
SELECT COMMITTEE ON THE PROVISIONS OF THE PUBIC HEALTH
AMENDMENT (REGISTERED NURSES IN NURSING HOMES) BILL 2020
LEGISLATIVE COUNCIL
Provisions of the Public Health
Amendment (Registered Nurses in
Nursing Homes) Bill 2020
Discussion paper
www.parliament.nsw.gov.auwww.parliament.nsw.gov.au
February 2021February 2021

LEGISLATIVE COUNCIL
Discussion paper - February 2021 i
Select Committee on the Provisions of the Public Health
Amendment (Registered Nurses in Nursing Homes) Bill 2020
Provisions of the Public
Health Amendment
(Registered Nurses in
Nursing Homes) Bill 2020
Discussion paper
Ordered to be printed according to Standing Order 226(4).

LEGISLATIVE COUNCIL
Provisions of the Public Health Amendment (Registered Nurses in Nursing Homes) Bill 2020
ii Discussion paper - February 2021
New South Wales Parliamentary Library cataloguing-in-publication data:
New South Wales. Parliament. Legislative Council. Select Committee on the Provisions of the
Public Health Amendment (Registered Nurses in Nursing Homes) Bill 2020.
Discussion paper: Provisions of the Public Health Amendment (Registered Nurses in Nursing Homes)
Bill 2020 / Select Committee on the Provisions of the Public Health Amendment (Registered Nurses in
Nursing Homes) Bill 2020. [Sydney, N.S.W.] : the Committee, 2021. – [19] pages ; 30 cm. (Report)
Chair: Hon. Courtney Houssos, MLC.
“February 2021”
ISBN 9781922543035
1. New South Wales. Parliament. Legislative Council— Public Health Amendment (Registered
Nurses in Nursing Homes) Bill 2020.
2. Nurses—Supply and demand—New South Wales.
3. Nurses—Certification—New South Wales.
4. Nursing homes—New South Wales.
I. Title
II. Houssos, Courtney.
III. Series: New South Wales. Parliament. Legislative Council. Select Committee on the Provisions
of the Public Health Amendment (Registered Nurses in Nursing Homes) Bill 2020. Report.
610.7306909944 (DDC22)
SELECT COMMITTEE ON THE PROVISIONS OF THE PUBLIC HEALTH AMENDMENT (REGISTERED NURSES IN
NURSING HOMES) BILL 2020
Discussion paper - February 2021 iii
Table of contents
Terms of reference iv
Committee details v
Chapter 1 Discussion paper 1
Introduction 1
Legislative framework for aged care in New South Wales 1
Federal legislation 1
New South Wales legislation 4
The interaction between federal and New South Wales legislation on the requirement
for registered nurses in nursing homes 5
Proposed federal reforms 6
Royal Commission into Aged Care Quality and Safety 8
Key themes 8
Staffing issues 9
2015 inquiry into registered nurses in nursing homes 12
Appendix 1 2015 inquiry into registered nurses in nursing homes recommendations and
government response 15

LEGISLATIVE COUNCIL
Provisions of the Public Health Amendment (Registered Nurses in Nursing Homes) Bill 2020
iv Discussion paper - February 2021
Terms of reference
1. That a select committee be established to inquire into and report on the provisions of the Public
Health Amendment (Registered Nurses in Nursing Homes) Bill 2020, and in particular:
(a) the need to have a registered nurse on duty at all times in nursing homes and other aged care
facilities with residents who require a high level of residential care,
(b) the impact registered nurses have on the safety and dignity of people in care,
(c) the impact on residential care of a lack of registered nursing staff on duty in a nursing home
or other aged care facility at all times,
(d) the need for further regulation and minimum standards of care and appropriate staffing levels
in nursing homes and other aged care facilities,
(e) the administration, procurement, storage and recording of medication by non-registered
nurses in nursing homes and other aged care facilities with residents who require a high level
of residential care, as compared with hospital clinical settings,
(f) the potential for cost-shifting onto other parts of the public health system as a result of any
legislative change to the current provisions for care in nursing homes or other aged care
facilities,
(g) the role of registered nurses in responding to critical incidents and preventing unnecessary
hospital admissions and unnecessary ambulance call outs and the consequent effect of this
upon the provision of ambulance services to the wider community,
(h) the lessons that can be learnt in New South Wales from the impact of the COVID-19 crisis
on private aged care facilities where staffing ratios are not mandated, and
(i) any other related matter.
