.
As of 2009, 11 states were providing long-term care
services and supports through risk-based managed
care arrangements outside of PACE programs, and
one additional state has been approved to imple-
ment an MLTC initiative.
8
So, although MLTC con-
tinues to be the exception rather than the rule, it is
slowly being adopted by additional states.
Reasons for Developing
MLTC Programs
The key feature of risk-based managed care is that a
contractor bears nancial risk for services provided
over time and across settings. The contractor is paid
a capitation rate per enrollee and is responsible for
providing all contracted benets under this rate. If
the actual cost of providing services exceeds the
aggregate capitation amount, the contractor experi-
ences a loss, but if services can be provided at or
below the capitation amount, the contractor prots.
As applied to long-term care, this approach creates
an incentive to avoid institutional care whenever
possible through the provision of cost-eective
home and community services.
States commonly cite the following goals as reasons
to develop MLTC.
• Strengthen accountability for quality. When
bolstered by a robust quality improvement
component, MLTC can hold contractors ac-
countable for consumer outcomes over time
and across service settings. Given that many
individuals who receive long-term care ser-
vices have complex, multi-service needs, the
ability to hold contractors accountable for a
broad range of services across multiple service
settings is critical to quality improvement.
Absent a single, accountable contractor, it is
very dicult to work on preventing avoidable
hospitalization or institutionalization.
• Streamline and coordinate access to servi-
ces. A good care management system can
help address the lack of coordination across
primary, acute, and long-term services. Such
coordination is particularly important in inte-
grated programs for dually eligible persons.
Care management is also critical in traditional
HCBS waiver programs, but care managers
are limited to managing waiver services and
have little or no interaction or inuence with
primary and acute health care providers.
• Complement state eorts to better balance
their long-term service systems. States see
MLTC as an eective vehicle for reducing the
unnecessary use of institutional services and
increasing the use of home and community
services. In the fee-for-service system, such
balancing eorts often face a nancing obsta-
cle: states need to increase resources for home
and community services while maintaining
funding for institutional care. The exibility of
capitation addresses this problem when com-
munity and institutional services dollars are
blended in a single capitation rate. The con-
tractor has the exibility to use the capitation
rate in the most appropriate way that meets
216 Understanding Medicaid Home and Community Services: A Primer
the needs and preferences of the consumer.
In essence, the capitation becomes a exible,
portable, and global budget.
9
Challenges to Implementing
MLTC Programs
Implementing MLTC programs has proven to be
more challenging than traditional Medicaid man-
aged primary and acute health care for families and
children. Major issues are summarized below.
• Consumers and advocates worry about
underservice and loss of control. Despite ef-
forts to emphasize person-centered concepts
in MLTC programs, many consumers and their
advocates worry that contractors will be nan-
cially motivated to reduce access to services,
limit consumer choice, and provide service
plans that are less tailored to members’ indi-
vidualized needs. To address these and related
concerns, states must engage consumers early
on and throughout program development,
implementation, and evaluation, recognizing
that a meaningful engagement process with
consumers requires a substantial commitment
of time and resources.
• Entities involved in delivering HCBS resist
role changes. In particular, organizations to
whom the state has delegated case manage-
ment of waiver services, such as counties, Area
Agencies on Aging, and Independent Living
Centers, generally do not want to cede that
responsibility to MCOs. States must work with
these entities to help them redene their roles,
and in some programs, to forge formal part-
nerships with MCOs.
• Infrastructure is lacking at the state and
service delivery levels. Commercial MCOs
generally lack experience providing long-term
care services, while state Medicaid agencies
and traditional HCBS providers lack experience
managing risk. Additionally, because state
legislatures often equate managed care with
privatization, they may expect to reduce state
administrative positions when MLTC is imple-
mented. A major education eort may be
needed for the state legislature to understand
that implementing a managed care program
does not result in a need for fewer state
agency sta.
• Rate setting is complex. Considerable varia-
tion in the needs of the population served
presents a major challenge to the rate setting
process. One person may need only a few
hours of personal assistance per day, while
another might need several months of nurs-
ing facility care; also, an individual’s needs can
vary over time. Determining a capitation rate
to pay appropriately for this potential range of
services, while also building appropriate incen-
tives to provide HCBS instead of institutional
services, is a complex task.
• High incidence of dually eligible persons.
One of the greatest challenges is the high
incidence of dually eligible persons among the
population in need of long-term care. While a
state may conclude that a Medicaid-only pro-
gram will have too few participants—particu-
larly in small states—and so is not worth the
eort, on the other hand, nding a contractor
that can provide the entire range of Medicaid
and Medicare services may not be feasible or
may require too much eort.
Medicaid Authorities
Medicaid authorities for MLTC have evolved con-
siderably since the early programs of the 1980s and
1990s. ALTCS and the rst generations of Minne-
sota’s Senior Health Options and Wisconsin’s Part-
nership Program all operated under §1115 waiv-
ers, which are intended to promote research and
demonstration initiatives that test new ideas. Since
then, additional statutory authorities have been en-
acted, and CMS has helped states to assess whether
or not they need the §1115 authority to achieve
their goals. The result has been a marked movement
away from §1115 waivers.
10
Medicaid authorities that states may consider alone
or in combination are described below and their key
features are summarized in Table 8-1 (on the next
page). The authority or combination of authorities
that a state selects depends primarily on the pro-
gram features desired. Ideally, the choices made will
enable the desired program features with the least

217
Chapter 8: Medicaid Authorities for Delivering Home and Community Services through Risk-Based Managed Care Systems
administrative burden. The major program features
are listed in the rst column of Table 8-1 and are
discussed below.
• Managed care authority is used to pay a lim-
ited number of contractors to serve a popula-
tion on a capitated basis. The con tractor is
responsible for a group of services, which it
oers through a network of pro viders. States
may select contractors through a competitive
process, or may simply set the participation
requirements and contract with any organiza-
tion meeting the requirements.
• Selective contracting allows the state to
limit the number of participating providers.
This feature diers from the normal practice
in Medicaid, in which provider qualica tions
are set by the state and all providers who meet
them may participate as Medicaid providers.
• Mandatory enrollment into Medicaid man-
aged long-term care requires a §1115 or a
§1915(b) waiver. Mandatory enrollment is
also possible under the §1932(a) and §1937
authorities, except for dually eligible per sons.
Because persons dually eligible are at risk for
needing long-term care, exempting them from
mandatory enrollment makes these authories
impractical for mandatory MLTC. Regardless of
the authority used, dually eligible persons may
never be subject to mandatory enrollment for
Medicare ser vices.
• HCBS beyond the State Plan, institutional
level-of-care requirement, and waiver of
comparability. Traditionally, states have pro-
vided a wide range of home and com munity
services—including those not available under
the Medicaid State Plan, such as environmen-
tal modications—on a fee-for-service basis
in a §1915(c) waiver program. States can oer
a capitated MLTC program using a §1915(c)
waiver in com-bination with a managed
care authority. However, the program will be
limited to individuals who meet the state’s
institutional level-of-care criteria.
With the passage of the Decit Reduction
Act of 2005 (DRA-2005)—as amended by the
Patient Protection and Aordable Care Act
of 2010 (hereafter called the Aordable Care
Act)—states may now oer HCBS under their
State Plan through the §1915(i) authority, free-
ing them from the requirement to use institu-
tional level-of-care criteria—unless the state
uses the 300 percent of SSI income eligibility
criteria. (See Chapter 4 for more information
about this authority.)
• Limit geographically. Except for the §1915(i)
authority, all of the authorities listed in Table
8-1 allow a state to limit a program geographi-
cally, referred to as waiving Medicaid’s “state-
wideness” requirement. States often do so to
gradually phase-in a pro-gram or because a
limited supply of MLTC contractors in rural
areas makes it impractical to oer a program
except in highly populated areas.
• HCBS nancial eligibility. In general, a state
may not deviate from the nancial eligibil-
ity criteria included in its State Plan, with the
exception of institutional nancial eligibility
criteria, an option states may elect to use for
institutional services and for §1915(c) waiv-ers.
Institutional nancial eligibility criteria include
(1)the special income rule, which allows states
to expand nancial eligibility to cover individu-
als in institutions (and §1915(c) waivers) who
have incomes up to 300 percent of the Federal
SSI benet level; (2)the ap-plication of spousal
impoverishment rules; (3)non-deeming of pa-
rental income for de-pendent children living at
home; and (4)var-ious exclusions from count-
able income (such as a home maintenance
allowance) in the determination of nancial
eligibility for home and community services.
This option to use 300 percent of the Federal
SSI benet to determine nancial eligibility is
also possible with a §1115 waiver, in a PACE
program under §1934, and with the §1915(i)
authority. However, if a state uses the special
income rule in its §1915(i) program, then par-
ticipants must meet institutional level-of-care
criteria. It is not possible to use institu-tional
nancial eligibility criteria under a §1915(b)
waiver or under the §1915(a) sta tutory author-
ity alone.
