RESEARCH BRIEF | 1
August 2022 (REVISED)
ASPE RESEARCH BRIEF
HHS OFFICE OF THE ASSISTANT SECRETARY FOR PLANNING AND EVALUATION
OFFICE OF BEHAVIORAL HEALTH, DISABILITY, AND AGING POLICY
LONG-TERM SERVICES AND SUPPORTS FOR
OLDER AMERICANS: RISKS AND FINANCING, 2022
Most Americans underestimate the risk of developing a disability and needing long-term
services and supports (LTSS). Using microsimulation modeling, we estimate that over half
(56%) of Americans turning 65 today will develop a disability serious enough to require LTSS,
although many will need assistance for less than three years. About one in five of all adults
(22%), however, will have a disability for more than five years. On average, an American
turning 65 today will incur $120,900 in future LTSS costs, measured in today’s dollars.
Families will pay more than one-third (37%) of the costs themselves out of pocket, with the
rest covered by public programs and private insurance. Although most people with LTSS
needs will spend relatively little on their care, 14% will spend at least $100,000 out of pocket
for future LTSS. But these paid services do not cover all care people need, and consistent
with prior research we find that family caregivers provide substantial unpaid care. Valuing
unpaid care contributions at the wage of a paid caregiver, we estimate that unpaid family care
for older adults with significant disabilities who receive care is worth $204,000 on average,
more than the expected cost of all paid LTSS. Without help from unpaid family caregivers,
families and public programs would spend much more on LTSS.
Background
Long-term services and supports (LTSS) includes a range of assistance individuals may
need to meet their health or personal needs over an extended period.
1
Most LTSS is
not medical care, but rather assistance with the basic personal tasks of everyday life,
sometimes called activities of daily living (ADLs), which include such tasks as bathing,
dressing, toileting and eating (Katz et al. 1963).
2
Many Americans prefer not to think
about this need for assistance or who will provide it. They underestimate the likelihood
that they will need help and how much it will cost (Wiener et al. 2015; Kane 2013;
Tompson et al. 2013). Even if they recognize the possibility of developing a disability
and needing daily help, many Americans mistakenly assume that insurance will cover
these costs. However, health insurance does not cover LTSS costs, and Medicare, the
major public insurance program for older Americans, does not cover most LTSS
expenses (Centers for Medicare & Medicaid Services 2015).
3
Relatively few financing options exist for LTSS. Although Medicaid provides LTSS to
those with chronic disabling conditions (Komisar 2013; Tompson et al. 2013),
4
it is
available only for individuals who meet income and other eligibility requirements (U.S.
Department of Health and Human Services 2015). A private market for LTSS insurance
RESEARCH BRIEF | 2
exists, but less than 8% of Americans have purchased coverage (Freundlich 2014),
partly because of high and rising premiums and the exit of insurers from the market
(Scism 2015). Sales figures from recent years suggest the market has stagnated or
even shrunk (Cohen 2016; Schmitz and Giese 2019; Ujvari 2018). In 2018, just
276,000 people received benefits from long-term care insurance (LTCI) and about 6.58
million people--less than 6% of the population ages 50 and older--had a long-term care
policy (National Association of Insurance Commissioners 2019). For some older adults,
the costs of LTSS are likely to outstrip retirement savings. Researchers at the
Employee Benefit Research Institute found that accounting for LTSS expenses
significantly increase the number of retirees projected to have inadequate resources to
cover living expenses (VanDerhei 2015).
As the United States population ages, a growing number of older adults will likely need
and use LTSS. Most Americans who receive paid LTSS pay some share out of pocket.
Those with longer spells may pay out of pocket until they qualify for Medicaid. Reliance
on Medicaid for those who cannot afford the full cost of LTSS may increase federal and
state spending for LTSS. The Congressional Budget Office projects that if the share of
adults ages 65 and older with functional limitations remains constant LTSS expenses
(including all paid care financed by Medicaid and other private and public sources,
including Medicare payments for post-acute services) could more than double between
2010 and 2050 as the population grows, increasing from 1.3% to 3.0% of gross
domestic product (Hagen 2013).
To provide context for policymakers and others considering LTSS financing proposals,
this brief presents information about the risk of needing care and associated costs,
based on results from a microsimulation model. This model projects the percentage of
older adults who will develop a disability and use paid LTSS. For those who use paid
LTSS, the model projects how much they will use and for how long. The model also
estimates care costs and how they would be financed under current policies.
Microsimulation modeling describes the average likelihood of these outcomes, as well
as the distribution of these needs and costs. Throughout this brief we focus on
significant disabilities that result in LTSS needs at the threshold for benefits under a tax-
qualified LTCI policy, set in the Health Insurance Portability and Accountability Act
(HIPAA): a need for assistance with at least two ADLs
5
that is expected to last at least
90 days or a need for substantial supervision for health and safety threats due to severe
cognitive impairment.
6
HIPAA does not count ADL limitations that can be resolved with
special equipment, such as wheelchairs, walkers, handrails, ramps, catheters, and
related devices (Stallard 2011). Estimates of disability prevalence are higher when we
include people with less severe disabilities and people with disabilities that can be
mitigated with special equipment.
Methods
The findings in this brief--an update of Favreault and Dey (2016)--are derived from
analyses using the Urban Institute’s Dynamic Simulation of Income Model 4
(DYNASIM4), a microsimulation model designed to analyze retirement and aging
issues. Starting with a representative sample of individuals and families, the model

RESEARCH BRIEF | 3
“ages” cohorts year-by-year, simulating such demographic events as births, deaths,
marriages, and divorces, and such economic and health events as labor force
participation, earnings, hours of work, disability onset and recovery, retirement, and use
and costs of LTSS. Simulations of these events and outcomes vary with demographic
and other characteristics of the population.
7
As the model ages the population, it
calibrates many key demographic and economic outcomes to the intermediate
assumptions of the Social Security and Medicare trustees’ reports (Board of Trustees,
Federal Old-Age and Survivors Insurance and Federal Disability Insurance Trust Funds
2021; Boards of Trustees, Federal Hospital Insurance and Federal Supplementary
Medical Insurance Trust Funds 2019). Data to inform the model are drawn from the
Health and Retirement Study, especially in the areas of health, disability (including
cognitive impairment and limitations in ADLs and instrumental activities of daily living
[IADLs]), LTSS use, and private LTCI coverage.
8
Because we rely on historical data,
the projections do not reflect how the COVID-19 pandemic might shift LTSS use.
Current and past LTSS prices are set equal to average or median prices reported in the
literature by state of residence, setting (home care, residential care, nursing home), and
whether Medicaid is the payer (Fossett and Burke 2010; Genworth 2019; Grabowski et
al. 2004; Hansen Hunter and Company 2018; Mollica 2009; Ng et al. 2014).
9
These
base projections incorporate the full cost of residential care, including room and board in
addition to costs associated with meeting care needs. They also incorporate home care
services that families purchase in private transactions, which are rapidly evolving and
which some other studies undercount (Doty 2017; HomecarePulse 2019; Kim 2022;
Newquist, DeLiema and Wilber 2015). The projections include hospice care, which
Medicare pays, but excludes other Medicare-financed services that are strictly post-
acute (see Box 1). These choices affect payer mix and comparability with other
estimates of LTSS expenses, including Favreault and Dey (2016).
BOX 1: Should We Include Medicare as a Payer for LTSS?
Many adults are confused about whether Medicare covers personal assistance if they develop LTSS
needs (also referred to as long-term care needs).
The Centers for Medicare & Medicaid Services is clear about Medicare policies on its website
(https://www.medicare.gov/coverage/long-term-care), which states the following:
• “Medicare doesn’t cover long-term care (also called custodial care), if that’s the only care you need.
Most nursing home care is custodial care.”
• “You pay 100% for non-covered services, including most long-term care.”
• “Long-term care is a range of services and support for your personal care needs. Most long-term
care isn’t medical care. Instead, most long-term care is help with basic personal tasks of everyday
life, sometimes called activities of daily living.”
Because Medicare does not cover LTSS when it is the only care people need, some analysts exclude
Medicare when describing who pays for LTSS (Hado and Komisar 2019). However, several prominent
government publications describe Medicare as an important LTSS payer (Hagen 2013; Colello 2022) and
include all Medicare services delivered in certain settings as LTSS. They make this choice because
National Health Expenditure Accounts (NHEA) data enable researchers to determine the settings in which
care is delivered, but not to determine whether the care is non-medical, making disaggregation difficult.
In a departure from Favreault and Dey (2016), we follow Hado and Komisar (2019) and do not include in
our projections any incidental care that Medicare finances, with one exception: the projections include the
value of Medicare-financed hospice care if it is provided to people meeting a HIPAA-level-of-need
threshold.
RESEARCH BRIEF | 4
Finally, we value unpaid family care at the approximate cost of hiring someone to
provide care. For each hour of unpaid care provided to a person with significant
disabilities, we assign a value equal to the median hourly wage for home care workers
in the care recipient’s state of residence. This projection is likely a lower bound for the
total value of unpaid family care because our estimates ignore administrative hiring
costs, any nonwage compensation that paid caregivers receive, and the value of care
provided to older adults with less-significant disabilities, which is likely substantial.
Additional details about the model’s assumptions are available in Johnson (2022).
Results
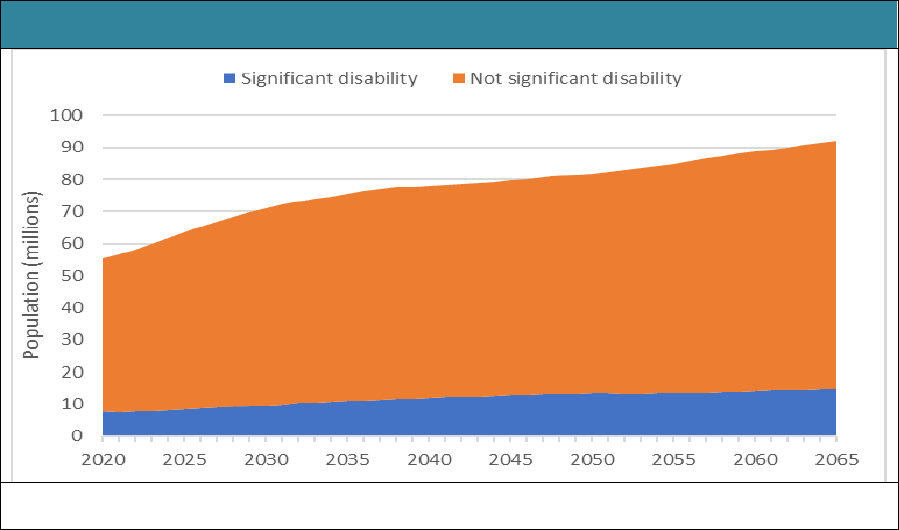
Figure 1 presents projections of the number of people ages 65 and older and the
number with significant disabilities from 2020 to 2065. As expected, given the aging
population, the number with significant disabilities is projected to grow substantially,
increasing from 7.6 million to almost 14.7 million. In percentage terms, the share of the
older population with significant disabilities increases from 14% to 16%.