The terms of reference were referred to the committee by the Legislative Council on Wednesday
21 October 2020.
1
1
Minutes, NSW Legislative Council, Wednesday 21 October 2020, pp 1484-1486.
SELECT COMMITTEE ON THE PROVISIONS OF THE PUBLIC HEALTH AMENDMENT (REGISTERED NURSES IN
NURSING HOMES) BILL 2020
Discussion paper - February 2021 v
Committee details
Committee members
The Hon Courtney Houssos MLC
Australian Labor Party
Chair
The Hon Mark Banasiak MLC
Shooters, Fishers and Farmers Party
Deputy Chair
The Hon Greg Donnelly MLC
Australian Labor Party
Ms Cate Faehrmann MLC*
The Greens
The Hon Wes Fang MLC
The Nationals
The Hon Natasha Maclaren-Jones MLC
Liberal Party
The Hon Taylor Martin MLC
Liberal Party
The Hon Daniel Mookhey MLC
Australian Labor Party
The Hon Mark Pearson MLC
Animal Justice Party
* Ms Cate Faehrmann MLC substituted for Ms Abigail Boyd MLC from 20 January 2021 for the
duration of the inquiry.
Contact details
Website
www.parliament.nsw.gov.au
Email
Telephone
9230 3067

LEGISLATIVE COUNCIL
Provisions of the Public Health Amendment (Registered Nurses in Nursing Homes) Bill 2020
vi Discussion paper - February 2021

SELECT COMMITTEE ON THE PROVISIONS OF THE PUBLIC HEALTH AMENDMENT (REGISTERED NURSES IN
NURSING HOMES) BILL 2020
Discussion paper - February 2021 1
Discussion paper
Introduction
1.1 The Select Committee on the Provisions of the Public Health Amendment (Registered Nurses
in Nursing Homes) Bill 2020 was established by the House on 21 October 2020. The terms of
reference can be found on p iv.
1.2 The object of the Public Health Amendment (Registered Nurses in Nursing Homes) Bill 2020
is to ensure that the requirement in New South Wales for a registered nurse to be on duty in a
nursing home at all times is continued, by updating the definition of nursing home so that it is
consistent with the terminology used under federal legislation.
1.3 This discussion paper provides background to the inquiry and aims to assist witnesses ahead of
hearings to be held in February and March 2021.
1.4 The paper first provides an overview of the legislative framework governing aged care in New
South Wales. In particular, it sets out how the federal legislation affects the operation of the
state requirement for a registered nurse to be on duty in a nursing home at all times. The paper
then provides a summary of the key themes arising from the Royal Commission into Aged Care
Quality and Safety with a focus on staffing issues. Finally, the paper provides an overview of
the recommendations of and government response to the 2015 inquiry into registered nurses in
nursing homes conducted by the NSW Legislative Council General Purpose Standing
Committee No. 3.
Legislative framework for aged care in New South Wales
1.5 Aged care is a federal responsibility in Australia, with the Australian Government primarily
responsible for its funding and regulation. In New South Wales, residential aged care facilities
are also subject to state legislation, including public health laws and laws governing the
dispensation of medicine.
1.6 This section sets out the federal and New South Wales legislation in relation to aged care, and
how the two legislative frameworks interact.
Federal legislation
1.7 At the federal level, the Aged Care Act 1997 (Cth), Aged Care Quality and Safety Commission Act
2018 (Cth) and Aged Care Principles provide the legislative framework for the funding and
regulation of aged care. The Aged Care Act sets out the requirements for the approval of
providers, quality of care and the rights of people receiving care, and applies to the states and
territories.