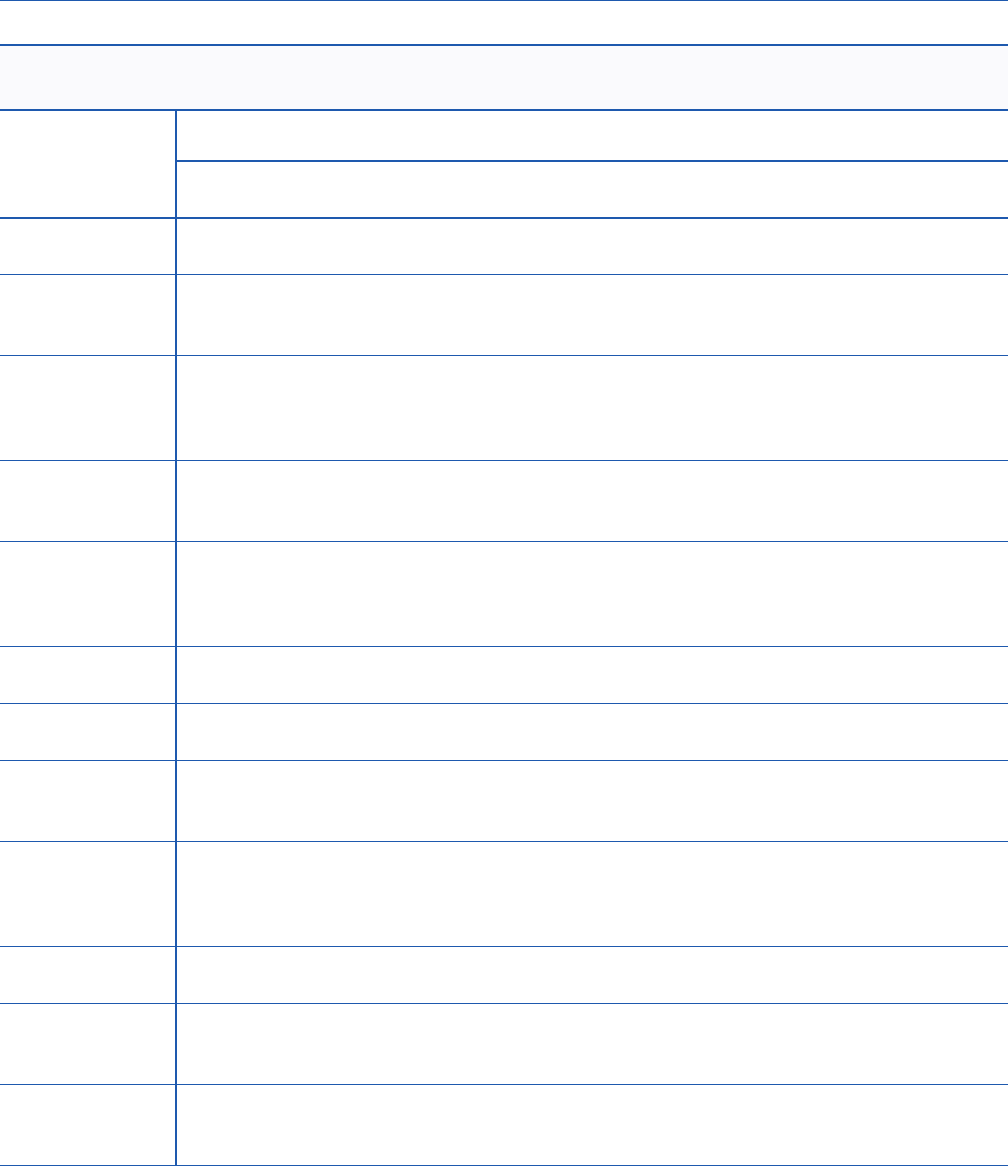
218 Understanding Medicaid Home and Community Services: A Primer
Table 8-1. Features of Medicaid Authorities That May Be Employed in
Managed Long-Term Care Programs
Features
Waivers Statutory Authority
§1115 §1915(b) §1915(c) §1915(a)
§1915(i)
(ACA)
§1932(a)
(BBA)
§1934
(BBA)
Managed care
3 3 3 3
PACE model
only
Selective
contracting
allowed
3 3 3 3
Mandatory
enrollment
3 3
Yes, but not
for dually
eligible
persons
Oer HCBS
beyond State
Plan
3 3 3 3
Institutional
level-of-care
requirement
3
Only if state
uses the
300% of SSI
income rule
3
Waive
comparability
3 3 3 3 3 3
Limit
geographically
3 3 3 3 3
Expand HCBS
nancial
eligibility
3 3 3 3
Budget and cost
requirements
Budget
neutral
Cost
eective
Cost neutral
Less than
upper
payment
level
Includes
Medicare
3
State Plan
amendment
required
3 3 3
Renewal
requirement
Usually
every 5
years
2 years 5 years None —1 None None
ACA = The Aordable Care Act; BBA = Balanced Budget Act.
1
If a state’s §1915(i) program targets a specic population, the State Plan amendment will only be approved for 5 years,
with the option for the state to renew for additional 5 year periods if CMS determines, prior to the beginning of the re-
newal period, that (1) the state met Federal and state requirements and (2) the state’s monitoring is in accordance with
the Quality Improvement Strategy in the state’s approved State Plan Amendment.

219
Chapter 8: Medicaid Authorities for Delivering Home and Community Services through Risk-Based Managed Care Systems
• Budget and cost requirements are important
when selecting an authority for implementing
an MLTC program, especially a §1115 wai ver.
The test for a §1115 waiver demonstra tion pro-
gram is that it be budget neutral, which means
that the total costs of the pro gram can not
exceed what they would have been under the
state’s regular Medicaid pro gram. Because the
state needs to stay within a total expenditure
cap, if enrollment is greater than projected, the
state is at risk for any additional costs. A state
may manage this risk by capping enrollment,
but may not want to do so if the policy objec-
tive is to expand coverage.
11
Section 1915(b) waivers require cost eect-ive-
ness, which applies to the average per-person
costs, which may not exceed the average per
person costs of the comparable fee-for-service
group. These costs must be calculated in an
actuarially sound manner, based on actual ex-
penditures in a base year. A state is at risk if av-
erage per person costs exceed fee-for-service
costs, but not for unanticipated enrollment of
additional per-sons.
12
Section 1915(c) waivers require cost neu-
trality, which means the average per person
cost for waiver services may be no greater than
the average cost of the institutional serv ices
that the waiver services are an alternative to,
determined on a per capita basis or in the
aggregate. The budget requirement for PACE
sites under §1934 is similar to that for §1915(c).
It requires that the cost of PACE services must
be less than the upper payment limit—dened
as the average amount that would have been
spent on a comparable pop ulation in fee-for-
service arangements.
13
Fi nally, if proposing a
benchmark plan under §1937, a state must
demonstrate that the proposed plan is actuari-
ally equivalent to the selected benchmark.
• Renewal requirements. When determining
which authority to use, states may want to
consider the associated administrative bur-
dens of each option. A clear advantage of
using the §1932(a) and §1934 authorities is
that once approved, they become a perma-
nent feature of the state’s Medicaid program
unless subsequently altered by the state. Sec-
tion 1915(b) waivers are approved for 2-year
per-iods and may be renewed for up to 2 years.
Section 1915(c) waivers are approved initially
for a 3-year period with a 5-year renewal per-
iod. Section 1115 demonstration programs are
initially approved for a 5-year period and can
be renewed for a 3-year period. Section 1915(i)
benets that include targeted pop-ulations
can only be approved for a 5-year period, with
the option to renew for additional 5-year peri-
ods.
Under a new provision of the Aordable Care
Act, the Secretary of HHS may allow waiver
programs for individuals who are dually eli-
gible to be approved for an initial period of up
to 5 years and renewed for up to 5 years, at the
State’s request.
14
CMS will be issuing guidance
on this provision in the near future.
The features a state wishes to include in its MLTC
program should drive the state’s decision about
what specic authorities to use. In general, a state
wants to achieve the greatest number of desired
features with the least administrative burden. A
summary of each authority follows.
Section 1115 Waivers
Of all the Medicaid authorities that states can use to
oer MLTC, §1115 waivers oer the greatest ex-
ibility. However, they also have the most rigorous
approval criteria and generally take longer to obtain
than other waivers. Section 1115 allows the Secre-
tary of Health and Human Services to waive any of
the requirements of §1902 of the Social Security Act
for purposes of researching innovative approaches
to delivering Medicaid benets and services, includ-
ing both managed care and fee-for-service innova-
tions. Section 1902 includes the basic requirements
for operating a Medicaid program, making the
§1115 waiver the most comprehensive available.
To be approved, a §1115 demonstration must test
a new idea to improve the Medicaid program. The
budget test is more rigorous than those for other
waivers and the Federal Oce of Management
and Budget reviews for budget neutrality. There is
220 Understanding Medicaid Home and Community Services: A Primer
no limit on the amount of time CMS may take to
review the application. In short, this waiver can do
the most, but can only be used to test a true innova-
tion. See Table 8-2 for an example of the use of this
authority.
Concurrent §1915(b) and
§1915(c) Waivers
Section 1915(b) waivers are used to create manda-
tory managed care programs. They may not be used
to oer benets that are not included in the Med-
icaid State Plan, nor may they be used to expand
nancial eligibility for HCBS beyond State Plan eli-
gibility levels. An exception is that a managed care
plan can oer expanded or additional services with
program savings. Section 1915(b) waivers provide
the opportunity for states to oer to enrollees ad-
ditional services paid for through savings achieved
under the waiver. In order to provide these §1915(b)
(3) services, CMS must approve a state’s request for
authority under subsection 1915(b)(3) in conjunc-
tion with either subsection 1915(b)(1) and/or (b)
(4).
16
Section 1915(c) waivers do not allow capitated
managed care arrangements, but have been used
since the 1980s to provide home and community
services not covered in the Medicaid State Plan.
Thus, concurrent use of §1915(b) and §1915(c) waiv-
ers allows states to cover both State Plan services
(e.g., home health, personal care, and rehabilitative
services) and non-State Plan home and community
services (e.g. homemaker services, adult day health
services, and assistive technology) in their man-
aged care programs’ capitation rate for individuals
eligible for §1915(c) waivers. States may also include
home and community services in their §1915(b)
waivers as §1915(b)(3) services.
The §1915(c) authority also allows states to use
institutional nancial eligibility criteria, which, as
discussed above, expands income eligibility criteria
to 300 percent of the Federal SSI benet; applies
spousal impoverishment rules; does not deem
parental income for dependent children; and allows
exclusions from countable income when determin-
ing nancial eligibility for servi ces. By using these
two authorities concurrently, states can create an
MLTC program, as has New Mexico. See Table 8-3.
Table 8-2. Arizona Long-term Care System (ALTCS)
Start Date 1988–89
Target Group Older persons, persons with physical disabilities, or persons with intellectual or other develop-
mental disabilities, all of whom must be clinically certied to need an institutional level of care.
Enrollment is mandatory. However, dually eligible persons continue to receive their Medicare
benets through the fee-for-service system, a Medicare Advantage Plan, or a Special Needs Plan.
Service Area Statewide
Scope of
Medicaid
Capitation
All Medicaid services, including primary and acute health care, long-term care services (institu-
tional and HCBS), and behavioral services.
15
Authorities Section 1115 waiver. Arizona has operated its entire Medicaid program under a §1115 waiver
from its inception in 1982. ALTCS was truly experimental when it was implemented in 1988—no
state had undertaken any signicant MLTC, and Arizona was proposing it statewide on a manda-
tory basis. The population is similar to that served in §1915(c) waiver programs. If ALTCS were
proposed today, a §1915(b) and (c) waiver combination would likely be considered.