FIGURE 1. Total Population Ages 65 and Older,
Including the Number of People Projected to Have Significant Disabilities, 2020-2065
SOURCE: Authors’ tabulations from DYNASIM4, run id982.
NOTE: Estimates are for adults born between 1941 and 1974 who survive to age 65.
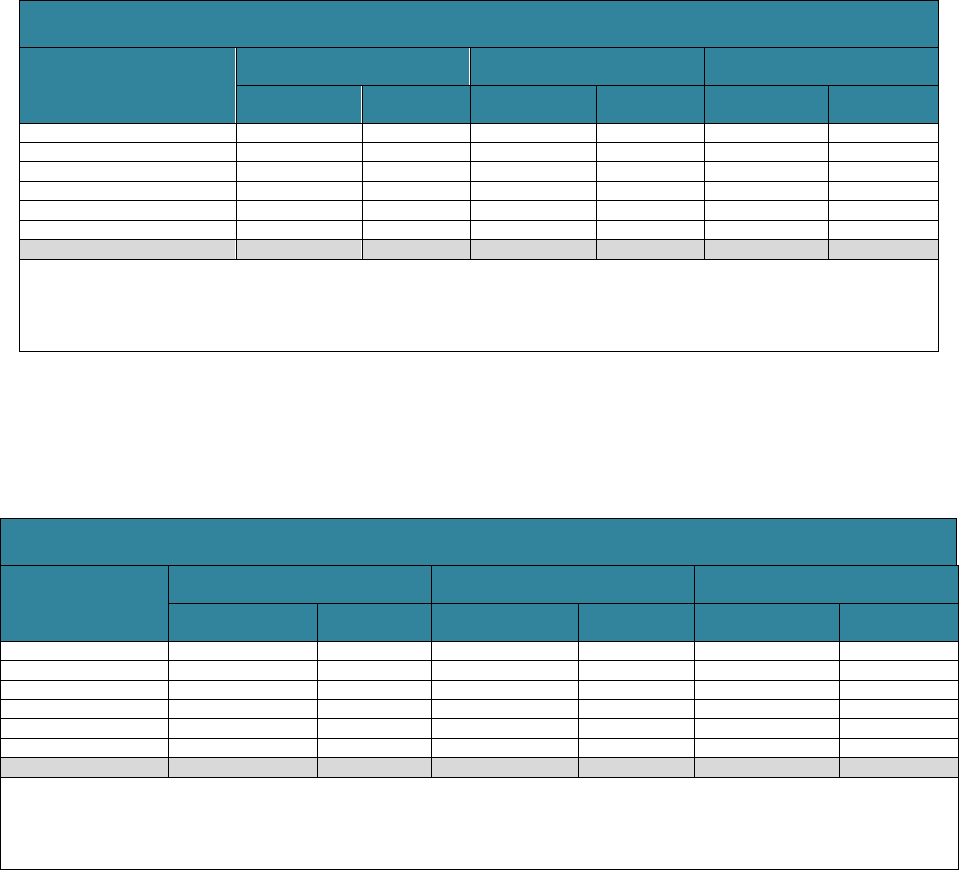
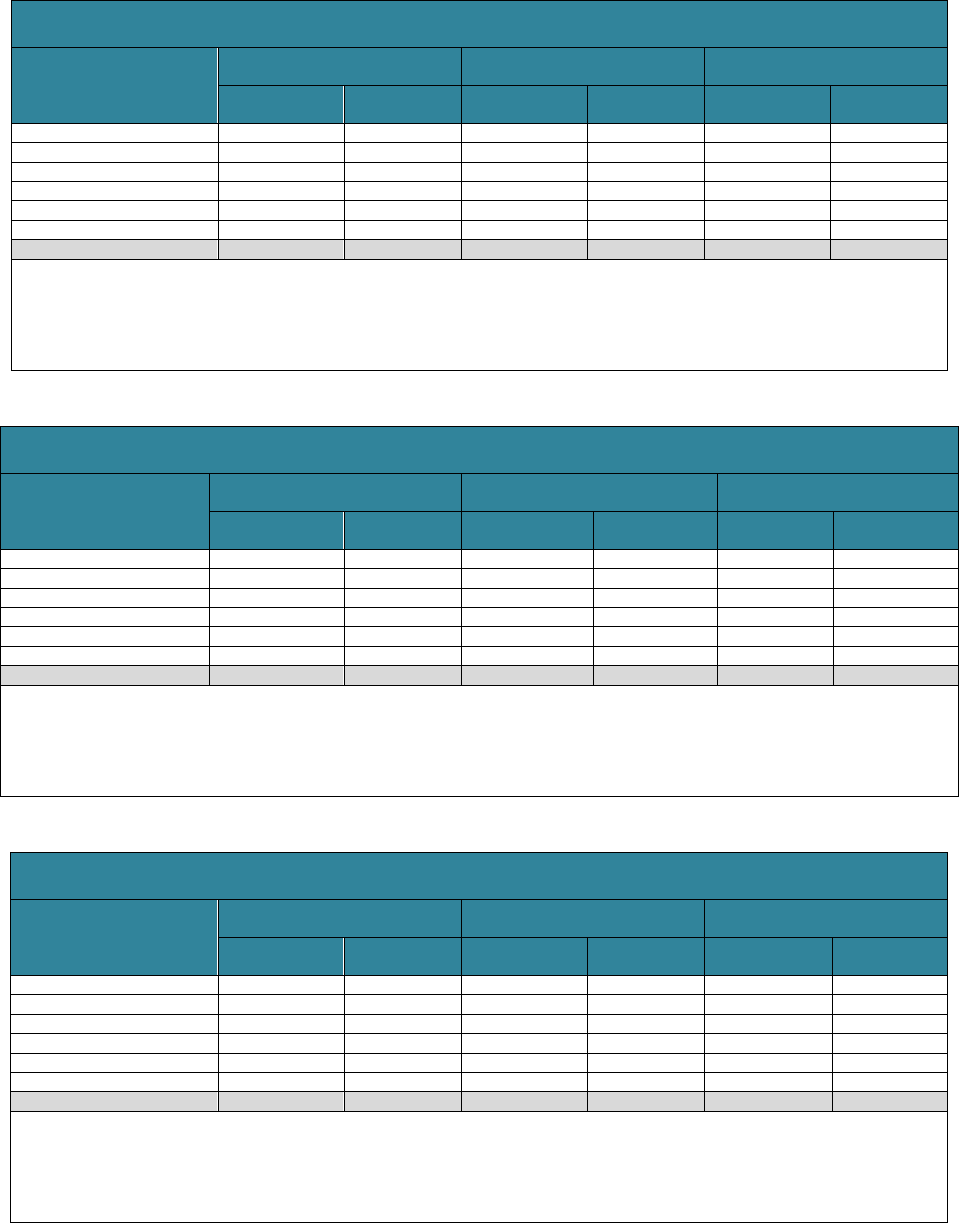
Table 1 displays expected LTSS needs from age 65 to death. It presents life
expectancy at age 65 and the mean and distribution of the duration of disability for
adults turning 65 between 2021 and 2025.
10
The typical person in this cohort who is
alive at age 65 can expect to live another 20.5 years. Fifty-six percent can anticipate
having at least some significant need for LTSS; 12% are expected to have needs that
last less than a year, and about 22% are expected to have needs that extend beyond
five years. Estimates such as these are sensitive to the definition of disability. Many
people whose disabilities do not reach higher levels of significance still need and use
LTSS. With a more expansive definition, such as one that includes those with one ADL
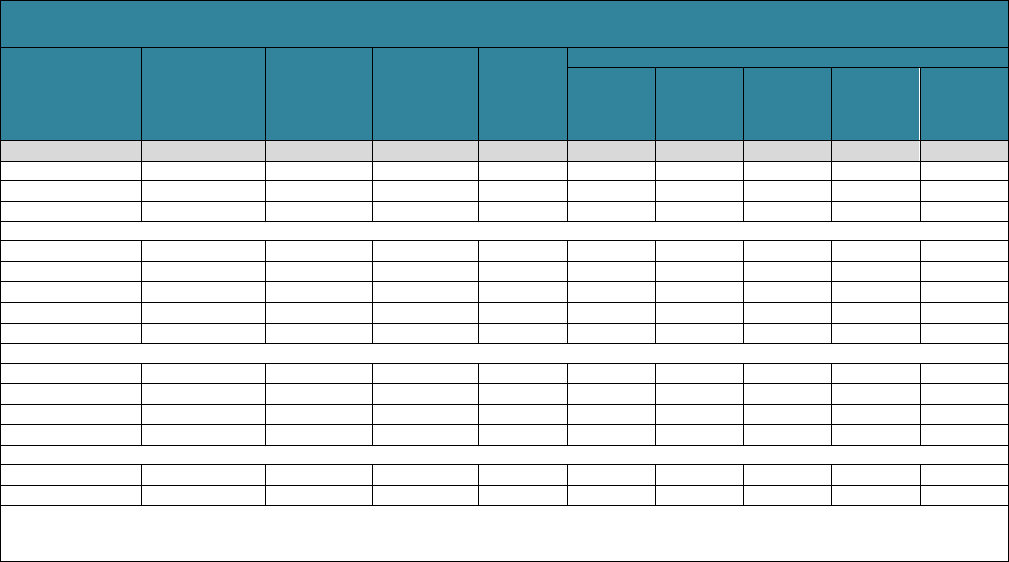
RESEARCH BRIEF | 5
limitation or only IADLs limitations without severe cognitive impairment, the number of
people with LTSS needs would be significantly higher (Freedman and Spillman 2014;
Kemper, Komisar and Alecxih 2005/2006).
TABLE 1. Projected Need for LTSS for People Turning 65 in 2021-2025,
by Gender, Income, Self-Reported Health Status, and Marital Status
Life Expectancy
at Age 65
(years, full
population)
Average
Years of
LTSS Need
(all)
Average
Years of
LTSS Need
Given Some
Need
Percent
with Some
LTSS
Need
Distribution of LTSS Needs for the Full Population (%)
None
<1 Year
1.00-1.99
Years
2.00-4.99
Years
>5 Years
Total
20.5
3.1
5.4
56.4
43.6
11.9
7.9
14.7
22.1
Gender
Men
19.1
2.5
5.1
48.6
51.4
11.2
7.1
12.8
17.5
Women
21.9
3.6
5.6
63.7
36.3
12.4
8.6
16.4
26.3
Income Quintile at Age 65
Lowest
18.2
3.8
6.1
62.9
37.1
12.0
7.8
14.5
28.6
Second
19.1
3.0
5.3
57.3
42.7
12.7
8.2
14.9
21.5
Middle
20.3
3.2
5.8
54.8
45.2
10.1
7.9
14.4
22.4
Fourth
21.0
2.7
4.9
54.3
45.7
11.5
8.4
15.0
19.5
Highest
23.2
2.8
5.1
54.0
46.0
12.8
7.2
14.5
19.6
Health Status at Age 65
Excellent
22.3
2.8
5.1
55.6
44.4
11.5
7.6
17.0
19.5
Very good
21.4
3.0
5.4
55.5
44.5
11.2
8.5
13.8
22.0
Good
20.4
2.8
5.2
54.1
45.9
12.3
7.4
14.1
20.3
Fair/poor
18.9
3.5
5.7
60.3
39.7
12.2
7.7
15.1
25.3
Marital Status at Age 65
Married
21.6
2.9
4.7
54.9
45.1
11.9
7.8
14.6
20.6
Unmarried
19.7
3.4
5.4
60.0
40.0
11.9
8.2
15.2
24.7
SOURCES: Authors’ tabulations from DYNASIM4, run id982
NOTES: LTSS need is defined as a need for assistance with at least two activities of daily living or supervision due to severe cognitive impairment that is expected to last
at least 90 days.