LEGISLATIVE COUNCIL
Provisions of the Public Health Amendment (Registered Nurses in Nursing Homes) Bill 2020
2 Discussion paper - February 2021
1.8 The term 'aged care' is defined in the Aged Care Act as including residential care, home care, and
flexible care. Section 41-3 defines 'residential care' as personal and/or nursing care that is
provided in a residential facility. The section also clarifies what is not considered to be residential
care:
(1)
Residential care
is personal care or nursing care, or both personal care and nursing
care, that:
(a) is provided to a person in a residential facility in which the person is also
provided with accommodation that includes:
(i) appropriate staffing to meet the nursing and personal care needs
of the person; and
(ii) meals and cleaning services; and
(iii) furnishings, furniture and equipment for the provision of that care
and accommodation; and
(b) meets any other requirements specified in the Subsidy Principles.
(2) However, residential care does not include any of the following:
(a) care provided to a person in the person’s private home;
(b) care provided in a hospital or in a psychiatric facility;
(c) care provided in a facility that primarily provides care to people who are
not frail and aged;
(d) care that is specified in the Subsidy Principles not to be residential care.
1.9 Under section 3-1, the Australian Government provides financial support through the payment
of subsidies for the provision of aged care, as well as relevant grants. The process for the
allocation of aged care places is set out in section 11-1 of the Aged Care Act:
An approved provider can only receive *subsidy for providing residential care or flexible
care in respect of which a *place has been allocated. The Commonwealth plans the
distribution between *regions of the available places in respect of the types of subsidies.
It then invites applications and allocates the places to approved providers.
1.10 The Act also sets out the responsibility of approved providers in chapter 4. These concern:
the quality of care provided
user rights for those who receive care
accountability for the care that is provided and for the suitability of key personnel.
1.11 In particular, section 54-1 of the Aged Care Act establishes the responsibilities of approved
providers in relation to the quality of aged care. Section 54-1(b) requires that providers ‘maintain
an adequate number of appropriately skilled staff to ensure that the care needs of care recipients
are met’.

SELECT COMMITTEE ON THE PROVISIONS OF THE PUBLIC HEALTH AMENDMENT (REGISTERED NURSES IN
NURSING HOMES) BILL 2020
Discussion paper - February 2021 3
1.12 Subordinate to the Aged Care Act are 17 legislative instruments known as the Aged Care
Principles, including the Quality of Care Principles 2014 and the User Rights Principles 2014. The
Aged Care Principles provide further detail on the rules for government-funded aged care
including: funding; regulation; approval of providers; subsidies and fees; standards; quality of
care; rights of people receiving care; and non-compliance. These regulatory arrangements apply
to all approved providers operating under the Aged Care Act.
1.13 Approved providers must also comply with eight Aged Care Quality Standards: consumer
dignity and choice; ongoing assessment and planning with consumers; personal care and clinical
care; services and support for daily living; organisation’s service environment; feedback and
complaints; human resources; and organisational governance.
1.14 All aged care services funded by the Australian Government must meet the Aged Care Quality
Standards to qualify for funding. Each quality standard includes a statement of the outcome to
be realised for the consumer, expectations of the provider and requirements to be achieved.
Human resources are the focus of Standard 7 which requires that: 'The organisation has a
workforce that is sufficient, and is skilled and qualified to provide safe, respectful and quality
care and services.'
2
1.15 As a result, individuals are to receive quality care and services when needed ‘from people who
are knowledgeable, capable and caring’.
3
In order to deliver this outcome, a number of
requirements are specified:
a. The workforce is planned to enable, and the number and mix of members of the
workforce deployed enables, the delivery and management of safe and quality care and
services.
b. Workforce interactions with consumers are kind, caring and respectful of each
consumer’s identity, culture and diversity.
c. The workforce is competent and members of the workforce have the qualifications
and knowledge to effectively perform their roles.
d. The workforce is recruited, trained, equipped and supported to deliver the outcomes
required by these standards.
e. Regular assessment, monitoring and review of the performance of each member of
the workforce.
4
1.16 It is important to note that the federal legislative framework does not currently mandate
minimum staffing levels for residential aged care.
2
Australian Government, Aged Care Quality and Safety Commission, Aged Care Quality Standards,
Standard 7(2) – Human Resources, p 4.