More information is available at: http://www.azahcccs.gov/reporting/default.aspx
221
Chapter 8: Medicaid Authorities for Delivering Home and Community Services through Risk-Based Managed Care Systems
Section 1915(a)
The §1915(a) authority allows states to create
voluntary managed care programs without a waiver
or a Medicaid State Plan amendment. It does not
allow selective contracting, which means that states
cannot engage in competitive procurement of con-
tractors under this authority. The state may, how-
ever, dene the contractors’ qualications and oer
contracts to all who meet them, and participating
contractors may limit specic providers when they
create their networks. This authority can also be
used to waive comparability and to limit a program
geographically.
This authority alone is not sucient to create an
MLTC initiative because without a concurrent
§1915(c) waiver or a §1915(i) State Plan benet, it
limits the state to oering existing State Plan ser-
vices and using regular State Medicaid Plan nancial
eligibility criteria. However, §1915(c) waiver services
can count as services oered under the State Plan.
17
Services not expressly contained in the approved
§1915(c) waiver or in the §1915(i) State Plan amend-
ment for which payment is made under the con-
tract, may be provided as “in lieu of” services at the
state’s election.
18
Thus, states that oer many long-term services
through their State Plan or existing §1915(c) waivers
may nd this authority adequate for establishing an
MLTC program—as does Pennsylvania, which uses
the §1915(a) authority to operate a program for
adults with autism. See Table 8-4 for an example of
the use of this authority.
Table 8-3. New Mexico Coordination of Long-Term Services (CoLTS)
Start Date 2008
Target Group Older persons and persons with physical disabilities. Enrollment is mandatory.
Service Area Statewide
Scope of Medicaid
Capitation
Most Medicaid services, including primary and acute health care and long-term care services
(institutional and HCBS). Behavioral services are carved out to a separate managed care organi-
zation.
Authorities Concurrent §1915(b) and (c) waivers. New Mexico is the latest state to implement an MLTC
program, and has used the (b)(c) combination to create a mandatory, statewide program that
includes primary and acute health care and long-term services in one package.
More information is available at: http://www.nmaging.state.nm.us/COLTS_overview.html.
Table 8-4. Pennsylvania Adult Community Autism Program (ACAP)
Start Date 2009
Target Group Adults (age 21+) with Autism Spectrum Disorder who require an Intermediate Care Facility (ICF)
level of services, but can live in a community setting. Enrollment is voluntary.
Service Area Four counties.
Scope of Medicaid
Capitation
Primary care, ICF level of services in the community, and behavioral services. Acute care and
pharmacy are carved out.
Authorities Section 1915(a) authority. Pennsylvania operates this program without waivers. Although the
§1915(a) authority does not authorize selective contracting, only one contractor to date has met
the required qualications and is the sole vendor.
More information is available at: http://www.dpw.state.pa.us/ServicesPrograms/Autism/.
222 Understanding Medicaid Home and Community Services: A Primer
Section 1932(a)
Section 1932(a) was enacted as part of the Balanced
Budget Act of 1997. As previously discussed, the
BBA recognized that Medicaid man aged care had
become the service delivery mode for more than
half of all Medicaid beneciaries by the late 1990s,
and made mandatory managed care a State Plan
option under certain conditions. Section 1932(a)
is basically the same as the §1915(a) authority
with the exception that it allows mandatory en-
rollment—except for dually eligible persons and
children with special needs. However, these popula-
tions can be included on a voluntary basis. It can be
used to create a man aged care plan for either health
care or long-term care or both.
See Table 8-5 for an example of a program that uses
§1932(a) in combination with a §1915(c) waiver and
Medicare Special Needs Plan authority to create a
voluntary MLTC program for dually eligible adults of
all ages with disabilities.
Table 8-5. Wisconsin Family Care Partnership (FC-P)
Start Date 1996
Target Group Older persons and persons under age 65 with physical disabilities who are clinically certied to
need institutional level of care. Enrollment is voluntary.
19
Service Area 16 counties, with expansion underway.
Scope of
Medicaid
Capitation
All Medicaid services, including primary and acute health care, long-term care services (HCBS
and institutional), and behavioral services. (Medicare services are also fully capitated in a sepa-
rate payment that FC-P receives from the Medicare program.)
Authorities Section 1915(c) waiver and §1932(a) State Plan amendment. Wisconsin borrowed from the PACE
model to create a program that includes all Medicaid and all Medicare services in one package
for dually eligible persons. (But FC-P does not require enrollees to be dually eligible.) Because
the program deviates substantially from PACE (e.g., it includes persons under 55 years of age),
it could not use the §1934 PACE authority. Instead, it combined a §1915(c) HCBS waiver with
the State Plan managed care option of §1932(a). Section 1932(a) is usually used for mandatory
managed care programs, but it can also be used with exempt populations (e.g., dually eligible
persons) on a voluntary basis. Medicare services are provided using the Medicare Special Needs
Plan authority.
More information is available at: http://dhs.wisconsin.gov/wipartnership/.
Section 1934
Section 1934 was also enacted as part of the BBA,
making PACE a Medicaid State Plan optional benet.
In combination with Medicare stat utory authority in
Title XVIII, this authority makes PACE a non-waiver
option for fully capitated Medicare and Medicaid
managed care for dually eligible persons. Enroll-
ment is voluntary. The major limitation is that the
authority applies specically to the PACE model and
may not be used to authorize an MLTC program that
does not adhere to the model. See Table 8-6 for a
description of PACE.

223
Chapter 8: Medicaid Authorities for Delivering Home and Community Services through Risk-Based Managed Care Systems
Table 8-6. Program of All-inclusive Care for the Elderly (PACE)
Start Date 1983 at On Lok in California; 1990 in replication sites.
Target
Group
Persons 55 or older who ae clinically certied to need a nursing facility level of care.
Service Area 72 PACE providers operate programs in 30 states, as of September 2009.
Scope of
Medicaid
Capitation
All Medicaid services, including primary and acute health care, long-term care services
(HCBS and institutional), and behavioral services. (Medicare services are also fully capitat-
ed in a separate payment that the PACE program receives from the Medicare program.)
Authorities Section 1934 State Plan amendment. After several years operating under a §1115 waiver,
the Balanced Budget Act of 1997 made PACE a State Plan option. The authority may only
be used to establish a PACE program, which is a specic model of care that features an In-
terdisciplinary Team, adult day health centers where members receive primary health care,
and sta model care networks that include physicians who work for the PACE provider
organization. Parallel Medicare authority is contained in Title XVIII of the Act at §1894.
For more information: http://www.npaonline.org/website/article.asp?id=4/.
Medicare Special Needs Plans
Because such a high proportion of individuals who
need long-term services are dually eligible for Med-
icaid and Medicare, some states oering MLTC have
contracted with Medicare Special Needs Plans to
create integrated programs for dually eligible per-
sons. Special Needs Plans are authorized under the
Medicare Advantage man aged care program. Unlike
regular Medicare Advantage plans, Special Needs
Plans may limit enrollment to one of three autho-
rized groups: dually eligible persons, beneciaries
requiring institutional level of care, or beneciaries
with specied chronic conditions.
20
A state uses the appropriate Medicaid authorities to
craft a managed Medicaid program and contracts
with a Special Needs Plan, which has a separate con-
tract with CMS to deliver Medicare managed care
services. The two are combined at the plan level to
create an integrated Medicaid and Medicare pro-
gram for dually eligible persons. Because no author-
ity exists for mandatory Medicare enrollment, inte-
grated plans must be voluntary. See Table 8-7 for an
example of contracting with Special Needs Plans to
create integrated Medicare-Medicaid programs.
As noted above, §1934, which authorizes PACE
programs, is the other authority that may be used to
oer integrated Medicare-Medicaid programs.
224 Understanding Medicaid Home and Community Services: A Primer
Section 1915(i)
Section 1915(i) was enacted as part of the DRA of
2005 and amended by the Aordable Care Act.
This authority allows states to oer HCBS under
their Medicaid State Plan to individuals eligible for
Medicaid under an eligibility group covered by the
State Plan. Unlike the §1915(c) waiver authority,
the §1915(i) authority does not tie the provision of
HCBS to people who require an institutional level
of care, unless the state uses the 300 percent of SSI
income rule to determine nancial eligibility. This
authority also does not by itself allow managed care
approaches, and would need to be used in com-
bination with another authority to implement an
MLTC program.
21
All Quality and Other Requirements of Each
Authority Must Be Met
For many states, combining two waivers or a waiver
and a State Plan amendment will be an eective
way to create the program desired while avoiding
the greater burdens associated with a §1115 waiver.
However, states must be prepared to meet the
requirements of each authority they invoke (e.g.,
a program that combines managed care authority
and HCBS authority must meet all the requirements
of both). In addition, if partnering with a Medicare
Special Needs Plan to create a program for dually
eligible persons, the Special Needs Plan will be ac-
countable to CMS for all Medicare managed care
requirements.
In the area of quality, for example, a program under
the authority of §1915(a), §1915(b), or §1932(a)
must meet continuous quality improvement re-
quirements for Medicaid managed care, including
performance improvement projects for health sta-
tus and outcomes. The state must also provide for
an External Quality Review Organization to evaluate
outcomes and access to care. In addition, for the
rst two renewals of a §1915(b) waiver, the state
must provide to CMS an independent assessment
on access and quality requirements. Under §1915(c),
states must meet CMS quality requirements in
several areas, including safeguarding waiver partici-
pants’ health and welfare.
22
(See the Appendix for an
overview of CMS requirements for quality manage-
ment and improvement systems.)
Table 8-7. Minnesota Senior Health Options
Start Date 1997
Target
Group
Older persons (65+) who are dually eligible for Medicaid and Medicare, whether or not
they have long-term care needs. Enrollment is voluntary.
Service Area Nearly statewide
Scope of
Medicaid
Capitation
All Medicaid services, including primary and acute health care, HCBS, and up to 180 days
of institutional long-term care services. Behavioral services are also included. (Medicare
services are fully capitated in a separate payment to Minnesota Senior Health Options
from the Medicare program.)
Authorities Section1915(a) authority and §1915(c) waiver. When this program began in 1997, it
was an experimental model to combine Medicaid and Medicare and integrate nancing
for primary and acute health services and long-term care services under a §1115 waiver.