LTSS needs vary substantially by personal characteristics. The average duration of
disability is higher for women (3.6 years) than for men (2.5 years). Among women, 64%
are likely to develop a significant disability, and 26% will need at least 5 years of care.
The proportion needing at least five years of care is especially high among those in the
lowest income quintile at age 65 (29%)
11
and those reporting fair or poor health at age
65 (25%). Among those who ever develop a significant disability, the average duration
is 5.6 years for women and 5.1 years for men.
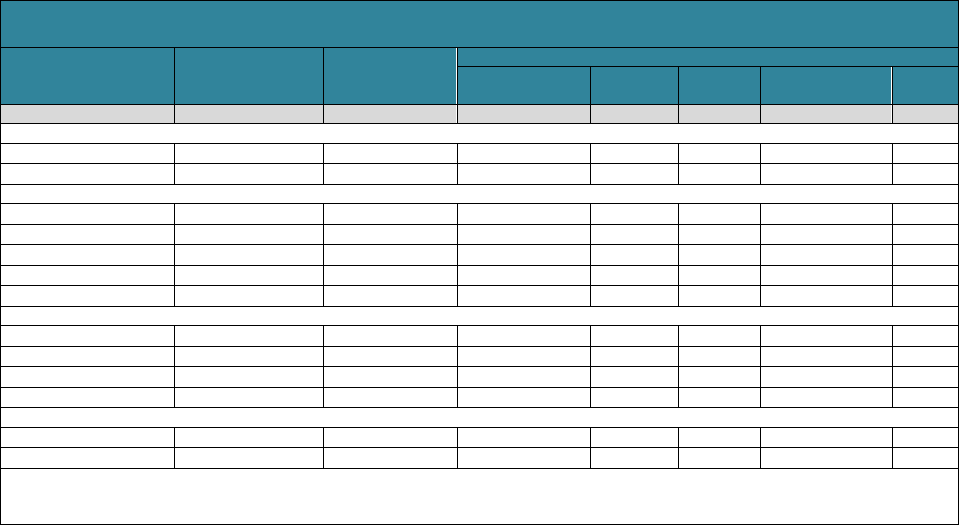
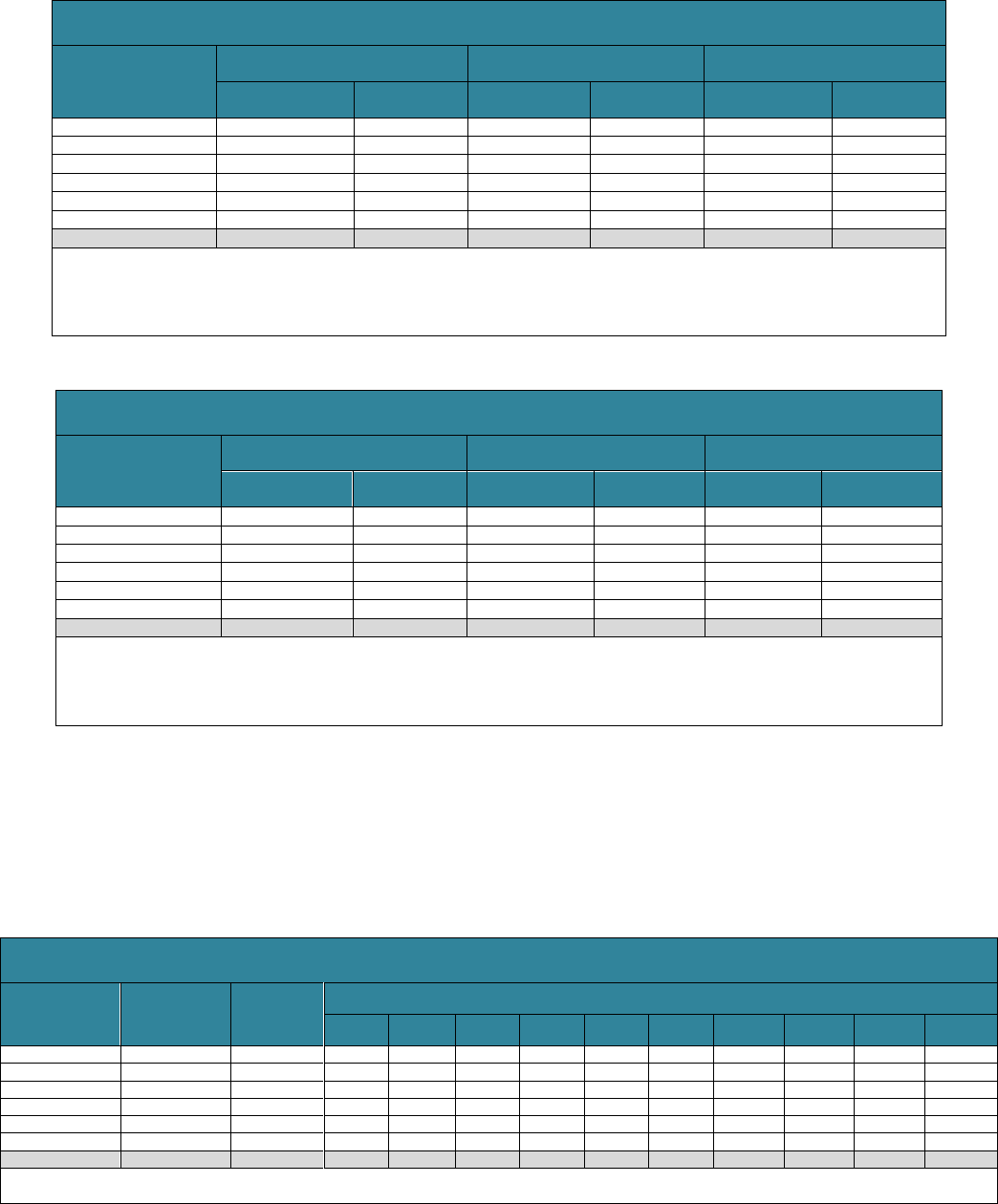
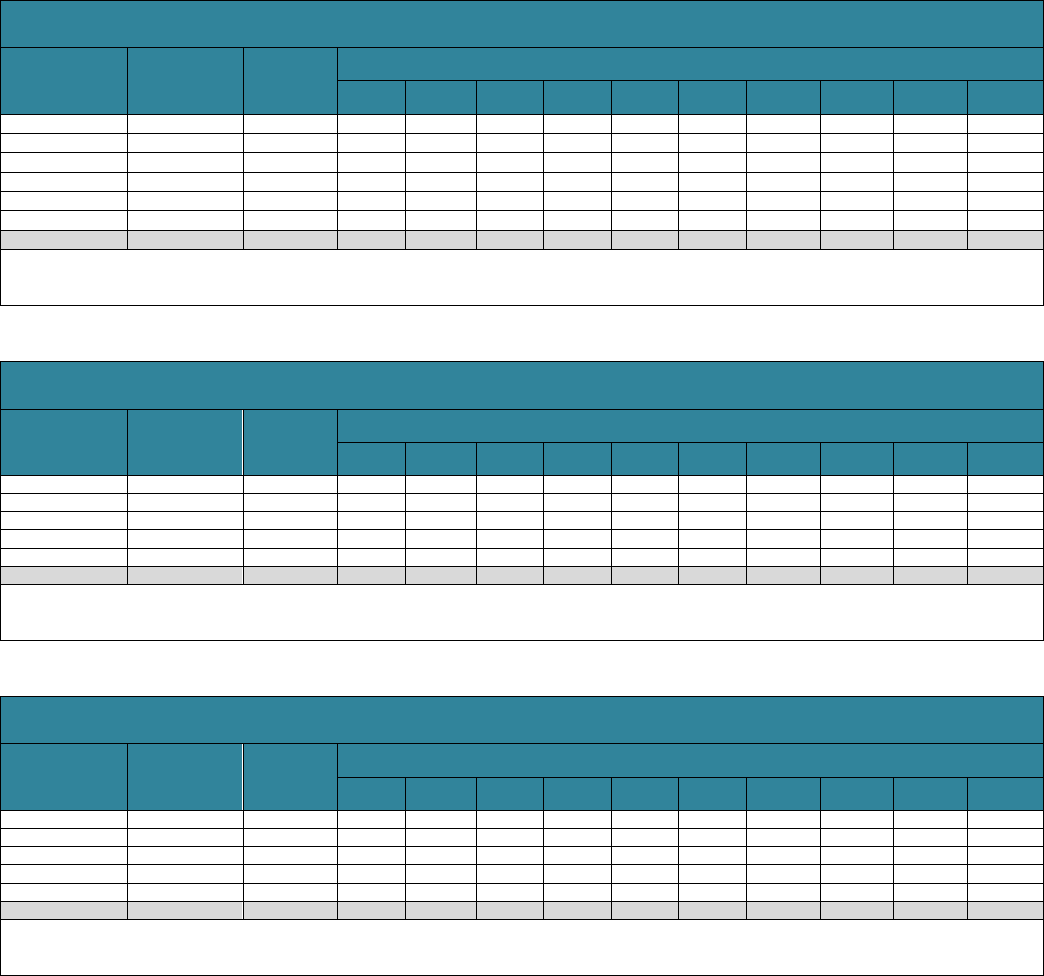
Table 2 examines the use of paid LTSS for a significant disability from age 65 onward
measured in service days (where 365 days of paid LTSS counts as one year,
regardless of whether all care occurs in the same calendar year). Of the average 3.1
years that older adults are projected to have a significant disability, they will receive paid
care for about 0.8 years, and unpaid caregivers, such as family and friends, will make
up most of the difference.
12
Again, patterns vary by personal characteristics. People
who are unmarried at age 65 use more paid services than those who are married (1.0
years, on average, compared with 0.7 years). Those in poor health at age 65 and those
with lower income at age 65, many of whom qualify for Medicaid, use more paid
services.