3
Australian Government, Aged Care Quality and Safety Commission, Aged Care Quality Standards,
Standard 7(1) – Human Resources, p 4.
4
Australian Government, Aged Care Quality and Safety Commission, Aged Care Quality Standards,
Standard 7(3) – Human Resources, p 4.

LEGISLATIVE COUNCIL
Provisions of the Public Health Amendment (Registered Nurses in Nursing Homes) Bill 2020
4 Discussion paper - February 2021
New South Wales legislation
1.17 In New South Wales, aged care facilities are subject to state legislation, most notably, the Public
Health Act 2010 (NSW). Section 104 currently requires a nursing home to have a registered nurse
on duty at all times:
(1) A person who operates a nursing home must ensure that—
(a) a registered nurse is on duty in the nursing home at all times, and
(b) a registered nurse is appointed as a director of nursing of the nursing home,
and
(c) any vacancy in the position of director of nursing of the nursing home is
filled within 7 days.
1.18 In addition, Section 104(2) provides that the regulations may prescribe the minimum
qualifications to be held by a director of nursing at a nursing home. Clause 95 of the Public Health
Regulation 2012 (NSW) sets out the minimum requirements for a director of nursing at a nursing
home, which include five years post-basic or post-graduate nursing experience and two years of
experience in a management position in a hospital.
1.19 The requirement for a registered nurse to be on duty at all times in a nursing home is a
longstanding one in New South Wales. Prior to the introduction of the Aged Care Act 1997 (Cth),
nursing homes were regulated by the states. Section 39 of the Nursing Homes Act 1988 (NSW)
required a registered nurse to always be on duty in a nursing home. The definition of ‘nursing
home’ at the time was much broader than it is now and included not only aged care facilities
but any premises at which nursing care was provided to residents.
1.20 The Nursing Homes Act was repealed by the Health Legislation Further Amendment Act 2004 (NSW)
due to the Australian Government having introduced the Aged Care Act 1997. The federal
legislation created a situation where nursing homes in New South Wales at the time were
regulated by both the NSW and Australian governments. The Nursing Homes Act was thus viewed
as adding an ‘additional and unnecessary layer of regulation’ to the ‘comprehensive funding and
regulatory regime for aged care facilities’ already provided by the Australian Government.
5
1.21 Nonetheless, some of its provisions were retained. The Health Legislation Further Amendment Act
2004 (NSW) amended the Public Health Act 1991 (NSW) (the predecessor to the current Public
Health Act 2010 (NSW)) so as to continue the staffing requirements of the Nursing Homes Act,
including that a registered nurse always be on duty, as the federal legislation did not include
requirements for minimum nurse staffing.
5
Morris Iemma, Second reading speech: Health Legislation Further Amendment Bill 2004,
22 September 2004.

SELECT COMMITTEE ON THE PROVISIONS OF THE PUBLIC HEALTH AMENDMENT (REGISTERED NURSES IN
NURSING HOMES) BILL 2020
Discussion paper - February 2021 5
The interaction between federal and New South Wales legislation on the requirement
for registered nurses in nursing homes
1.22 Nursing homes have traditionally been viewed as facilities for those with high care needs.
However, use of the term ‘nursing home’ has decreased recently as the terminology used in the
aged care sector has moved away from the clinical language of ‘nursing home’ towards that of
‘residential care’ or ‘in-home care’. This shift in terminology at the federal level, and the ending
of a distinction between high and low care, has had a number of repercussions for the Public
Health Act 2010 (NSW) which uses terms that to some extent are no longer current.
1.23 A ‘nursing home’ is currently defined in Section 5(1) of the Public Health Act 2010 (NSW) as:
a facility at which residential care (within the meaning of the Aged Care Act 1997 of the
Commonwealth) is provided, being—
(a) a facility at which that care is provided in relation to an allocated place (within the
meaning of that Act) that requires a high level of residential care (within the
meaning of that Act), or
(b) a facility that belongs to a class of facilities prescribed by the regulations.
1.24 The definition of ‘nursing home’ thus relies on how ‘residential care’, ‘allocated place’ and ‘high
level of residential care’ are defined in the Aged Care Act 1997 (Cth).