By renewal time, other states had developed combination approaches without a §1115
waiver and its dicult budget test, and Minnesota agreed to change to the (a)(c) combina-
tion at that time. Medicare authority also shifted over time, from special payment author-
ity and variances under the Medicare statute, to Medicare Special Needs Plan authority.
More information is available at: http://www.dhs.state.mn.us/main/idcplg?IdcService=GET_DYNAMIC_CONVE
RSION&dDocName=id_006271&RevisionSelectionMethod=LatestReleased
225
Chapter 8: Medicaid Authorities for Delivering Home and Community Services through Risk-Based Managed Care Systems
Resources
Since the Primer was rst published in 2000, numerous reports and other resources have become available
on the Internet. This section includes key resources relevant to Medicaid managed care authorities. Most of
the publications cite additional resources and the websites also have links to other sources of information.
Publications
Bella, M., and Palmer, L. (2009). Supporting Integrated Care for Dual Eligibles: Policy Options. Baltimore,
MD: Center for Health Care Strategies.
This policy brief addresses opportunities for integrating care for this high-cost, high-need population. The
brief outlines the rationale for integrating care for dually eligible persons, reasons why integration has been
slow to progress, and emerging vehicles to accelerate the adoption of fully integrated care models. A compan-
ion resource paper provides additional details on promising integrated care models and the challenges and
opportunities for supporting integrated approaches.
Available at http://www.chcs.org/publications3960/publications_show.htm?doc_id=982564
CMS (2009). Providing Long Term Services and Supports in a Managed Care Delivery System. Enrollment
Authorities and Rate Setting Techniques: Strategies States May Employ to Oer Man aged HCBS, CMS Re-
view Processes and Quality Requirements.
CMS has developed a brief technical assistance paper that outlines the enrollment authorities that states may
consider when designing managed HCBS programs, the CMS review and approval process for each, and rate
setting techniques that may be useful. This resource is the product of a CMS central and regional workgroup
with expertise in managed care and HCBS, which reects the progressive eorts underway in a number of
states.
Available at http://www.cms.hhs.gov/CommunityServices/Downloads/ManagedLTSS.pdf
CMS State Medicaid Director Letter. May 20, 2010. Community Living Initiative.
This letter provides some basic information on the Patient Protection and Aordable Care Act, P.L. 111-148,
enacted March 23, 2010, and the Health Care and Education Reconciliation Act of 2010, P.L. 111-152, enacted
March 30, 2010, (together referred to as the Aordable Care Act), and includes a link to the online technical as-
sistance guide entitled Long Term Services and Supports in a Managed Care Delivery System.
Available at http://www.cms.gov/smdl/downloads/SMD10008.pdf
226 Understanding Medicaid Home and Community Services: A Primer
Saucier, P., Kasten, J., and Burwell, B. (2009). Federal Authority for Medicare Special Needs Plans and
Their Relationship to State Medicaid Programs. Prepared by Thomson Reuters for the U.S. Department of
Health and Human Services, Oce of the Assistant Secretary for Planning and Evaluation, Oce of Dis-
ability, Aging and Long-Term Care Policy.
This brief, the rst in a series of three, reviews the history and current status of the Federal Medicare Special
Needs Plan authority, with particular attention to provisions of interest to state Medicaid programs.
Available at http://aspe.hhs.gov/daltcp/reports/2009/leghist.htm
Saucier, P., Burwell, B., and Gerst, K. (2005). The Past, Present and Future of Managed Long-Term Care.
Prepared by Thomson Reuters and the University of Southern Maine Muskie School for the U.S. Depart-
ment of Health and Human Services, Oce of the Assistant Secretary for Planning and Evaluation, Of-
ce of Disability, Aging and Long-Term Care Policy.
The focus of this study is Medicaid-nanced long-term care, though the discussion includes Medicare since
most Medicaid long-term care beneciaries are dually eligible. Thus the study includes both Medicaid-only
programs and integrated programs that manage both Medicaid and Medicare benets. The study focuses
on older persons and persons with physical disabilities, and excludes programs that are primarily targeted to
persons with developmental disabilities or serious and persistent mental illness.
Available at http://aspe.hhs.gov/daltcp/reports/mltc.htm#section1
Saucier, P., and Fox-Grage, W. (2005). Medicaid Managed Long-Term Care. Washington, DC: AARP, Public
Policy Institute.
This issue brief reviews the limited but important experience of states that had implemented Medicaid man-
aged long-term care programs at the time of publication, identies key policy issues, and assesses the likeli-
hood of future growth in these programs.
Available at http://www.aarp.org/health/medicare-insurance/info-2005/ib79_mmltc.html
227
Chapter 8: Medicaid Authorities for Delivering Home and Community Services through Risk-Based Managed Care Systems
Websites
Centers for Medicare & Medicaid Services
The following site provides information about combining §1915(b) and §1915(c) authorities to provide a con-
tinuum of services to disabled and/or elderly populations. By combining these authorities, states can provide
long-term care services in a managed care environment or use a limited pool of providers.
Web address: http://www.cms.hhs.gov/MedicaidStWaivProgDemoPGI/06_Combined1915bc.asp
The following site provides a list of resources that are currently available to provide information and assistance
when developing integrated Medicare and Medicaid models of care.
Web address: http://www.cms.hhs.gov/IntegratedCareInt/2_Integrated_Care_Roadmap.asp
The following site provides an Overview of Special Needs Plans and includes several downloadable resources.
Web address: http://www.cms.hhs.gov/specialneedsplans/
National PACE Association
The National PACE Association works with CMS sta and members of Congress who work on policy issues
aecting PACE organizations. Because PACE organizations are innovative programs that work with both the
Medicare and Medicaid programs, the model has its own regulations that govern its operation. Information
about Federal and state policy can be found at the following sites, respectively.
Web address: http://www.npaonline.org/website/article.asp?id=730and http://www.npaonline.org/website/
article.asp?id=731
228 Understanding Medicaid Home and Community Services: A Primer
Center for Health Care Strategies (CHCS)
The Center for Health Care Strategies is a nonprot health policy resource center dedicated to improving
health care quality for low-income children and adults, people with chronic illnesses and disabilities, frail
elders, and racially and ethnically diverse populations experiencing disparities in care. CHCS works with state
and Federal agencies, health plans, providers, and consumer groups to develop innovative programs that
better serve people with complex and high-cost health care needs. The following website includes numerous
publications and other resources about dually eligible persons and integrated care.
Web address: http://www.chcs.org/info-url_nocat5108/info-url_nocat_list.htm?attrib_id=8408
In particular, the website has two links that are directly relevant to this chapter:
http://www.chcs.org/publications3960/publications_show.htm?doc_id=747565
This webinar explored progress that states have made in integrating care for dually eligible populations via
Special Needs Plans, the challenges for integrating care, as well as new non-Special Needs Plan alternatives for
states to consider.
http://www.chcs.org/publications3960/publications_show.htm?doc_id=504045
Download resources from this webinar, which featured state and health plan best practices for managing the
long-term care of Medicaid beneciaries, and integrating acute and long-term care for adults solely covered
by Medicaid or dually eligible for Medicaid and Medicare.

229
Chapter 8: Medicaid Authorities for Delivering Home and Community Services through Risk-Based Managed Care Systems
Endnotes: Citations, Additional Information,
and Web Addresses
1
Paul Saucier is the author of this chapter.
2
Categorical groups eligible for SSI include those age 65 or older, and children and adults under age 65
who meet SSI disability criteria.
3
Kaye, N. (2005). Medicaid Managed Care: Looking Forward, Looking Back. Portland, ME: National Acad-
emy for State Health Policy.
4
Saucier, P., Burwell, B., and Gerst, K. (2005). The Past, Present and Future of Managed Long-Term Care.
Prepared by Thomson Reuters and the University of Southern Maine Muskie School for the U.S. De-
partment of Health and Human Services, Oce of the Assistant Secretary for Planning and Evaluation,
Oce of Disability, Aging, and Long-Term Care Policy. Available at http://aspe.hhs.gov/daltcp/reports/
mltc.htm#section1.
5
CMS. National Summary of Medicaid Managed Care Programs and Enrollment as of June 30, 2008.
Available at http://www.cms.hhs.gov/MedicaidDataSourcesGenInfo/downloads/08Trends508.pdf.
6
CMS. Number of Managed Care Entity Enrollees by State as of June 30, 2008. Available at http://www.
cms.hhs.gov/MedicaidDataSourcesGenInfo/downloads/08MCE-%20Enrolleesf508.pdf.
7
Kaye, N. (2005), op. cit.
8
The 11 states operating MLTC outside of PACE are Arizona, California, Florida, Hawai’i, Massachusetts,
Minnesota, New Mexico, New York, Texas, Washington, and Wisconsin. Tennessee has received Federal
permission to implement an initiative scheduled to begin in 2010.
9
Evaluations of early MLTC programs have found consistently that hospital and nursing home use de-
creases and community services increase. For a review of the literature, see Saucier, P., Burwell, B., and
Gerst, K. (2005), op. cit.
10
Saucier, P., and Fox-Grage, W. (2005). Medicaid Managed Long-Term Care. Washington, DC: AARP,
Public Policy Institute. Available at http://www.aarp.org/health/medicare-insurance/info-2005/ib79_
mmltc.html.
11
If a state has made the policy decision to cover persons who meet certain nancial or other criteria,
capping enrollment could upset advocates and raise valid issues related to equity. If a state can get
Federal nancial participation for all eligible persons, they would of course prefer this, but because
the Oce of Management and Budget puts an overall cap on expenditures, the state must either cap
enrollment or pay costs only with state dollars once the expenditure limit is reached.
12
The requirements for a §1115 waiver can lead to enrollment caps, which are politically dicult and can
strain relations with contractors. Capping per person costs can be done easily by setting the capitation
rate to not exceed the per person cap.

230 Understanding Medicaid Home and Community Services: A Primer
13
For more on Medicaid rate setting in PACE, see National PACE Association (2009). Pace Medicaid Rate-
Setting: Issues and Considerations for States and PACE Organizations. Available at http://www.npaon-
line.org/website/navdispatch.asp?id=2871.
14
The Aordable Care Act amended §1915(h) of the Social Security Act.
15
Behavioral services include mental health and substance abuse services.
16
CMS. (2009). Providing Long Term Services and Supports in a Managed Care Delivery System. Enroll-
ment Authorities and Rate Setting Techniques: Strategies States May Employ to Oer Managed HCBS,
CMS Review Processes and Quality Requirements. Available at http://www.cms.hhs.gov/Community-
Services/Downloads/ManagedLTSS.pdf.