Distribution of LTSS Needs
for the Full Population (%)
Distribution of LTSS Needs for
the Full Population (%)
Distribution of LTSS Needs
for the Full Population (%)
Distribution of LTSS
Needs for the Full
Population (%)
RESEARCH BRIEF | 6
TABLE 2. Projected Use of Paid LTSS for People Who Turn 65 in 2021-2025, by Gender,
Income Quintile, Self-Reported Health Status, and Marital Status
Average Years with
Paid LTSS Use
Percent with Any
Paid LTSS Use
(all)
Distribution of Paid LTSS Use for the Full Population (%)
None
<1 Year
1.00-1.99
Years
2.00-4.99 Years
>5
Years
Total
0.8
45.3
54.7
24.1
7.3
9.5
4.4
Gender
Men
0.6
38.9
61.1
22.2
6.2
7.4
3.1
Women
1.0
51.3
48.7
25.9
8.4
11.4
5.6
Income Quintile at Age 65
Lowest
1.2
49.4
50.7
23.7
6.7
10.6
8.4
Second
0.8
45.6
54.4
26.1
6.7
8.5
4.3
Middle
0.7
44.7
55.3
25.2
6.3
9.3
4.0
Fourth
0.7
44.0
56.1
23.4
8.8
9.0
2.8
Highest
0.7
43.7
56.3
22.9
7.7
10.1
3.1
Health Status at Age 65
Excellent
0.8
46.1
53.9
23.1
8.6
10.9
3.5
Very good
0.8
45.5
54.5
25.0
7.1
9.1
4.3
Good
0.7
43.2
56.8
23.6
7.4
8.7
3.5
Fair/poor
1.0
47.1
52.9
24.3
6.8
10.2
5.8
Marital Status at Age 65
Married
0.7
42.5
57.5
23.4
7.1
8.7
3.4
Unmarried
1.0
50.5
49.5
25.9
7.9
10.9
5.9
SOURCES: Authors’ tabulations from DYNASIM4, run id982
NOTES: LTSS need is defined as a need for assistance with at least two activities of daily living or supervision due to severe cognitive impairment that is
expected to last at least 90 days.
While individuals on average will need 0.8 years of paid LTSS, 55% of older adults will
not use any paid LTSS. About 24% of older adults (or about half of paid LTSS users)
will receive less than a year of paid LTSS (measured in service days), and about 4% of
older adults will use five years or more. These projections are similar to Johnson’s
(2019) estimates of care use based on recent historical data.
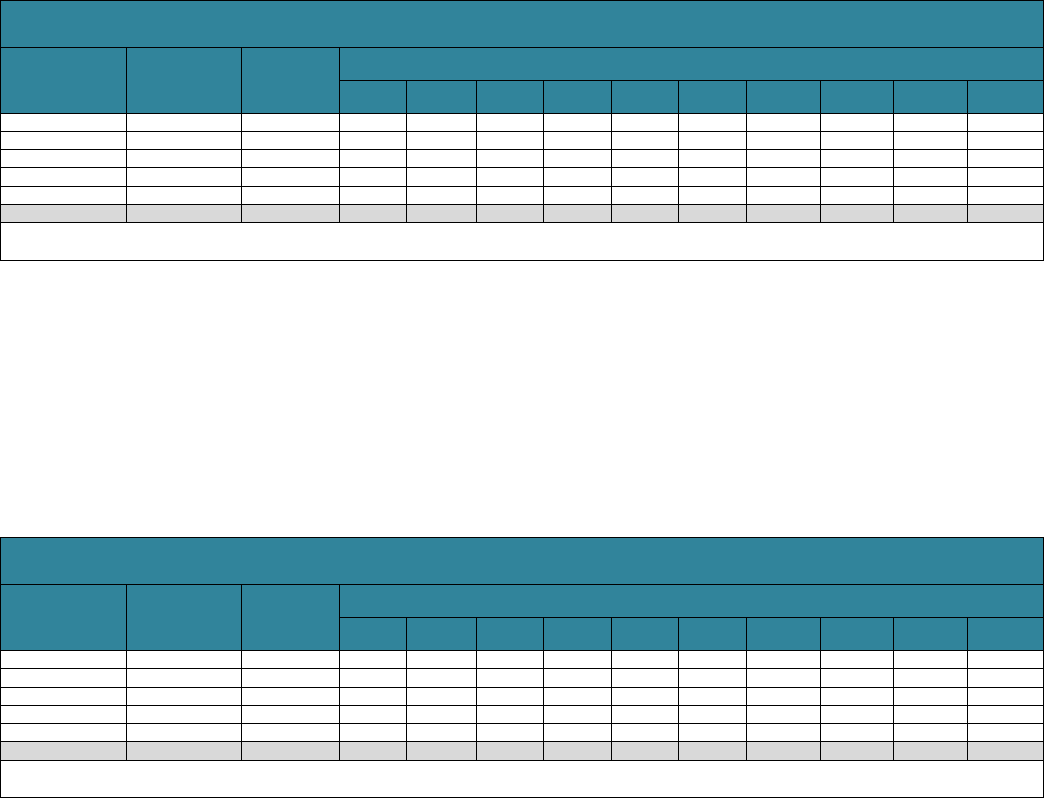
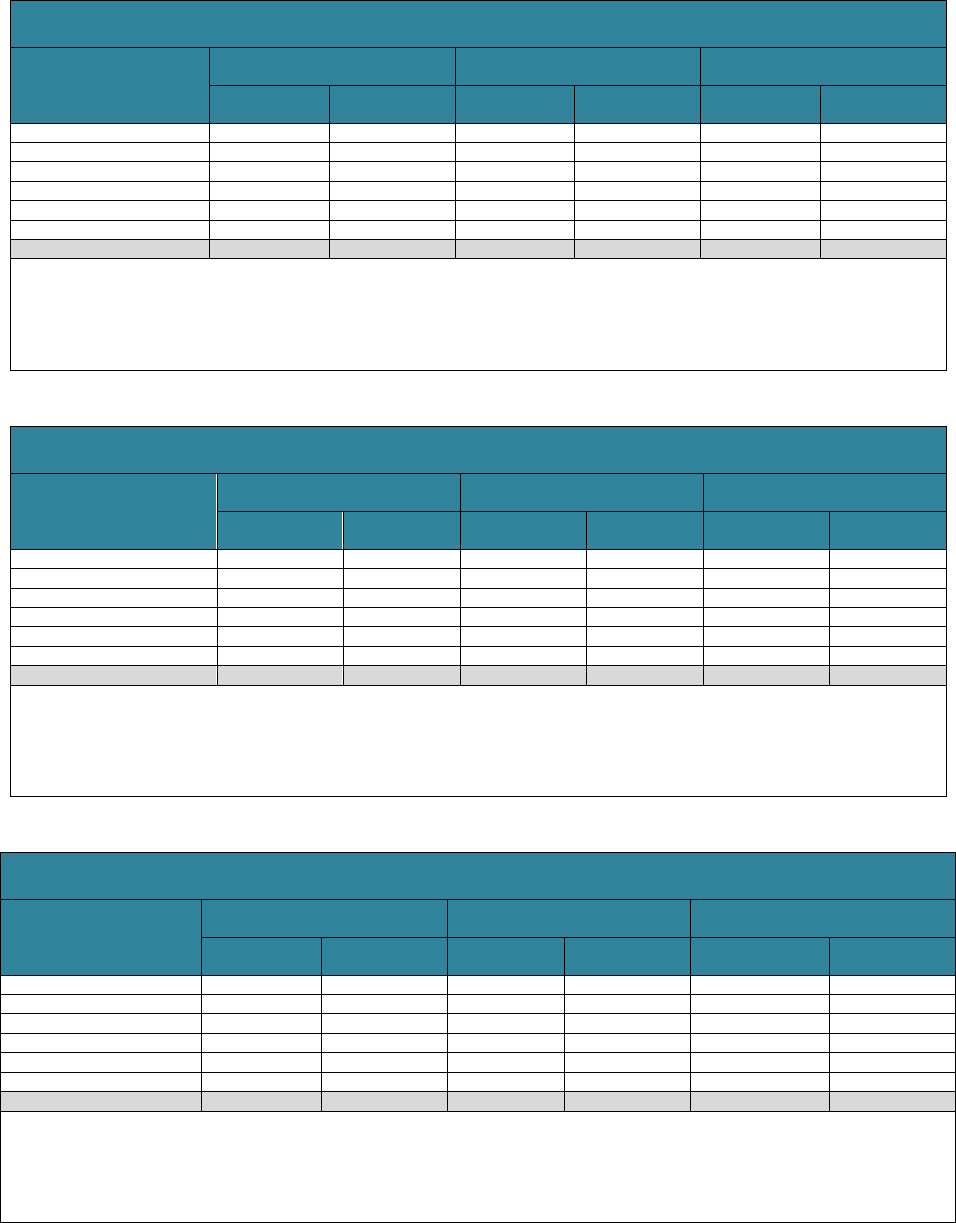
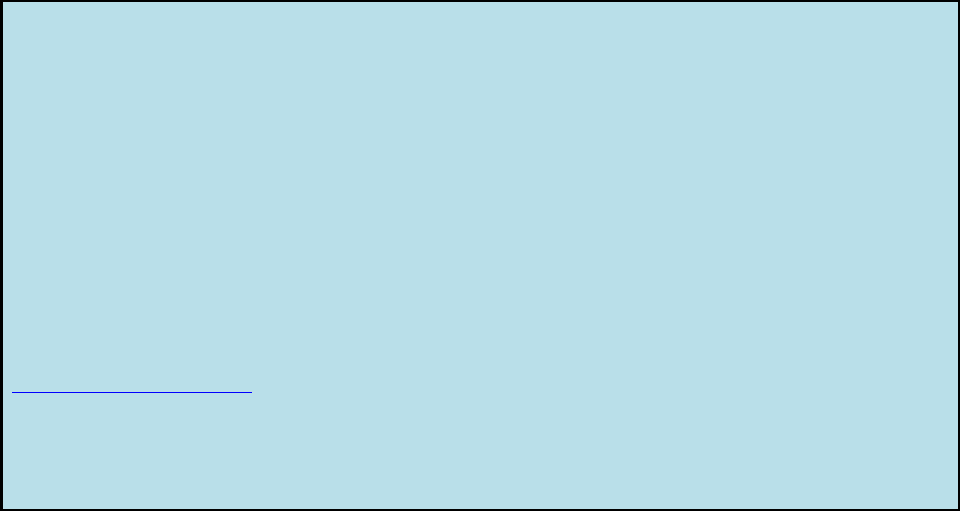
Table 3 presents the average sum of expenditures for LTSS (in 2020 dollars) that could
be expected from age 65 until death for the entire population, and Table 4 repeats the
analysis for those who use paid LTSS. The tables display this projected sum of
expenditures by setting and payer for those reaching age 65 between 2021 and 2025.
These estimates differ from a present discounted value (PDV) of expenditures at age
65, the amount that an individual would need to set aside at age 65 to cover future
LTSS expenses. The PDV is lower than the sum-of-expenditures measure because it
accounts for the investment returns that could be earned on funds set aside at age 65
until LTSS expenses begin, often after age 80. We show PDV projections in the
appendix.
13
We project that total paid LTSS expenses will average $120,900 per person (Table 3).
14
Medicaid is the largest payer of LTSS, averaging $51,800 after age 65 and accounting
for 43% of the total. Family out-of-pocket costs are also substantial, averaging $44,800
and accounting for 37% of the total. Payments vary by setting. Medicaid covers more
than half (52%) of total costs in institutional settings, whereas out-of-pocket payments
by families account for 44% of total community-based expenses.