1.25 Care recipients that are approved for residential care under the Aged Care Act 1997 are classified
according to the level of care needed, with reference to the Classification Principles.
1.26 Prior to 1 July 2014, the Aged Care Act 1997 had defined a ‘high level of residential care’ by the
meaning given to it by the Classification Principles. The Classification Principles 1997 (Cth) (in
force until 1 July 2014) had defined a ‘high level of residential care’ as:
residential care given to a care recipient whose classification level:
(a) includes the following domain categories or combinations of domain categories:
(i) a high ADL [Activities of Daily Living] domain category; or
(ii) a high CHC [Complex Health Care] domain category; or
(iii) a domain category of medium or high in at least two of the three domain
categories; or
(iv) a high behaviour domain category and either an ADL domain category
other than nil or a CHC domain category other than nil; or
(b) is high level residential respite care.
LEGISLATIVE COUNCIL
Provisions of the Public Health Amendment (Registered Nurses in Nursing Homes) Bill 2020
6 Discussion paper - February 2021
1.27 However, in 2013 the Aged Care Act 1997 (Cth) was amended to remove the distinction between
low and high levels of residential care.
6
Consequently, the Classification Principles 2014 (Cth) did
not include a definition for ‘high level of residential care’.
1.28 As a result, Section 104 of the Public Health Act 2010 became inoperable. There was no longer a
distinction between nursing homes, which provided for those who required a high level of
residential care, and hostels, which provided a low level of care.
1.29 In response, the NSW Government agreed to maintain mandated minimum nursing
requirements for facilities formerly designated as high care.
7
It achieved this by inserting clause
95A into the Public Health Regulation 2012. Clause 95A clarified that a facility that was a nursing
home for the purposes of the Act immediately before 1 July 2014 was to be prescribed as a
nursing home for the purposes of section 5(1)(b) of the Public Health Act 2010. This was to
ensure that certain facilities would continue to be nursing homes for the purposes of the Public
Health Act 2010 despite amendments to the Aged Care Act 1997 (Cth).
1.30 This has since created a divide in the system, with a distinction between those facilities that
commenced operation after 2014 and those that existed prior. The term ‘nursing home’ in New
South Wales has in many ways come to refer to facilities that were previously classed as
providing a high level of residential care under the Australian Government’s former
classification system.
8
Whilst residential aged care facilities that have been established since 2014
may decide to have a registered nurse on duty 24 hours a day, they are not bound by section 104
of the Public Health Act 2010.
Proposed federal reforms
1.31 Arguments have been made at the federal level for greater clarity concerning the minimum
number of nursing staff required in residential aged care facilities, along with minimum staff to
patient ratios, and necessary qualifications. Counsel Assisting the current Royal Commission
into Aged Care Quality and Safety released their final submissions in October 2020 on the
Commission's proposed recommendations, including recommendations on staffing issues,
discussed further at p 9.
1.32 This issue was also considered by the House of Representatives Standing Committee on Health,
Aged Care and Sport which conducted an inquiry into the quality of care in residential aged care
facilities in Australia, publishing its report in October 2018. The committee noted that ‘the
legislative requirements for staffing of residential aged care facilities are left to the determination
of aged care providers’.
9
However, it felt that a registered nurse should be available at an aged
6
See the Aged Care (Living Longer Living Better) Act 2013 (Cth). For a detailed discussion of the ‘Living
Longer Living Better’ reforms see: Rebecca de Boer and Peter Yeend, Aged Care (Living Longer Living
Better) Bill 2013, Bills Digest No 106, 9 May 2013.
7
Standing Committee on Community Affairs, Australian Senate, Future of Australia’s Aged Care Sector
Workforce (2017), p 58.
8
General Purpose Standing Committee No. 3, NSW Legislative Council, Registered nurses in New South
Wales nursing homes (2015), p 1.
9
Standing Committee on Health, Aged Care and Sport, Australian House of Representatives, Quality
of care in residential aged care facilities in Australia (2018), p 35.