17
Ibid. CMS may consider the inclusion of HCBS in a stand-alone §1915(a) contract in those cases where
the state operates an approved section §1915(c) waiver or §1915(i) State Plan benet for the same
population served through the contract, in the same geographic region as the contract, containing
the same services oered through the contract, and the costs of such services may be included in
contract payments. These HCBS would be expressly contained in the managed care contract, and the
individual need not be enrolled in a §1915(c) HCBS waiver or be receiving services through a §1915(i)
HCBS State Plan program. Because this is a voluntary vehicle, an individual must be able to have the
option to receive the services through another Medicaid approved authority in the state (i.e., State
Plan or HCBS waiver).
18
Ibid.
19
Adults age 17 years, 9 months and older are eligible.
20
For an overview of the Federal Special Needs Plan authority, see Saucier, P., Kasten, J., and Burwell, B.
(2009). Federal Authority for Medicare Special Needs Plans and their Relationship to State Medicaid
Programs. Prepared by Thomson Reuters for the U.S. Department of Health and Human Services, Of-
ce of the Assistant Secretary for Planning and Evaluation, Oce of Disability, Aging and Long-Term
Care Policy. Available at http://aspe.hhs.gov/daltcp/reports/2009/leghist.htm.
21
To date, there are no known MLTC programs invoking this authority.
22
42 CFR 441.302. Available at http://law.justia.com:80/us/cfr/title42/42-3.0.1.1.10.7.html.

Appendix: Medicaid HCBS Quality
231
Guide to Appendix
Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .233
An Evidence-Based Approach to Quality Monitoring . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .233
Continuous Quality Improvement (CQI) Model . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .234
Continuous Quality Improvement: Design . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .234
Continuous Quality Improvement: Discovery . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .236
Crafting Performance Measures . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .236
Continuous Quality Improvement: Remediation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .240
Continuous Quality Improvement: Improvement . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .242
Beyond Assurance-Based CQI. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .244
The CMS Review Process . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .244
Technical Assistance for Medicaid HCBS Quality . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .245
Resources. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .246
Endnotes: Citations, Additional Information, and Web Addresses . . . . . . . . . . . . . . . . . . . . . . .248

233
Appendix: Medicaid HCBS Quality
Appendix
Medicaid HCBS Quality
Introduction
Under Federal statute, the Centers for Medicare & Medicaid Services (CMS) have the authority to oversee and
regulate states’ approaches to quality assurance for Section (§)1915(c) home and community-based services
(HCBS) waiver programs (hereafter called HCBS waiver programs). Over the last 10 years, CMS has mounted a
vigorous initiative to promote and enhance quality oversight of HCBS waiver programs, an initiative that has
required changes by the states and CMS.
Until 2004, Federal oversight of HCBS waiver program consisted of periodic reviews focusing on whether pro-
grammatic requirements had been met. During this period, CMS did not collect representative data on waiver
system performance, nor did it require the states to collect such information for use in quality monitoring and
improvement activities. Moreover, there was appreciable variation in how CMS Regional Oces conducted
quality reviews.
A major impetus for increased Federal attention to quality in the HCBS waiver programs was a 2003 Govern-
ment Accountability Oce (GAO) report.
The report cited as problematic the minimal information required in the waiver application about a state’s ap-
proach to monitoring quality, as well as the absence of a minimum level of routine reporting from the states to
CMS. The GAO urged greater oversight by CMS and the provision of increased guidance to the states on waiver
monitoring practices.
An Evidence-Based Approach to Quality Monitoring
In response to the GAO report, CMS designed and adopted an evidence-based approach to HCBS waiver
program quality. The evidence-based approach is premised on the expectation that states have rst-line
responsibility for program monitoring to ensure the waiver operates as it was designed (i.e., as specied in the
approved waiver application) and that program participants’ health and welfare are safeguarded. States, on a
periodic basis, must provide CMS with evidence that the program is indeed operating as specied in the ap-
proved waiver and that participants’ health and welfare are safeguarded. The evidence CMS requires is related
to the six statutory assurances that states make to CMS as a condition of approval of a waiver. CMS’s role is
to review the evidence the state submits, along with other information about the waiver’s performance, and
render a determination about the waiver’s compliance with the Federal assurances.
234 Understanding Medicaid Home and Community Services: A Primer
Continuous Quality
Improvement (CQI) Model
CMS’s evidenced-based approach, while new to the
Medicaid HCBS enterprise, is based on a well-es-
tablished management tool known as Continuous
Quality Improvement—or CQI. The CQI concept is
generally credited to W. Edwards Deming, a stat-
istician who pioneered this approach in his work
with manufacturers in Japan in the late 1940s. At
the heart of the CQI model is the use of empirical
information—that is, evidence—to drive continu-
ous, cyclical improvement. CMS has embodied the
CQI principles in its Design, Discovery, Remediation,
Improvement (DDRI) model. The DDRI model has
been the operative framework for HCBS waivers
since the early 2000s and is the common vocabu-
lary that links CMS’s expectations and state quality
eorts. CQI is best envisioned as a cyclical process,
one component feeding into the next.
Figure 1. The DDRI Model
It is CMS’s expectation that Medicaid HCBS pro-
grams embrace the CQI approach and nurture a
culture of quality improvement.
Continuous Quality Improvement:
Design
“Design” refers to a state’s plan for how it will moni-
tor a waiver program and make improvements
when systemic problems are detected. States must
describe this plan in the waiver application. In 2005,
CMS issued a new waiver application format, which
elicits specic information about a state’s design of
its quality monitoring and improvement strategy.
�
In the waiver application, a state must describe how
it will “discover” when the assurances have not been
met, its plans for monitoring whether the individual
problems it uncovers are “remediated” or xed, and
how it will engage in system “improvement” activi-
ties when it discovers that there are systemic prob-
lems responsible for an accumulation of individual
problems. A state’s CQI design must be organized
around the Federal assurances, described in Table 1.
Each assurance embodies more than one program-
matic expectation. In the waiver application, CMS
has articulated many subassurances—in order to
operationalize the six assurances in concrete terms
in accordance with CMS policy. CMS’s articulation of
subassurances seeks to ensure that states monitor
the aspects of the program CMS deems fundamen-
tal. A few examples of subassurances are presented
in Table 2. A full listing of the subassurances may be
found in the most current version of the §1915(c)
waiver
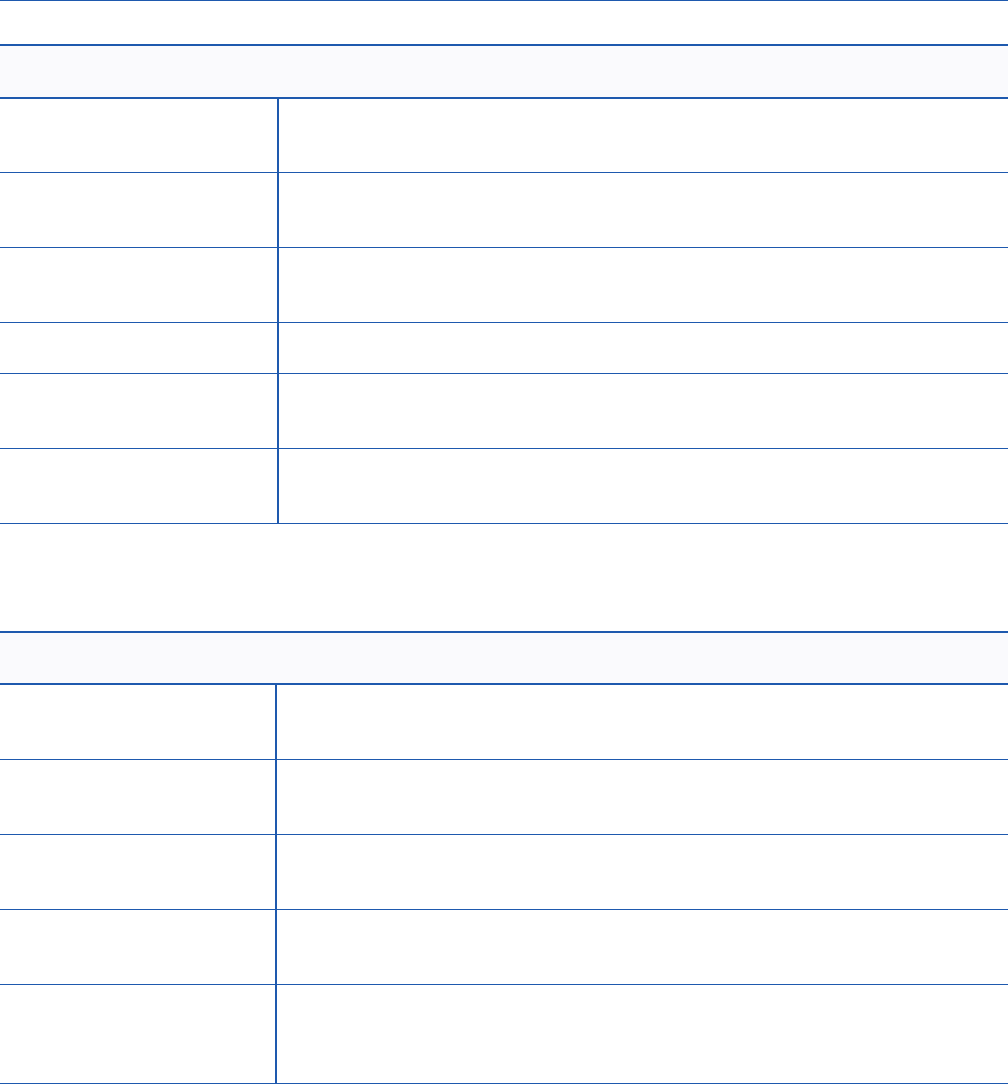
235
Appendix: Medicaid HCBS Quality
Table 1. Section 1915(c) Federal Assurances
Level of Care Persons enrolled in the waiver have needs consistent with an institutional level
of care.
Service Plan Participants have a service plan that is appropriate to their needs and prefer-
ences, and receive the services/supports specied in the service plan.
Provider
Qualications
Waiver providers are qualied to deliver services/supports.
Health and Welfare Participants’ health and welfare are safeguarded.
Financial
Accountability
Claims for waiver services are paid according to state payment methodologies
specied in the approved waiver.