15
Distribution of Paid LTSS Use for
the Full Population (%)
Distribution of Paid LTSS Use for the
Full Population (%)
Distribution of Paid LTSS Use for the Full
Population (%)
Distribution of Paid LTSS Use for
the Full Population (%)
RESEARCH BRIEF | 7
TABLE 3. Projected Sum of LTSS Expenditures from Age 65 through Death
for Adults Who Turn 65 in 2021-2025, by Payer and Setting
Payer
All Settings
Community-Based
(includes residential care)
Nursing Facility
Average ($)
Percentage
of total
Average ($)
Percentage
of total
Average ($)
Percentage
of total
Public
$70,100
58
$27,100
48
$43,000
67
Medicaid
51,800
43
18,600
33
33,200
52
Other Public
18,300
15
8,500
15
9,800
15
Private
$50,800
42
$29,400
52
$21,500
33
Out-of-Pocket
44,800
37
24,800
44
20,100
31
Private Insurance
6,000
5
4,600
8
1,400
2
All Payers
$120,900
100
$56,500
100
$64,400
100
SOURCES: Authors’ tabulations from DYNASIM4, run id982.
NOTES: Estimates are reported in 2020 inflation-adjusted dollars. Residential care is included in community-based care, not
nursing-facility care. LTSS prices are state- and setting-specific, based on Genworth (2019), Hansen Hunter and Company PC
(2018), and other sources. Nursing home and residential care prices are adjusted for wage inflation; home care prices grow
with the average of wage and price inflation. Components do not always sum to totals because of rounding.
Among those who ever use paid LTSS after turning age 65, the average cost is
projected at $245,400 (Table 4). Although conditioning on the use of LTSS increases
average costs, the cost distribution by payer and setting is very similar to that shown in
Table 3.
TABLE 4. Projected Sum of LTSS Expenditures from Age 65 through Death
for Users of Paid LTSS Who Turn 65 in 2021-2025, by Payer and Setting
Payer
All Settings
Community-Based (includes
residential care)
Nursing Facility
Average ($)
Percentage
of total
Average ($)
Percentage
of total
Average ($)
Percentage
of total
Public
$139,700
57
$52,500
46
$87,200
67
Medicaid
102,900
42
35,500
31
67,400
52
Other Public
36,800
15
17,000
15
19,800
15
Private
$105,700
43
$62,200
54
$43,500
33
Out-of-Pocket
93,500
38
52,800
46
40,700
31
Private Insurance
12,200
5
9,400
8
2,800
2
All Payers
$245,400
100
$114,700
100
$130,700
100
SOURCES: Authors’ tabulations from DYNASIM4, run id982.
NOTES: Estimates are reported in 2020 inflation-adjusted dollars. Residential care is included in community-based care, not
nursing-facility care. LTSS prices are state- and setting-specific, based on Genworth (2019), Hansen Hunter and Company PC
(2018), and other sources. Nursing home and residential care prices are adjusted for wage inflation; home care prices grow with the
average of wage and price inflation. Components do not always sum to totals because of rounding.
Expected LTSS costs are higher for women than men. Women’s costs average
$154,300 (Table 5), compared with $85,400 for men (Table 6). When we restrict our
analysis to adults with any LTSS expenditures, this average increases to $277,900 for
women and $200,400 for men (not shown). Women spend more on LTSS than men
because they tend to live longer and thus are more exposed to the risk of needing
LTSS. Additionally, married women are often younger than their husbands and more
likely to become widowed at older ages, leaving women less likely to receive unpaid
spousal care (and more likely to provide it).
All Settings
All Settings
Community Based
(Includes residential
care)
Community Based (Includes
residential care)
Nursing Facility
Nursing Facility
RESEARCH BRIEF | 8
TABLE 5. Projected Sum of Expenditures from Age 65 through Death,
for Women Who Turn 65 in 2021-2025, by Payer and Setting
Payer
All Settings
Community-Based (includes
residential care)
Nursing Facility
Average ($)
Percentage
of total
Average ($)
Percentage
of total
Average ($)
Percentage
of total
Public
$90,000
58
$33,200
47
$57,000
68
Medicaid
68,400
44
23,000
32
45,500
54
Other Public
21,600
14
10,200
14
11,500
14
Private
$64,300
42
$37,700
53
$26,600
32
Out-of-Pocket
56,400
37
31,400
44
25,000
30
Private Insurance
7,900
5
6,300
9
1,600
2
All Payers
$154,300
100
$70,800
100
$83,500
100
SOURCES: Authors’ tabulations from DYNASIM4, run id982.
NOTES: Estimates are reported in 2020 inflation-adjusted dollars. Residential care is included in community-based care, not
nursing-facility care. LTSS prices are state- and setting-specific, based on Genworth (2019), Hansen Hunter and Company PC
(2018), and other sources. Nursing home and residential care prices are adjusted for wage inflation; home care prices grow with
the average of wage and price inflation. Components do not always sum to totals because of rounding.
TABLE 6. Projected Sum of Expenditures from Age 65 through Death
for Men Who Turn 65 in 2021-2025, by Payer and Setting
Payer
All Settings
Community-Based (includes
residential care)
Nursing Facility
Average ($)
Percentage
of total
Average ($)
Percentage
of total
Average ($)
Percentage
of total
Public
$48,700
57
$20,600
50
$28,100
64
Medicaid
34,000
40
13,900
34
20,100
46
Other Public
14,700
17
6,700
16
8,000
18
Private
$36,700
43
$20,700
50
$16,000
36
Out-of-Pocket
32,600
38
17,800
43
14,800
34
Private Insurance
4,100
5
2,900
7
1,200
3
All Payers
$85,400
100
$41,300
100
$44,100
100
SOURCES: Authors’ tabulations from DYNASIM4, run id982.
NOTES: Estimates are reported in 2020 inflation-adjusted dollars. Residential care is included in community-based care, not
nursing-facility care. LTSS prices are state- and setting-specific, based on Genworth (2019), Hansen Hunter and Company PC
(2018), and other sources. Nursing home and residential care prices are adjusted for wage inflation; home care prices grow with
the average of wage and price inflation. Components do not always sum to totals because of rounding.
Table 7 presents the distribution of the sum of expected costs for adults ages 65 and
older in 2021-2025 by payer. About 15% of older adults can expect their total LTSS
expenses from age 65 onward to amount to more than $250,000, whereas about 8%
will have positive but low costs (less than $10,000). A smaller percentage (about 6%)
will spend $250,000 or more out of pocket on LTSS. Fourteen percent will spend at
least $100,000 out of pocket on LTSS after turning 65.
TABLE 7. Projected Average and Distribution of Sum of LTSS Expenditures from Age 65
through Death for Adults Turning 65 in 2021-2025, by Payer
Payer
Average
Expenditures
Percent of
People with
Expenditures
Distribution of Sum of LTSS Expenditures
(% of people)
None
<$10,000
$10,000-
$24,999
$25,000-
$49,999
$50,000-
$74,999
$75,000-
$99,999
$100,000-
$149,999
$150,000-
$199,999
$200,000-
$249,999
>$250,000
Public
$70,100
Medicaid
51,800
18.3
81.7
2.4
1.4
1.5
1.1
1.0
1.6
1.5
1.2
6.8
Other Public
18,300
40.9
59.1
13.2
8.6
8.1
3.8
2.2
2.4
1.0
0.6
0.8
Private
$50,800
Out-of-Pocket
44,800
34.9
65.1
5.9
5.0
4.4
3.2
2.3
3.7
2.3
1.6
6.4
Private Insurance
6,000
3.6
96.4
0.4
0.5
0.6
0.3
0.2
0.5
0.2
0.2
0.6
All Payers
$120,900
49.3
50.7
8.2
5.4
5.5
3.7
2.7
3.8
2.9
2.4
14.7
SOURCES: Authors’ tabulations from DYNASIM4, run id982.
NOTES: Estimates are reported in 2020 inflation-adjusted dollars.
A
ll Settings
Community-based (Includes residential care) Nursing Facility
A
ll Settings
Community-based (Includes r
esidential care)
Nursing Facility
RESEARCH BRIEF | 9
These figures mask important differences by income. People with lower incomes tend
to have more of their costs covered by Medicaid and pay less out of pocket. The
DYNASIM4 projections suggest that although Medicaid is used by older adults
throughout the age-65 income distribution, it primarily serves those in the bottom two
income quintiles (Table 8). For example, about 35% of people in the bottom income
quintile at age 65 and 23% of those in the second quintile will receive Medicaid LTSS at
some point after turning 65, compared with 6% in the top income quintile. Our
projections indicate that adults in upper income quintiles who use Medicaid are typically
individuals who have survived through their mid to late 90s, consistent with other
research (Borella et al. 2017; DeNardi et al. 2013).
TABLE 8. Projected Average and Distribution of Sum of Medicaid LTSS Expenditures
From Age 65 to Death for Adults Who Turn 65 in 2021-2025, by Income Quintile
Income Quintile at
Age 65
Average
Medicaid
Expenditures
Percent of
People with
Medicaid
Expenditures
Distribution of Sum of Medicaid LTSS Expenditures
(% of people)
None
<$10,000
$10,000-
$24,999
$25,000-
$49,999
$50,000-
$74,999
$75,000-
$99,999
$100,000-
$149,999
$150,000-
$199,999
$200,000-
$249,999
>$250,000
Lowest
108,400
35.4
64.6
4.4
2.8
2.4
1.7
1.7
3.6
2.4
2.1
14.3
Second
63,500
22.5
77.5
3.4
1.8
1.7
1.5
1.1
1.7
2.0
1.6
7.6
Middle
47,600
17.6
82.4
2.5
1.4
1.4
1.1
0.9
1.1
1.7
1.2
6.4
Fourth
21,400
9.3
90.7
1.2
0.3
1.4
0.6
0.4
0.9
0.8
0.7
3.1
Highest
14,000
5.7
94.3
0.4
0.4
0.4
0.4
0.6
0.6
0.4
0.2
2.3
All Quintiles
$51,800
18.3
81.7
2.4
1.4
1.5
1.1
1.0
1.6
1.5
1.2
6.8
SOURCES: Authors’ tabulations from DYNASIM4, run id982.
NOTES: Estimates are reported in 2020 inflation-adjusted dollars.
Family out-of-pocket expenditures, in contrast, are more concentrated within higher
income quintiles (Table 9). The average lifetime out-of-pocket LTSS expense in the top
quintile is $75,400, compared with $15,400 in the bottom quintile. Again, however, the
mean obscures important distributional information. About 10% of people in the top
income quintile at age 65 can expect to incur out-of-pocket expenses after turning age
65 that exceed $250,000. In the bottom half of the income distribution, where more
people are protected by Medicaid, the expected share with out-of-pocket spending that
exceeds $250,000 is less than 5%.