Administrative
Authority
The state Medicaid agency is actively involved in the oversight of the waiver,
and is ultimately responsible for all facets of the waiver program.
Table 2. Examples of Subassurances (Version 3.5 of the §1915(c) Waiver Application)
Level of Care The levels of care of enrolled participants are reevaluated at least annually or as
specied in the approved waiver
Service Plan Service plans are updated/revised at least annually or when warranted by
changes in the waiver participant’s needs
Service Plan Services are delivered in accordance with the service plan, including in the
type, scope, amount, and frequency specied in the service plan.
Service Plan Participants are aorded choice: between waiver services and institutional care;
and between/among waiver services and providers.
Provider
Qualications
The state veries that providers initially and continually meet required licensure
and/or certication standards and adhere to other state standards prior to their
furnishing waiver services.
236 Understanding Medicaid Home and Community Services: A Primer
application. (See the Resources section of this ap-
pendix for a link to the application.)
Continuous Quality Improvement:
Discovery
Discovery refers to the monitoring process states
use to uncover deviations from program design in
a timely fashion. Discovery allows states to know
when program processes are not being followed
and when the assurances (subassurances) are
not being met. The discovery monitoring process
requires a state to establish performance measures
that enable it to assess whether—and the extent
to which—it is complying with each of the Federal
assurances.
In the waiver application, a state must specify one
or more performance measures for each subassur-
ance. In addition, it must provide information on
(1)the data source(s) for each performance mea-
sure; (2)how the representativeness of the data will
be ensured; (3)information on the party or parties
responsible for collecting, reviewing, and using the
data to manage the program; and (4)how frequent-
ly summary (i.e., aggregated) reports will be gener-
ated and reviewed.
Crafting Performance Measures
Most importantly, performance measures should
be actionable. Because their purpose is to help the
state evaluate its program and the health and wel-
fare of program participants, the measures should
be able to identify when a subassurance is not
being met, so that actions can be taken to bring the
program into compliance. Performance measures
must also meet four criteria (see Box).
Criteria for Crafting Performance
Measures
• Be measurable and stated as a metric
• Have face validity
• Be based on the correct unit of analysis
• Be representative
The rst criterion is that the performance measure
be measurable and stated as a metric. This means
that the performance measures must be able to
take on dierent values. States frequently make
the mistake of describing a process for monitor-
ing a subassurance, rather than focusing on the
outcome of the monitoring reported in the form of
a metric. Typically, assurance-based performance
measures are stated in the form of a percentage.
The performance measure data must also be able
to be aggregated across individual waiver partici-
pants, providers, or claims—depending on the unit
of analysis (discussed below). Aggregating perfor-
mance measure data allows the state to generate
reports on a specic aspect (subassurance) for the
program as a whole, assess the operation of the
program on that given aspect, and determine the
level of compliance.
A Performance Measure
Should Be a Metric
Acceptable: Percent of waiver participants
whose service plans were reviewed and updated
annually. (Outcome)
Unacceptable: The Division of Aging conducts
record reviews to assess whether services plans
of waiver participants are reviewed and updated
annually. (Process)
237
Appendix: Medicaid HCBS Quality
The second criterion is face validity, the property
of a performance measure that reects whether it
will indeed measure what it has been designed to
measure—in this case, a subassurance. To meet this
criterion, state sta have to ask the following: Does
the performance measure truly capture and mea-
sure the essence of a specic subassurance? “On
the face of it” does it track with the subassurance? A
performance measure with face validity will enable
a state to monitor its performance on a given subas-
surance, and for CMS to judge the state’s demon-
stration of compliance with the
A Performance Measure Should Have
Face Validity
Service Plan Subassurance: Service plans
address all participants’ assessed needs (includ-
ing health and safety risk factors) and personal
goals, either by the provision of waiver services
or through other means.
Unacceptable: Mean risk fall score for waiver
participants.
• Metric, but lacks face validity.
• Does not tell you to what extent risks were
addressed in service plan.
• May be a good assessment item, but is not
a performance measure with face validity
for the subassurance.
Acceptable: Percent of participants’ service
plans that address their risk.
• Metric.
• Has face validity vis-à-vis the subassurance.
subassurance. If a performance measure lacks face
validity, the state runs the risk of collecting poten-
tially useless information, wasting resources, losing
the ability to monitor one aspect of its program,
and not demonstrating compliance to CMS. States
should be careful to not use performance measures
that are stated as a metric but are lacking face valid-
ity vis-à-vis a given subassurance.
The third criterion is the correct unit of analysis.
Choosing the correct unit of analysis for a perfor-
mance measure is crucial. The unit of analysis refers
to the group/entity which the performance mea-
sure references. Typically, the unit of analy sis for
Level of Care, Service Plan, and Health and Welfare
subassurances is the waiver participant; for Provider
Qualication subassurances it is providers, and for
Financial Accountability it is claims. Data for gener-
ating performance measures can come from several
sources (administrative data, claims data, reviews
of participants’ records, automated care coordina-
tion systems, critical incident data bases, mortality
reviews, etc.), and sometimes from a combination
of data sources. Whatever the data source, it is key
to make sure that the unit of analysis is appropriate
to the subassurance that the performance measure
will be used to monitor.
A Performance Measure (PM)
Should Use the Correct Unit of Analysis
Service Plan Subassurance: Service plans
are updated/revised at least annually.
Incorrect Unit of Analysis: Percent of Sup-
ports Coordination Agencies that updated/
revised annual service plans on time.
• PM focuses on Supports Coordination
Agencies (provider) rather than waiver
participants.
• May be a more appropriate measure for a
Provider Qualications PM.
Correct Unit of Analysis: Percent of waiver
participants who received an annual up-
dated/revised service plan.
The fourth criterion is representativeness. When
monitoring a waiver, CMS is interested in knowing
how the waiver as a whole is performing on any
given subassurance. If the performance measure
data are not representative of the waiver population
(or of providers or claims), neither the state nor CMS
can be condent that the resulting measure accu-
rately portrays the waiver’s performance.

238 Understanding Medicaid Home and Community Services: A Primer
By denition, the data for generating a performance
measure are representative if they derive from the
entire population (e.g., service plans of ALL waiver
participants, reviews of ALL providers, reports on
ALL claims). However, collecting data from the
entire population can be very costly—particularly
for larger waiver programs. Thus, performance
measures frequently are based on data taken from
a sample (i.e., a subset of the population). The
estimates derived from a sample can represent the
entire population, as long as random selection is
used in drawing the sample.
CMS expects performance measure data to be
representative because if not, then the state can-
not assert with condence that the data represent
the waiver as a whole, and CMS cannot conclude
compliance due to insucient evidence.
CMS elicits information about the state’s plan for
generating representative data for its performance
measures within the quality section of the waiver
application labeled “Sampling Approach.” These
sections require states to specify whether a perfor-
mance measure will be based on population data
or whether the state will use a sampling approach.
If the state opts for sampling, CMS does not require
the state to specify the size of the sample, but rather
asks the state to specify the sampling parameters
that will be used to determine sample size. CMS has
certain expectations about the values these param-
eters must take on for the resultant sample to be
considered representative (see Box.)
239
Appendix: Medicaid HCBS Quality
Using Sampling Parameters to Determine a Representative Sample
Three parameters must be set to determine sample size: (1)Condence Level, (2)Condence Interval (also called the Margin of Er-
ror), and (3)Distribution (of the variable) in the Population. CMS considers a sample to be suciently representative if the Con-
dence Level is .95 or larger and the Condence Interval (Margin of Error) is +/– 5 percent or less. A Condence Level of 95 percent
ensures that one can be 95 percent certain that the estimate derived from the sample is accurate. A Condence Interval of +/– 5
percent ensures that the actual population value is within +/– 5 percent points of the estimate provided by the sample. A Distribu-
tion value of .5 is always acceptable (discussed in more detail below.)
For most states, determining a credible sample size will involve using a sample size calculator. Many calculators may be found on-
line by searching the term “sample size calculator.” These calculators will prompt the user for values for Population Size, Condence
Level, and Condence Interval (Margin of Error).
Many calculators will not prompt the user for a value for the Distribution (of the variable) in the Population, but will assume a .5
value. The best calculators, however, will allow the user to specify the Distribution value. It is not possible here to delve into the
conceptual underpinnings of this parameter; suce it to say that under certain conditions states may vary this parameter (from
.5), thereby lowering the recommended sample size, and still have a sample that is considered large enough to be representative.
There is a rule of thumb states may follow in varying the Distribution parameter: If the state is drawing a sample for the rst time in
order to collect data for a performance measure(s), it must assume a 50-50 Distribution and use the .5 value.
However, if the state has collected data on a given performance measure(s) previously, and derived the estimate from the entire
population or a representative sample, they may alter the distribution to reect that previous experience. For example, in Year 1 of
data collection the state discovered that 90 percent of service plans addressed participants’ needs, but 10 percent did not. In Year
2, they would be justied in using a 90–10 split (.9 Distribution value) in the sample size calculator. To illustrate the dierence in
sample size that altering the Distribution can make, let us use the example of a waiver with 3,000 participants. With a Distribution
value of .5, the recommended sample size is 341, but with a Distribution of .9 (or .1, its reciprocal), the recommended sample is
133.
5
If a state can justify using a Distribution other than the standard .5, it can decrease sample size while simultaneously generating
performance measure estimates that are credible and representative.
One error states should avoid is simply choosing sample size based on a percentage of the population (e.g., 10 percent of all
waiver participants). This approach will often either yield a sample that is not large enough to deliver credible results or will specify
a sample that is larger than necessary. Sample size should always be calculated by specifying the sampling parameters discussed
above.
Sample Stratication. Sometimes states are interested in obtaining information on how various subgroups—or strata—are
performing. For example, a state may want to monitor the performance of care coordination agencies in their responsibility for
conducting timely annual level-of-care determination. So, the state decides to “stratify” its record review sample by care coordina-
tion agency. However, before doing so, states need to consider several implications of a stratication approach. First, if there is a
desire to compare subgroups, then it is important that the sample for each subgroup be large enough to be representative of each
subgroup. In general, the more subgroups, or strata, the larger the overall sample size will need to be. The state must balance its
need for information on subgroups with available resources.