TABLE 9. Projected Average and Distribution of Sum of Family Out-of-Pocket LTSS Expenditures
from Age 65 to Death for Adults Turning 65 in 2021-2025, by Income Quintile
Income Quintile at
Age 65
Average
Out-of-Pocket
Expenditures
Percent of
People with
Out-of-Pocket
Expenditures
Distribution of Sum of Out-of-Pocket LTSS Expenditures
(% of people)
None
<$10,000
$10,000-
$24,999
$25,000-
$49,999
$50,000-
$74,999
$75,000-
$99,999
$100,000-
$149,999
$150,000-
$199,999
$200,000-
$249,999
>$250,000
Lowest
15,400
27.6
72.4
5.3
4.7
4.1
2.0
1.9
3.4
1.8
1.0
3.4
Second
34,200
32.9
67.1
6.2
4.5
4.2
4.4
2.3
3.8
1.9
1.2
4.4
Middle
43,200
34.7
65.3
6.1
4.8
4.7
3.5
1.5
3.9
2.0
1.9
6.3
Fourth
57,900
38.1
61.9
6.2
5.7
4.4
2.9
2.5
3.7
2.8
2.0
7.9
Highest
75,400
41.5
58.5
5.6
5.6
4.7
3.5
3.3
3.7
3.1
1.9
10.3
All Quintiles
$44,800
34.9
65.1
5.9
5.0
4.4
3.2
2.3
3.7
2.3
1.6
6.4
SOURCES: Authors’ tabulations from DYNASIM4, run id982.
NOTES: Estimates are reported in 2020 inflation-adjusted dollars.
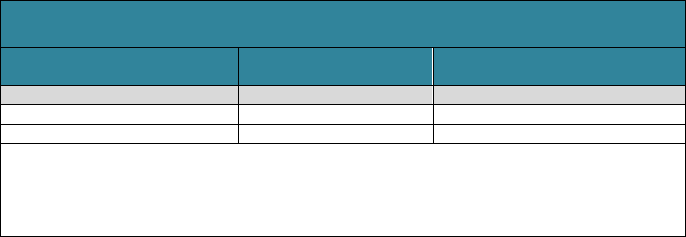
Many older adults with care needs receive substantial amounts of unpaid care from
family members and friends. Our projections indicate that the value of unpaid family
care received by adults born between 2021 and 2025 with significant disabilities
averages $91,900 (Table 10). Among people receiving unpaid family care, the average
value of care reaches $204,000, more than the value of all paid LTSS. Women receive
more unpaid care than men.
RESEARCH BRIEF | 10
TABLE 10. Projected Average Value of Unpaid Family Care from
Age 65 through Death for Adults Who Turn 65 in 2021-2025
All Adults
Adults Receiving Unpaid
Family Care
Total
$91,900
$204,000
Men
74,200
196,800
Women
108,600
208,800
SOURCES: Authors’ tabulations from DYNASIM4, run id982.
NOTES: Estimates are reported in 2020 inflation-adjusted dollars and restricted to care
received during periods of significant disability. Each hour of unpaid care is valued at the
median hourly wage for home care workers in the care recipient’s state of residence and
summed from age 65 to death.
Conclusion
Most Americans who survive to age 65 can expect to need and use LTSS. Our
estimates suggest more than half the population (56%) will have a significant level of
disability. On average, the projected duration of LTSS need is 3.1 years, and the
projected length of paid LTSS is just less than one year. The average cost of this care
is $120,900. However, a number of people can expect to need LTSS for many years
and to have care costs that total hundreds of thousands of dollars. Average long-term
care costs can be out of reach for many Americans. Medicaid is an important payer of
LTSS, but because it serves only those who meet strict income and asset criteria many
families pay for LTSS out of pocket. Private LTSS insurance has only a modest reach,
and it predominantly covers costs for those high in the income distribution. Other public
expenditures, such as U.S. Department of Veterans Affairs (VA) care, only help cover
small shares of the population with LTSS needs. The value of unpaid care provided by
family members and friends to people with significant disabilities exceeds the value of
paid care, and unpaid care is even more important when people have less severe
disability. Our results highlight the need for better planning for LTSS to accommodate
both average and catastrophic financial risks associated with chronic disability.
Differences from Earlier Projections
The results presented here differ from those reported in Favreault and Dey (2016).
Compared with the earlier version of our model, which generated Favreault and Dey’s
projections, our updated model projects longer average durations of LTSS needs (3.1
years versus 2.0 years), but the average time spend receiving LTSS does not differ
much between the two versions. The updated model also projects lower average LTSS
expenditures ($120,900 versus $138,100), especially for family out-of-pocket payments.
These differences result from some definitional changes between the two analyses and
numerous technical changes and updates.
An important substantive change between this brief and Favreault and Dey (2016) is
that we removed from our expected cost tables the incidental LTSS that Medicare
covers. As Box 1 discusses, Medicare generally does not pay for long-term care when
it is the only service a person needs. However, some people may have some of their
LTSS needs met through the course of receiving post-acute care. Given recent
Medicare payment rule changes, we expect that this type of overlap will be less
common in coming years.
RESEARCH BRIEF | 11
Much of the shift in the projections result from data updates and changes in the way we
specified model equations. We updated the DYNASIM starting sample to rely on later
panels of the Survey of Income and Program Participation. We also use more recent
state-specific price data (Genworth 2019, Hansen Hunter and Company 2018). Further,
we re-estimated many of the model parameters so that they use more recent data from
the Health and Retirement Study and other data sources. As we re-estimated some
parameters, we sometimes changed equation specification, which altered our
projections. These changes increased families’ sensitivity to costs when making LTSS
decisions, reducing some paid LTSS use by lower-income families, especially when
they would have to pay out of pocket. They also reduced service use at older ages.
When projecting the duration of LTSS needs, we now focus more on days in need
rather than years in need to better capture partial-year impairments. Additionally, we
removed some post-acute services from our LTSS estimates and improved our
algorithm of assigning costs to payers, which increased the significance of other public
payers, such as the VA and programs funded by the Older Americans Act.
In addition, the updated model improves our projections of severe cognitive impairment,
which partly determines the projected population with significant disabilities at risk of
receiving LTSS. We closely compare our dementia projections with the literature on the
distribution of the duration of impairment (for example, Brookmeyer et al. 2002, Larson
et al. 2004). Although the literature on cognitive impairment has been growing rapidly in
recent years, estimates on the length of time with a severe cognitive impairment is still
limited. As more data become available and this literature evolves, we will continue to
update these functions, given that dementia is such a significant driver of the need for
LTSS, and especially paid care.
Despite these differences, our substantive conclusions remain unchanged: older adults
face significant risk of needing LTSS, potentially incurring large out-of-pocket costs and
requiring unpaid help from family members.
End Notes
1. LTSS is also sometimes called long-term care.
2. Services may be provided in a person's home, in the community, or in residential
facilities (e.g., nursing homes or assisted living facilities) (Office of the Assistant
Secretary for Planning and Evaluation 2012).
3. Most LTSS is not medical care, but rather help with basic personal tasks of
everyday life. Medicare does not cover this LTSS (also called custodial care) if
that is the only care needed. Most nursing home care is custodial care. Medicare
does cover care in a hospital, skilled nursing care in a skilled nursing facility,
eligible home health services, and hospice and respite care.
RESEARCH BRIEF | 12
4. In a recent representative survey of Americans aged 40-70 conducted by GfK on
behalf of the Office of the Assistant Secretary for Planning and Evaluation at the
U.S. Department of Health and Human Services, only 25% of respondents
correctly identified Medicaid as the government program that pays the most for
LTSS in the United States.
5. The ADLs enumerated in the statute are eating, toileting, transferring, bathing,
dressing, and continence.
6. Throughout the brief we reference this level of need as “significant LTSS needs.”
7. DYNASIM4's LTSS projections draw information from a wide range of cross-
sectional and longitudinal sources, including the Health and Retirement Study,
Medicare Current Beneficiary Study, and National Health and Aging Trends
Survey.
8. Capturing trends in LTSS outcomes is challenging. When there is a clear trend,
such as the decline in mortality, DYNASIM4 follows the Social Security trustees'
assumptions. Otherwise, DYNASIM4 assumes that the underlying propensity to
develop LTSS needs or use LTSS continues at current levels, but that the
aggregate rates observed change as the composition of the population shifts. As
the population becomes better educated, for example, the model assigns the rates
for more highly educated adults to more people, but the rate for an adult with a
certain level of education does not change.
9. DYNASIM4 varies LTSS prices somewhat based on income, so that some lower-
income families use lower-cost providers--especially for home care--and some
higher-income families--especially those covered by LTCI--use higher-cost
providers.
10. Multiple cohorts are used to provide a sample that is large enough for
subpopulation analysis.
11. We define income quintile by income relative to the federal poverty level. This
measure recognizes that married couples need more resources than single adults
but acknowledges that shared living arrangements allow couples to economize, so
a couple needs less than twice as much as a single adult. The measure includes
earnings, pensions, Social Security, Supplemental Security Income, and asset
income (defined as the annuitized value of financial assets) received by individuals
and, if married, their spouses.
12. Use of unpaid services is substantial at both the HIPAA and non-HIPAA disability
levels, while use of paid services is more concentrated at the HIPPA level.

RESEARCH BRIEF | 13
13. Dollar amounts are rounded to the nearest $100, reflecting the inherent uncertainty
surrounding the projections. PDV estimates, which are reported in Tables A1-A9,
use the Social Security trustees' ultimate real interest rate of 2.5%. Because the
trustees assume long-range price growth averages 2.6%, this real discount rate is
equivalent to a nominal long-run discount rate of about 5.1%.
14. We restrict our cost estimates to people with significant disabilities, except that we
count nursing home care costs regardless of a resident’s disability status and we
count residential care costs for residents who report difficulty with at least two
ADLs (or are severely cognitively impaired), instead of requiring them to need
assistance with two or more ADLs. Because our cost estimates use a somewhat
less stringent disability requirement than our estimates of the receipt of paid LTSS,
our projection of the share of older adults with LTSS expenditures slightly exceeds
our projection of the share who receive any paid LTSS (49.3% in Table 7 versus
45.3% in Table 2).
15. The relative share of costs borne by different payers is sensitive to whether and
how residential care is incorporated into these projections. Some researchers
exclude from LTSS cost estimates the housing component of residential care,
which is included in our estimates. The NHEA exclude some related sectors
completely (Hartman, Kornfeld and Catlin 2010). Removing the housing
component of residential care or removing residential care completely reduces out-
of-pocket costs and families’ share of spending.
References
Board of Trustees, Federal Old-Age and Survivors Insurance and Federal Disability
Insurance Trust Funds (2021). 2021 Annual Report of the Board of Trustees of the
Federal Old-Age and Survivors Insurance and Federal Disability Insurance Trust Funds.
Washington, DC: Government Printing Office.
Boards of Trustees, Federal Hospital Insurance and Federal Supplementary Medical
Insurance Trust Funds (2019). 2019 Annual Report of the Boards of Trustees of the
Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds.
Washington, DC.
Borella M, De Nardi M, and French E (2017). Who Receives Medicaid in Old Age?
Rules and Reality. Fiscal Studies, 39(1): 65-93.
Brookmeyer R, Corrada M, Curriero F, and Kawas C (2002). Survival Following a
Diagnosis of Alzheimer’s Disease. Archives of Neurology, 59: 1764-1767.
Centers for Medicare & Medicaid Services (2015). Your Medicare Coverage: Long-Term
Care. Baltimore, MD: U.S. Department of Health and Human Services.
http://www.medicare.gov/coverage/long-term-care.html (accessed April 29, 2015).