Although CMS elicits information from states on the waiver application about stratication, stratication is not a CMS requirement;
it is entirely at the state’s discretion whether to stratify. However, if stratication is used, it is important that the data be “re-weight-
ed” so that they represent the entire population; a simple averaging of results from the various strata will not produce a valid
estimate.
6
A statistician or someone with expertise in sampling statistics should be consulted. Technical assistance is also available
from CMS as described later in this appendix.
When states use the same quality improvement strategy (QIS) across multiple waivers or across waivers and state-funded HCBS
programs (sometimes referred to as a “Global QIS”), they may be tempted to draw one sample for all the waivers and programs
combined. However, CMS requires that evidence be reported for each waiver separately, and that the samples for each waiver be
large enough, on their own, to be representative of a given waiver’s population/providers. In this context, one might hear the issue
referred to as “stratifying” by waiver. If the state wants to sample across multiple programs, it will have to stratify by program and
ensure that the sample size for each program is large enough to be representative.
240 Understanding Medicaid Home and Community Services: A Primer
Continuous Quality Improvement:
Remediation
The purpose of discovery activities is to identify
instances where the program is not operating as
intended and is out of compliance with the Federal
assurances. Discovery activities, however, are not an
end in themselves but rather (and most important-
ly) a means to identifying problems so that they can
be addressed. In the CQI waiver cycle this is called
Remediation. The focus of remediation is to address
and resolve all individual problems uncovered in
the course of discovery.
The rate of compliance is measured through the
performance measures as discussed above. CMS ex-
pects states to be in compliance with the statutory
assurances. If a performance measure indicates that
the state achieved less than 100 percent compli-
ance, the state must remediate all instances of non-
compliance discovered. While a state may not be in
compliance initially, it may come into compliance
by taking remedial actions. Compliance can occur
by appropriately addressing all detected problems.
It is clearly preferable, however, for the state to
achieve compliance by preventing problems in the
rst place (i.e., having a high level of performance
initially).
As states design their quality strategies they must
build in systematic mechanisms for addressing
problems as they are uncovered. In the waiver appli-
cation, states are required to specify these meth-
ods. States should have policies and procedures
describing (1)who is responsible for monitoring
remediation activities and verifying that problems
are appropriately addressed, (2)the explicit ex-
pectations for timeframes within which problems
should be resolved, and (3)what sanctions may be
imposed in the event that corrective action is not
taken by the responsible party. It is also important
that remediation methods be appropriate to the
problems uncovered. Corrective actions will dier
depending upon the assurance, subassurance, and/
or performance measure for which non-compliance
was discovered.
Like discovery evidence, states should also be able
to aggregate remediation evidence. The aggrega-
tion of remedial activities is a state’s way of sum-
marizing the types and numbers of actions taken in
response to non-compliance with regard to a given
performance measure. Aggregated data about
remediation actions, in the form of remediation re-
ports, provide the evidence CMS requires to ensure
that the state has addressed instances of non-com-
pliance. Remediation reports can also be used by
the state, along with discovery reports, to identify
and analyze trends related to non-compliance.
Table 3 illustrates what a summary discovery and
remediation report might look like for one level-of-
care subassurance. The discovery and remediation
reports are linked because the number and types
of remediation actions necessarily follow from the
instances of non-compliance uncovered through
the state’s discovery activities. In this example, over
the course of one calendar year, the state uncovered
30 instances where a reevaluation to determine the
level of care was not conducted on time (Discovery
Results).
241
Appendix: Medicaid HCBS Quality
Table 3. Fictitious State Waiver Quality Monitoring Report, Generated 1-1-2009
Period of Performance: January 1, 2008 through December 31, 2008
Performance Measure: Number and percent of waiver participants who received an annual re-determina-
tion of eligibility within 12 months of their initial level-of-care evaluation or within 12 months of their last
annual level-of-care re-determination.
Discovery Results
Compliance Rate Sample
Compliance
91% 300
Non-compliance 9%
30
Total
100% 330
Remediation Actions
Actions Number of Actions
Reevaluation conducted, still eligible 25
Reevaluation conducted, not eligible 4
Referred to state-funded program 4
Claims from period of ineligibility excluded from Federal Financial
Participation(FFP)
4
# of remediations completed in < 30 days 26
# of remediations completed in 31-60 days 2
# of remediations completed in > 60 1
Outstanding remediation actions 1*
Total instances of non-compliance addressed 29
* In a record review on 12/22/08, a person was discovered to be 35 days overdue for a re-determination. Due to the
holidays, the re-determination had not occurred at the time this report was generated.

242 Understanding Medicaid Home and Community Services: A Primer
Twenty-nine of the 30 instances were addressed
through the state conducting a reevaluation on
each tardy re-determination (Remediation Actions).
In 25 of the 30, the person was found to still be
eligible at reevaluation and thus no further action
was necessary. However, in 4 cases the person re-
evaluated was deemed ineligible for the waiver, and
in these instances the state took further actions to
refer these individuals to the state-funded program
and to ensure that no FFP was claimed for waiver
services provided during the period of ineligibility.
In this example, the state had a policy that all
remediation actions related to late level-of-care
re-determinations must be accomplished within 30
calendar days of discovery; as such, the state is also
tracking whether appropriate remedial actions are
taken within the specied timeframe. In addition,
the remediation report identies the number of
outstanding problems not addressed on the date
the report was generated.
The example provided in Table 3 is a summary
report for one year and might be the type of report
a state would submit to CMS as evidence. However,
the state should have a data system
capable of generating more frequent reports, to en-
able performance monitoring as the discovery and
remediation results come in. A key component of
a quality assurance system is the ability to discover
problems close to their occurrence, which then
enables a quick response—be it xing the original
problem or uncovering remediation actions that are
inappropriate and/or untimely.
Continuous Quality Improvement:
Improvement
Fixing individual problems as they occur is an es-
sential component of CQI, but if the same type of
problem occurs repeatedly, it would be helpful for
the state to step back and assess what systemic
causes might be responsible. Having determined
the potentially largest contributor(s) to the prob-
lem, the state is then in a position to develop an
intervention to prevent future occurrences of the
problem. Examining summary discovery and reme-
diation data over several months is a good way to
determine if there are trends indicating the need
to go beyond interventions to address individual
problems and initiate those that are more systemic
and would result in better performance.
While Remediation focuses on addressing individual
problems, Improvement focuses on making adjust-
ments to the system’s processes or procedures in
order to prevent or minimize future individual prob-
lems. When system improvements work, discovery
data improve.
Typically, the discovery metrics of the performance
measures enable the state to assess whether an
improvement action actually resulted in better per-
formance; for example, the state will conduct a “pre-
post” analysis using the performance measure data
to evaluate the impact of the improvement action.
The “pre” data is the performance on a measure(s)
prior to the implementation of the improvement
intervention, and the “post” data constitutes per-
formance on the same measure(s) in the months
following the intervention.
If the improvement action is eective, the state will
see improvement in the performance measures.
If improvement is not achieved after a reas onable
amount of time has passed (i.e., sucient time to
allow for full implementation of the improvement
action), the state needs to go back to the drawing
board and gure out why the improvement proj-
ect did not work. One reason why an intervention
might not be successful is because the intervention
really did not occur as it was designed (e.g., a newly
instituted procedure was not followed). The other
reason for failure is that the intervention was not
the right intervention. If a state does not get the
results anticipated, it needs to assess both possible
causes. In most instances, states are very astute
about targeting the right intervention, and more
often than not a new procedure has the intended
result.

243
Appendix: Medicaid HCBS Quality
Example of a Quality Improvement Project
A State was concerned that the compliance rate on its performance measure “Percent of service plans that address
participants’ risk” consistently hovered around an unacceptable 75 percent for several months. The State’s waiver
manual species that risks should be evaluated during an assessment and enumerates the various aspects of risk
(i.e., health risks, behavioral risks, cognitive risks, fragility of the informal support system, etc.). Yet, case managers’
practice did not always meet the State’s expectations as stated in the manual.
When the Quality Unit, as part of their quality monitoring, reviews participants’ service plans and discovers that
risk has not been addressed, the case manager is required to revise the service plan and then the Quality Unit must
follow-up to verify that the service plan has indeed been updated. Continually having to remed iate these individ-
ual instances of non-compliance are costly to the State (in addition to the lack of compliance possibly jeopardizing
the health and welfare of program participants).
To improve the situation, the State decided to recongure its assessment form by adding a risk assessment proto-
col that must be completed by the case manager during every assessment. After reviewing other states’ approach-
es to risk assessment, the Quality Unit and Program Operations sta developed its own protocol, piloted it with a
small group of case managers, and revised it based on the pilot’s ndings. Prior to rollout of the new Risk Assess-
ment Protocol, Program Operations sta conducted multiple training sessions in the use of the new protocol for
case managers and supervisory personnel throughout the State. They also assigned one of their sta as a “go to”
person to answer questions case managers might have when using the new protocol.
Because the Quality Unit conducts record reviews on an ongoing basis, it was able to assess the eect of the new
Risk Assessment Protocol. Three months after the new protocol was implemented, 86 percent of service plans
addressed risk, and after 6 months, the compliance rate was at 97 percent; but by month 12 it had fallen back to
90 percent. Upon investigation, the State determined that the decrease was attributed to new case managers who
had not received the initial training on the new protocol. In order to sustain a high compliance rate, the State is
exploring the development of an online training module that all new case managers must view, combined with
close supervision for their rst 3 months of employment.
While the State’s initial quality improvement project was successful, the success was not sustained. Thus, they con-
tinue to ne tune their training processes to achieve their goal of high compliance rates.
244 Understanding Medicaid Home and Community Services: A Primer
CMS expects states to engage in CQI activities,
especially if there is consistent non-compliance over
a period of several months. States are required to
specify in the waiver application the party respon-
sible for assessing the need for, prioritizing, and
implementing quality improvement activities, as
well as the state’s processes for conducting these
activities. They also are required to specify how they
will assess the impact of the changes they made
and whether they resulted in quality improvements.
See Box below for an example of a quality improve-
ment project.
Quality improvement is a necessary and essential
component in any CQI endeavor, and states should
design deliberate processes to ensure that the
waiver program’s performance undergoes routine
evaluation to identify and improve its operation. At
least once during the waiver’s approved period, and
as part of its quality improvement responsibilities,
CMS expects a state to
evaluate the eectiveness of its quality monitoring
processes (i.e., to determine if the state’s monitoring
processes work as well as they were intended). This
evaluation provides an opportunity for the state to
consider exploring more ecient and/or eective
approaches to its quality monitoring processes.