RESEARCH BRIEF | 14
Cohen MA (2016). The State of the Long-Term Care Insurance Market. In Nordman,
EC. The State of Long-Term Care Insurance: The Market, Challenges and Future
Innovations. Kansas City, MO: National Association of Insurance Commissioners and
Center for Insurance Policy Research.
Colello KJ (2022). Who Pays for Long-Term Services and Supports? Washington, DC:
Congressional Research Service.
DeNardi M, French E, and Baily Jones J (2013). Medicaid Insurance in Old Age.
Working Paper 2012-2013. Chicago, IL: Federal Reserve Bank of Chicago.
Doty P (2017). Private Pay Home Care: New Models of Access and Service Delivery.
Public Policy and Aging Report 27(3): 111-120. doi:10.1093/ppar/prx021
Favreault M, and Dey J (2016). Long-Term Services and Supports for Older Americans:
Risks and Financing. Washington, DC: U.S. Department of Health and Human Services,
Office of the Assistant Secretary for Planning and Evaluation. http://aspe.hhs.gov/basic-
report/long-term-services-and-supports-older-americans-risks-and-financing-research-
brief.
Fossett J, and Burke C (2010). Medicaid Policy and Long-Term Care Spending: An
Interactive View. Albany, NY: Rockefeller Institute.
Freedman VA and Spillman BC (2014). Disability and Care Needs among Older
Americans. Milbank Quarterly, 92(3): 509-541.
Freundlich N (2014). Long-Term Care: What are the Issues? Princeton, NJ: Robert
Wood Johnson Foundation.
Genworth (2019). Cost of Care Survey, 2019: Median Cost Data Tables.
https://pro.genworth.com/riiproweb/productinfo/pdf/282102.pdf.
Grabowski D, Feng Z, Intrator O, and Mor V (2004). Recent Trends in State Nursing
Home Payment Policies. Health Affairs, 23(1).
Hado E, and Komisar H (2019). Long-Term Services and Supports. Washington, DC:
AARP Public Policy Institute. https://www.aarp.org/content/dam/aarp/ppi/2019/08/long-
term-services-and-supports.doi.10.26419-2Fppi.00079.001.pdf.
Hagen S (2013). Rising Demand for Long-Term Services and Supports for Elderly
People. Washington, DC: Congressional Budget Office.
Hansen Hunter and Company PC (2018). A Report on Shortfalls in Medicaid Funding
for Nursing Center Care. Washington, DC: American Health Care Association.
https://www.ahcancal.org/facility_operations/medicaid/Documents/2017%20Shortfall%2
0Methodology%20Summary.pdf.
RESEARCH BRIEF | 15
Hartman MB, Kornfeld RJ, and Catlin AC (2010). A Reconciliation of Health Care
Expenditures in the National Health Expenditures Accounts and in Gross Domestic
Product. Suitland, MD: US Bureau of Economic Analysis.
https://apps.bea.gov/scb/pdf/2010/09%20September/0910_healthcare.pdf.
HomecarePulse (2019). Homecare Benchmarking Study 2019, Spring Edition. Rexburg,
ID.
Johnson R (2019). What Is the Lifetime Risk of Needing and Receiving Long-Term
Services and Supports? Washington, DC: U.S. Department of Health and Human
Services, Office of the Assistant Secretary for Planning and Evaluation.
https://aspe.hhs.gov/basic-report/what-lifetime-risk-needing-and-receiving-long-term-
services-and-supports.
Johnson R (2022). Projections of the Risk of Long-Term Services and Supports at Ages
65 and Older. Report to ASPE. Washington, DC: Urban Institute.
Kane J (2013). PBS Newshour: Americans Seriously Unprepared for Long-Term Care,
Survey Finds. http://www.pbs.org/newshour/rundown/as-boomers-age-most-woefully-
unprepared-for-long-term-care/ (accessed May 5, 2015).
Katz S, Ford AB, Moskowitz RW, Jackson BA, and Jaffe MW (1963). Studies of Illness
in the Aged: The Index of ADL: A Standardized Measure of Biological and Psychosocial
Function. JAMA, 185(12): 914-919. doi:10.1001/jama.1963.03060120024016.
Kemper P, Komisar HL, and Alecxih L (2005/2006). Long-term Care over an Uncertain
Future: What Can Current Retirees Expect? Inquiry, 42: 335-350.
Kim JJ (2022). Personal Care Aides as Household Employees and Independent
Contractors: Estimating the Size and Characteristics of the Workforce. Innovations in
Aging, 6(1): 1-10.
Komisar H (2013). AARP Thinking Policy. http://blog.aarp.org/2013/08/22/medicare-
does-not-pay-for-long-term-care/ (accessed April 29, 2015).
Larson EB, Shadlen M-F, Wang L, McCormick WC, Bowen JD, Teri L, and Kukull WA
(2004). Survival after Initial Diagnosis of Alzheimer Disease. Annals of Internal
Medicine, 140(7): 501-511.
Mollica R (2009). State Medicaid Reimbursement Policies and Practices in Assisted
Living. National Center for Assisted Living, American Health Care Association.
National Association of Insurance Commissioners (2019). Long-Term Care Insurance
Experience Reports for 2018. Washington, DC: National Association of Insurance
Commissioners. https://naic.org/prod_serv/LTC-LR-19.pdf.
RESEARCH BRIEF | 16
Newquist DD, DeLiema M, and Wilber KH (2015). Beware of Data Gaps in Home Care
Research: The Streetlight Effect and Its Implications for Policy Making on Long-Term
Services and Supports. Med Care Res Rev, 72(5): 622-640.
doi:10.1177/1077558715588437.
Ng T, Harrington C, Musumeci M, and Reaves E (2014). Medicaid Home and
Community-Based Services Programs: 2010 Data Update. Menlo Park, CA: Kaiser
Commission on Medicaid and the Uninsured.
Office of the Assistant Secretary for Planning and Evaluation (2012). Glossary of Terms.
Washington, DC: U.S. Department of Health and Human Services, Office of the
Assistant Secretary for Planning and Evaluation. https://aspe.hhs.gov/glossary-terms
(accessed May 1, 2015).
Scism L (2015). Long-term Care Insurance: Is it Worth it? Wall Street Journal.
Schmitz A, and Giese C (2019). Is Insurance the Answer to the Long-Term-Care
Financing Challenge? Generations, 43(1): 86-88.
Stallard E (2011). Estimates of the Incidence, Prevalence, Duration, Intensity and Cost
of Chronic Disability among the U.S. Elderly. North American Actuarial Journal, 15(1):
32-58.
Tompson T, Benz J, Junius A, Nguyen K, and Lowell K (2013). Long-Term Care:
Perceptions, Experiences and Attitudes among Americans 40 or Older. Research
Highlights. Chicago: Associated Press-NORC Center for Public Affairs Research.
Ujvari K (2018). Disrupting the Marketplace: The State of Private Long-Term Care
Insurance, 2018 Update. Washington, DC: AARP Public Policy Institute.
https://www.aarp.org/content/dam/aarp/ppi/2018/08/disrupting-the-marketplace-the-
state-of-private-long-term-care-insurance.pdf.
U.S. Department of Health and Human Services (US DHHS) (2015).
LongTermCare.gov. http://longtermcare.gov/medicare-medicaid-
more/medicaid/medicaid-eligibility/ (accessed May 1, 2015).
VanDerhei J (2015). Retirement Savings Shortfalls: Evidence from EBRI's Retirement
Security Projection Model. Issue Brief. Washington, DC: Employee Benefit Research
Institute.
Warshawsky M (2014). Millionaires on Medicaid. Wall Street Journal.
Wiener J, Khatutsky G, Thach N, and Greene A (2015). What Americans Think About
Long-Term Care. Washington, DC: U.S. Department of Health and Human Services,
Office of the Assistant Secretary for Planning and Evaluation.
RESEARCH BRIEF | 17
Appendix: Projections of LTSS Expenditures Using a Present
Discounted Value Measure
TABLE A1. Projected PDV of Expenditures from Age 65 through Death
for Adults Who Turn 65 in 2021-2025, byPayer and Setting
Payer
All Settings
Community-Based
(includes residential care)
Nursing Facility
Dollars
Percentage
of total
Dollars
Percentage
of total
Dollars
Percentage
of total
Public
$42,200
60
$17,400
53
$24,800
67
Medicaid
31,500
45
12,400
38
19,100
52
Other Public
10,700
15
5,000
15
5,700
15
Private
$27,600
40
$15,600
47
$12,100
33
Out-of-Pocket
24,000
34
12,800
39
11,300
31
Private Insurance
3,600
5
2,800
8
800
2
All Payers
$69,800
100
$33,000
100
$36,900
100
SOURCES: Authors’ tabulations from DYNASIM4, run id982.
NOTES: PDV = present discounted value. Estimates are reported in 2020 inflation-adjusted dollars. We use a real discount rate
of 2.5% (5.1% nominal) in these calculations. Residential care is included in community-based care, not nursing-facility care.
LTSS prices are state- and setting-specific, based on Genworth (2019), Hansen Hunter and Company PC (2018), and other
sources. Nursing home and residential care prices are adjusted for wage inflation; home care prices grow with the average of
wage and price inflation. Components do not always sum to totals because of rounding.
TABLE A2. Projected PDV of Expenditures from Age 65 through Death
for Adults Who Turn 65 in 2021-2025 and Use Paid LTSS, by Payer and Setting
Payer
All Settings
Community-Based
(includes residential care)
Nursing Facility
Average ($)
Percentage
of total
Average ($)
Percentage
of total
Average ($)
Percentage
of total
Public
$83,700
59
$33,300
50
$50,300
67
Medicaid
62,200
44
23,400
35
38,700
52
Other Public
21,500
15
9,900
15
11,600
16
Private
$58,100
41
$33,600
50
$24,600
33
Out-of-Pocket
50,800
36
28,000
42
22,900
31
Private Insurance
7,300
5
5,600
8
1,700
2
All Payers
$141,700
100
$66,900
100
$74,800
100
SOURCES: Authors’ tabulations from DYNASIM4, run id982.
NOTES: PDV = present discounted value. Estimates are reported in 2020 inflation-adjusted dollars. We use a real discount rate
of 2.5% (5.1% nominal) in these calculations. Residential care is included in community-based care, not nursing-facility care.
LTSS prices are state- and setting-specific, based on Genworth (2019), Hansen Hunter and Company PC (2018), and other
sources. Nursing home and residential care prices are adjusted for wage inflation; home care prices grow with the average of
wage and price inflation. Components do not always sum to totals because of rounding.
TABLE A3. Projected PDV of Expenditures from Age 65 through Death
for Women Who Turn 65 in 2021-2025, by Payer and Setting
Payer
All Settings
Community-Based
(includes residential care)
Nursing Facility
Average ($)
Percentage
of total
Average ($)
Percentage
of total
Average ($)
Percentage
of total
Public
$52,800
61
$21,000
52
$31,900
69
Medicaid
40,400
47
15,100
37
25,300
55
Other Public
12,400
14
5,900
15
6,600
14
Private
$34,000
39
$19,400
48
$14,600
31
Out-of-Pocket
29,500
34
15,800
39
13,700
30
Private Insurance
4,500
5
3,600
9
900
2
All Payers
$86,800
100
$40,400
100
$46,400
100
SOURCES: Authors’ tabulations from DYNASIM4, run id982.
NOTES: PDV = present discounted value. Estimates are reported in 2020 inflation-adjusted dollars. We use a real discount rate of
2.5% (5.1% nominal) in these calculations. Residential care is included in community-based care, not nursing-facility care. LTSS
prices are state- and setting-specific, based on Genworth (2019), Hansen Hunter and Company PC (2018), and other sources.
Nursing home and residential care prices are adjusted for wage inflation; home care prices grow with the average of wage and price
inflation.
All Settings
All Settings
All Settings
Community Based Includes
Residential Car
e
Community Based Includes Res
idential Care
Community Based includes residential Care
Nursing Facility
Nursing Facility
Nursing Facility
RESEARCH BRIEF | 18
TABLE A4. Projected PDV of Expenditures from Age 65 through Death
for Women Who Turn 65 in 2021-2025 and Use Paid LTSS, by Payer and Setting
Payer
All Settings
Community-Based
(includes residential care)
Nursing Facility
Average ($)
Percentage
of total
Average ($)
Percentage
of total
Average ($)
Percentage
of total
Public
$93,000
60
$35,700
49
$57,300
69
Medicaid
70,900
45
25,400
35
45,500
54
Other Public
22,100
14
10,300
14
11,800
14
Private
$63,200
40
$37,100
51
$26,200
31
Out-of-Pocket
55,100
35
30,500
42
24,600
29
Private Insurance
8,100
5
6,600
9
1,600
2
All Payers
$156,300
100
$72,800
100
$83,500
100
SOURCES: Authors’ tabulations from DYNASIM4, run id982.
NOTES: PDV = present discounted value. Estimates are reported in 2020 inflation-adjusted dollars. We use a real discount rate
of 2.5% (5.1% nominal) in these calculations. Residential care is included in community-based care, not nursing-facility care.
LTSS prices are state- and setting-specific, based on Genworth (2019), Hansen Hunter and Company PC (2018), and other
sources. Nursing home and residential care prices are adjusted for wage inflation; home care prices grow with the average of
wage and price inflation.
TABLE A5. Projected PDV of Expenditures from Age 65 through Death
for Men Turning 65 in 2021-2025, by Payer and Setting
Payer
All Settings
Community-Based
(includes residential care)
Nursing Facility
Average ($)
Percentage
of total
Average ($)
Percentage
of total
Average ($)
Percentage
of total
Public
$30,900
60
$13,700
55
$17,300
65
Medicaid
22,000
43
9,600
38
12,500
47
Other Public
8,900
17
4,100
16
4,800
18
Private
$20,800
40
$11,300
45
$9,500
35
Out-of-Pocket
18,200
35
9,500
38
8,700
32
Private Insurance
2,600
5
1,800
7
800
3
All Payers
$51,700
100
$25,000
100
$26,800
100
SOURCES: Authors’ tabulations from DYNASIM4, run id982.
NOTES: PDV = present discounted value. Estimates are reported in 2020 inflation-adjusted dollars. We use a real discount rate of
2.5% (5.1% nominal) in these calculations. Residential care is included in community-based care, not nursing-facility care. LTSS
prices are state- and setting-specific, based on Genworth (2019), Hansen Hunter and Company PC (2018), and other sources.
Nursing home and residential care prices are adjusted for wage inflation; home care prices grow with the average of wage and price
inflation.
TABLE A6. Projected PDV of Expenditures from Age 65 through Death
for Men Who Turn 65 in 2021-2025 and Use Paid LTSS, by Payer and Setting
Payer
All Settings
Community-Based
(includes residential care)
Nursing Facility
Average ($)
Percentage
of total
Average ($)
Percentage
of total
Average ($)
Percentage
of total
Public
$70,500
58
$30,000
51
$40,600
65
Medicaid
49,900
41
20,700
35
29,300
47
Other Public
20,600
17
9,300
16
11,300
18
Private
$51,000
42
$28,700
49
$22,300
36
Out-of-Pocket
44,900
37
24,400
42
20,500
33
Private Insurance
6,100
5
4,300
7
1,800
3
All Payers
$121,500
100
$58,600
100
$62,800
100
SOURCES: Authors’ tabulations from DYNASIM4, run id982.
NOTES: PDV = present discounted value. Estimates are reported in 2020 inflation-adjusted dollars. We use a real discount rate
of 2.5% (5.1% nominal) in these calculations. Residential care is included in community-based care, not nursing-facility care.
LTSS prices are state- and setting-specific, based on Genworth (2019), Hansen Hunter and Company PC (2018), and other
sources. Nursing home and residential care prices are adjusted for wage inflation; home care prices grow with the average of
wage and price inflation.
All Settings
All Settings
All Settings
Community Based Includes residential care
Community
based includes residential care
Community Based includes residential care
Nurs
ing facility
Nursing Facility
Nursing Facility
RESEARCH BRIEF | 19
TABLE A7. Projected Average and Distribution of PDV of LTSS Expenditures from Age 65 through Death
for Adults Who Turn 65 in 2021-2025, by Payer
Payer
Average
Expenditures
Percent of
People with
Expenditures
Distribution of PDV of LTSS Expenditures
(% of people)
None
<$10,000
$10,000-
$24,999
$25,000-
$49,999
$50,000-
$74,999
$75,000-
$99,999
$100,000-
$149,999
$150,000-
$199,999
$200,000-
$249,999
>$250,000
Public
$42,200
Medicaid
31,500
18.3
81.7
3.0
1.8
1.7
1.5
1.3
1.9
1.6
1.2
4.3
Other Public
10,700
40.9
59.1
17.3
10.2
7.4
2.9
1.3
1.2
0.4
0.1
0.1
Private
$27,600
Out-of-Pocket
24,000
35.5
65.2
8.3
5.6
5.7
3.3
2.8
3.3
2.0
1.3
2.5
Private Insurance
3,600
3.6
96.4
0.6
0.7
0.6
0.5
0.3
0.3
0.2
0.1
0.4
All Payers
$69,800
49.3
50.7
10.4
6.4
6.9
3.7
3.2
4.3
3.0
2.4
9.0
SOURCES: Authors’ tabulations from DYNASIM4, run id982.
NOTES: PDV = present discounted value. Estimates are reported in 2020 inflation-adjusted dollars. We use a real discount rate of 2.5% (5.1%
nominal) in these calculations.
TABLE A8. Projected Average and Distribution of PDV of Medicaid LTSS Expenditures
from Age 65 to Death for Adults Who Turn 65 in 2021-2025, by Income Quintile
Income Quintile at
Age 65
Average
Expenditures
Percent of
People with
Expenditures
Distribution of PDV of LTSS Expenditures
(% of people)
None
<$10,000
$10,000-
$24,999
$25,000-
$49,999
$50,000-
$74,999
$75,000-
$99,999
$100,000-
$149,999
$150,000-
$199,999
$200,000-
$249,999
>$250,000
Lowest
71,625
35.4
64.6
5.4
2.8
3.2
2.4
2.8
3.6
2.3
2.7
10.2
Second
37,433
22.5
77.5
4.5
2.0
2.0
1.8
1.8
2.3
1.9
0.8
5.3
Middle
27,378
17.6
82.4
3.1
1.8
1.7
1.6
1.0
1.8
1.5
1.4
3.7
Fourth
11,463
9.3
90.7
1.2
1.5
0.9
1.0
0.5
1.2
1.3
0.5
1.1
Highest
6,904
5.7
94.3
0.5
0.6
0.8
0.8
0.4
0.6
0.8
0.5
0.7
All Quintiles
$31,517
18.3
81.7
3.0
1.8
1.7
1.5
1.3
1.9
1.6
1.2
4.3
SOURCES: Authors’ tabulations from DYNASIM4, run id982.
NOTES: PDV = present discounted value. Estimates are reported in 2020 inflation-adjusted dollars. We use a real discount rate of 2.5% (5.1%
nominal) in these calculations.
TABLE A9. Projected Average and Distribution of PDV of Family Out-of-Pocket LTSS Expenditures
From Age 65 to Death for Adults Turning 65 in 2021-2025, by Income Quintile
Income Quintile at
Age 65
Average
Expenditures
Percent of
People with
Expenditures
Distribution of PDV of LTSS Expenditures
(% of people)
None
<$10,000
$10,000-
$24,999
$25,000-
$49,999
$50,000-
$74,999
$75,000-
$99,999
$100,000-
$149,999
$150,000-
$199,999
$200,000-
$249,999
>$250,000
Lowest
6,021
28.9
72.5
7.1
5.4
4.2
2.8
2.3
2.5
1.7
0.9
0.6
Second
19,057
33.7
67.2
8.1
5.2
6.9
3.0
2.8
2.8
1.2
1.2
1.5
Middle
24,000
34.9
65.3
8.4
5.3
6.0
3.2
2.3
3.2
2.5
1.2
2.5
Fourth
31,577
38.5
61.9
9.6
5.4
5.3
3.7
3.3
3.5
2.4
2.2
2.7
Highest
40,737
42.0
58.5
8.2
6.7
6.3
3.9
3.1
4.6
2.4
1.2
5.0
All Quintiles
$24,029
35.5
65.2
8.3
5.6
5.7
3.3
2.8
3.3
2.0
1.3
2.5
SOURCES: Authors’ tabulations from DYNASIM4, run id982.
NOTES: PDV = present discounted value. Estimates are reported in 2020 inflation-adjusted dollars. We use a real discount rate of 2.5% (5.1%
nominal) in these calculations.
RESEARCH BRIEF | 20
This Research Brief, authored by Richard W. Johnson (Urban Institute) and Judith Dey (U.S. Department
of Health and Human Services), presents information about the risk of needing care and associated costs
to provide content for policymakers and others considering long-term care financing proposals.
The LTSS projections in DYNASIM4 were originally developed by Melissa Favreault when she was a
senior fellow at the Urban Institute. Her microsimulation skills, deep knowledge of long-term care policy,
and hard work made this brief possible. We are indebted to her leadership and insights.
The authors also gratefully acknowledge conceptual and modeling help from Owen Haaga, Paul Johnson,
and Brenda Spillman and valuable comments and advice from Lauren Anderson, Chris Giese, Harriet
Komisar, William Marton, Al Schmitz, Brenda Spillman, Anne Tumlinson, and the late Joshua Wiener.
Many advisory panel members and seminar participants helped refine our projections. This remains work
in progress that we will update regularly as new data become available.
This brief was prepared under contract #HHSP233201600024I between HHS’s ASPE/BHDAP and the
Urban Institute. For additional information about this subject, visit the BHDAP home page at
https://aspe.hhs.gov/bhdap or contact the ASPE Project Officers, at HHS/ASPE/BHDAP, Room 424E,
H.H. Humphrey Building, 200 Independence Avenue, S.W., Washington, D.C., 20201;
The opinions and views expressed in this report are those of the authors. They do not reflect the views of
the Department of Health and Human Services or Urban Institute.