Appendix H of the waiver application requires states
to describe how and when they will conduct this
self-review.
Beyond Assurance-Based CQI
While CMS requires states to engage in quality
improvement activities related to the assurances
and subassurances, many states of their own accord
will identify aspects of their program they wish to
improve or enhance—aspects that are not directly
related to any of the assurances or subassurances.
For example, the state may install an automated
case management system or decide to upgrade its
information technology system. These types of im-
provements are encouraged by CMS, but they are of
a dierent nature than the improvement activities
associated with the assurances and subassurances.
States may also choose to track additional aspects
of program performance that go beyond the Fed-
eral requirements, and CMS is supportive of states
taking such initiatives.
The CMS Review Process
On a periodic basis, CMS requires states to submit
evidence that demonstrates their active monitor-
ing of their waivers, as well as compliance with the
assurances and subassurances. This evidence should
consist of summarized ndings of the Performance
Measures (Discovery Data), and summarized results
of all remediation actions taken when the state dis-
covered any non-compliance related to any Perfor-
mance Measures. Table 3 depicts what summarized
evidence might look for one performance measure.
States are also expected to report on any quality im-
provement actions they have initiated, the reasons
for conducting the quality improvement project,
the nature of the intervention, and the empirical
results of the improvement action (i.e., to what
extent it worked, as measured by an improvement
in the Performance Measure’s compliance rate). Cur-
rently, CMS requires states to submit information
on waiver quality on an annual basis in a 372 report,
a report that is waiver-specic and also includes
waiver cost and utilization data.
In addition to the annual reporting, prior to waiver
renewal CMS conducts an in-depth review of the
waiver program and requires the state to submit
evidence on all performance measures covering all
discovery, remediation, and improvement activity
reports for the rst 3 years of the waiver (and for the
rst 18 months for a new waiver).
�
After reviewing
the state’s evidence package, CMS issues a Findings
Report detailing whether the state met the assur-
ances. For a state that could not demonstrate it met
an assurance, the Findings Report will specify what
it must do to come into compliance if CMS is to
renew the waiver upon its expiration. A state found
out of compliance is typically required to submit an
action plan to CMS; once approved and the state
begins implementation, CMS will monitor the state’s
progress through state-submitted reports, telecon-
ferences, and on-site visits.
States should also expect to be visited by CMS sta
at least once during a waiver cycle. The purpose of
these visits is for CMS to verify that the monitoring
strategies that the state described in the approved
waiver application are actually being implemented,
and that monitoring reports are being generated in
245
Appendix: Medicaid HCBS Quality
the frequency specied in the application and used
by the state in operating the waiver. While on site,
CMS may (1)interview state sta to better under-
stand the processes and operations associated with
the quality improvement strategy, (2)”shadow”
quality oversight sta as they conduct monitoring
activities, (3)observe the state’s quality oversight
meetings where performance measure data and
remediation reports are reviewed and where quality
improvement activities are planned and evaluated,
and (4)visit providers to verify that the state is con-
ducting provider reviews as described in the waiver
application.
CMS may also visit a state if there are reports about
program participants’ health and welfare being seri-
ously jeopardized, or in the case of serious provider
infractions. Additionally, through-out the waiver’s
cycle, states should expect an ongoing dialogue
with CMS about waiver quality; both state sta and
CMS sta are expected to take responsibility for this
interchange.
Technical Assistance
for Medicaid HCBS Quality
CMS sta, be they Regional Oce sta assigned to
the waiver and/or sta in the Baltimore Central Of-
ce, are available to answer states’ questions about
Medicaid HCBS quality and to provide guidance. In
addition, since 2001 CMS has made available to the
states free quality-related technical assistance (TA)
through the National Quality Enterprise (NQE).
�
The
NQE provides one-on-one TA for states targeted
to specic waivers. In addition, the NQE conducts
HCBS Quality Training Forums consisting of tele-
conferences open to all states where topics related
to HCBS quality oversight are addressed by CMS,
national experts, and state HCBS sta. The NQE also
publishes periodic manuscripts on various HCBS
quality issues and maintains a website. This site in-
cludes links to many CMS documents pertaining to
HCBS quality, as well as manuscripts and resources
endorsed by CMS. Those joining the website are
able to post questions to peers in other states. Also,
states may request TA from the NQE through this
website. (See the Resources section for a web link to
the site.)
246 Understanding Medicaid Home and Community Services: A Primer
Resources
National HCBS Quality Enterprise Website
This website provides information on quality improvement for Medicaid §1915(c) HCBS waivers and the CMS
Quality Enterprise project. It also provides state Medicaid quality sta an opportunity to connect with one
another and pose questions to Quality Enterprise sta. Visitors must create a member’s account to access the
full site or can browse using a preview option.
Resources include CMS Quality Communications, technical assistance manuscripts, PowerPoint presentations,
and audio-recorded training calls. All of the materials posted on this website have been reviewed and ap-
proved by CMS. Material is added to the website on an ongoing basis and interested parties are encouraged to
check the website for updates. Below are some examples of material that may be found on the NQE website as
of the publication date of this Primer.
Web address: http://www.nationalqualityenterprise.net/
• B. Edwards, CMS Quality Communication #15: Web Based §1915(c) Waiver Application; Instructions and
Technical Guide; Resource Documents; 372 Online Form, CMS Disabled and Elderly Programs Group,
January 25, 2010.
• S. Galantowicz, Implementing Continuous Quality Improvement (CQI) in Medicaid HCBS Programs, Na-
tional Quality Enterprise, January 21, 2010.
• B. Jackson, PowerPoint presentation and audio recording: Examples of Performance Measures for the
§1915(c) Waiver Assurances (rst installment), January 14, 2010.
• B. Jackson, PowerPoint presentation and audio recording: Examples of Performance Measures for the
§1915(c) Waiver Assurances (second installment), March 11, 2010.
• G. Arden, CMS Quality Communication #12: Revised Interim Procedural Guidance (IPG) and Technical As-
sistance Products, CMS Disabled and Elderly Health Programs Group, February 6, 2007.
• R. Freedman and S. Taub, Sampling: A Practical Guide for Quality Management in Medicaid HCBS Waivers,
National Quality Contractor, March 2006.
• S. Galantowicz and B. Selig, Risk Management and Quality in HCBS: Individual Risk Planning and Preven-
tion, System-Wide Quality Improvement, National Quality Contractor, February 2005.
247
Appendix: Medicaid HCBS Quality
Centers for Medicare & Medicaid Services. (2008). Application for a §1915(c) Home and Community-
Based Waiver [Version 3.5]: Instructions, Technical Guide and Review Criteria. Baltimore, MD: Department
of Health and Human Services.
This publication contains extensive information concerning Federal policies that apply to the operation of an
HCBS waiver. In particular, Appendix G: Quality Improvement, Health and Welfare and Appendix H: System
Improvement are relevant to the forgoing discussion on Medicaid HCBS Quality. The instructions include tech-
nical guidance to aid states in designing an HCBS waiver, and incorporate the review criteria that CMS uses in
order to determine whether a waiver meets applicable statutory, regulatory, and other requirements.
Available at https://www.hcbswaivers.net/CMS/faces/portal.jsp under links and downloads, entitled §1915(c)
Waiver Application and Accompanying Materials.

248 Understanding Medicaid Home and Community Services: A Primer
Endnotes: Citations, Additional Information,
and Web Addresses
1
Beth Jackson is the author of this appendix. CMS funded the development of this appendix on quality
management systems.
2
CMS’s expectations for state responsibility for quality in Medicaid HCBS programs is most clearly
articulated for the §1915(c) waiver programs; however, the agency increasingly is looking to the
§1915(c) quality requirements as a model for further articulation of quality requirements for home
and community-based services provided under other Medicaid authorities, such as the §1915(a) and
§1915(b) authorities and the §1115 demonstration authority.
3
U.S. Government Accountability Oce. Long-Term Care: Federal Oversight of Growing Medicaid Home
and Community-Based Waivers Should Be Strengthened. GAO-03-576, June 2003.
4
Version 3.1 of the waiver application was issued in a Word format in 2005. In November 2006, CMS
launched the application in a web-based format under Version 3.4. In January 2008, CMS released
Version 3.5 where the quality-related portions were re-designed to elicit even more specic informa-
tion from the states on quality monitoring and improvement. As of April 1, 2010, use of the web-based
application is mandatory.
5
Assumes a Condence Level of .95 and a Condence Interval (Margin of Error) of +/–5.
6
Typically, stratication violates the simple random sample assumption that every unit within the
sample contributes equally. The sample size of the strata are often disproportionate to their represen-
tation in the population, and thus the sample must be statistically adjusted so that an estimate of the
entire population can be made, and to avoid having members of any one subgroup (strata) contribut-
ing more or less than a member of another subgroup.
7
This quality review process was instituted by CMS in January 2004 when they issued Interim Pro-
cedural Guidance. CMS updated aspects of this process in February 2007 with the Revised Interim
Procedural Guidance issued under Quality Communication #12 from the Director of the Disabled and
Elderly Health Programs Group.
8
From 2001–2008, the CMS-funded National Quality Contractor provided technical assistance to states.
In October 2008, CMS changed the funding mechanism to a grant and renamed it the National Quality
Enterprise.

Understanding Medicaid Home and Community Services: A Primer 2010 Edition
2010 Edition
U.S. Department of Health and Human Services
Office of the Assistant Secretary for Planning and Evaluation
U.S. Department of Health and Human Services
Office of the Assistant Secretary for Planning and Evaluation
200 Independence Avenue, Washington, DC 20201
Understanding Medicaid
Home and Community Services:
A Primer
To obtain a printed copy of this report, send the full report title and your mailing
information to:
U.S. Department of Health and Human Services
Office of Disability, Aging and Long-Term Care Policy
Room 424E, H.H. Humphrey Building
200 Independence Avenue, S.W.
Washington, D.C. 20201
FAX: 202-401-7733
Email: [email protected]
RETURN TO:
Office of Disability, Aging and Long-Term Care Policy (DALTCP) Home
[http://aspe.hhs.gov/_/office_specific/daltcp.cfm]
Assistant Secretary for Planning and Evaluation (ASPE) Home
[http://aspe.hhs.gov]
U.S. Department of Health and Human Services Home
[http://www.hhs.gov]