SELECT COMMITTEE ON THE PROVISIONS OF THE PUBLIC HEALTH AMENDMENT (REGISTERED NURSES IN
NURSING HOMES) BILL 2020
Discussion paper - February 2021 7
care facility at all times unless it can be demonstrated that the 'resident mix or size of a facility'
does not warrant compliance with this standard.
10
1.33 The committee made 14 recommendations, including recommendation 4 which sought to
legislate that at least one registered nurse be available at a residential aged care facility at all times:
The Committee recommends that the Australian Government:
legislate to ensure that residential aged care facilities provide for a minimum of
one Registered Nurse to be on site at all times; and
specifically monitor and report on the correlation between standards of care
(including complaints and findings of elder abuse) and staffing mixes to guide
further decisions in relation to staffing requirements.
11
1.34 This recommendation was reiterated by the committee in its advisory report on the Aged Care
Amendment (Staffing Ratio Disclosure) Bill 2018 (Cth) in December 2018.
1.35 The Australian Government responded to the inquiry report in October 2019. The Government
‘noted’ recommendation 4 but emphasised the need for flexibility in staffing levels across the
aged care sector, stating that recommendation 4:
…does not account for the differing levels of support that different care recipients need.
The relationship between staffing and the quality of care provided is complex and there
is considerable diversity in personnel arrangements across accredited homes in
Australia. This is to be expected given the variation across the sector including the
nature of the residents’ needs, facility size and design, the way work is organised and
the extent to which some services are conducted in-house or outsourced. Consequently,
there is no particular staffing mix which meets the circumstances of all care recipients
in residential care facilities.
12
1.36 It also highlighted the flexibility offered by Standard 7, Human Resources of the Aged Care
Quality Standards with its requirement that an organisation have a workforce that is sufficient,
skilled and qualified to provide safe, respectful and quality care and services.
13
1.37 The Senate Community Affairs References Committee commenced an inquiry in 2017 into the
effectiveness of the aged care quality assessment and accreditation framework for protecting
residents from abuse and poor practices, and ensuring proper clinical medical care standards are
maintained and practised.
10
Standing Committee on Health, Aged Care and Sport, Quality of care in residential aged care facilities in
Australia, p 59.
11
Standing Committee on Health, Aged Care and Sport, Quality of care in residential aged care facilities in
Australia, p 52.
12
Australian Government response to the House of Representatives’ Standing Committee on Health,
Aged Care and Sport Report on the Inquiry into the Quality of Care in Residential Aged Care
Facilities in Australia, October 2019, p 6.
13
Australian Government response to the House of Representatives’ Standing Committee on Health,
Aged Care and Sport Report on the Inquiry into the Quality of Care in Residential Aged Care
Facilities in Australia, October 2019, p 7.
LEGISLATIVE COUNCIL
Provisions of the Public Health Amendment (Registered Nurses in Nursing Homes) Bill 2020
8 Discussion paper - February 2021
1.38 In its April 2019 report, the committee agreed on the need for a diverse range of aged care staff,
as well as the requirement for registered nurses to be on duty at all times: 'The committee notes
there is a consensus view that staffing levels should be based on residents' care needs and the
service context, and should be sufficient to provide an appropriate number of care hours per
day from a range of appropriately qualified staff.'
14
The committee thus recommended that:
…the Aged Care Quality and Safety Commission work collaboratively with the
Department of Health, the Australian Commission on Safety and Quality in Health Care
and aged care stakeholders to develop benchmarks for staffing levels and skills mix,
which includes the requirement to roster a Registered Nurse on duty at all times, to
assist residential aged care providers in staff planning and aged care assessors in
regulating safe and appropriate staffing (recommendation 8).
15
1.39 The response of the Australian Government in June 2020 noted this recommendation and the
importance of adequate, skilled staff in residential aged care. The government recognised the
need for further collaborative work in this area and highlighted the establishment of the Aged
Care Workforce Industry Council for this purpose.
16
Royal Commission into Aged Care Quality and Safety
1.40 The Royal Commission into Aged Care Quality and Safety was established on 8 October 2018
and is due to hand down its final report by 26 February 2021.
1.41 The Commission published an interim report on 31 October 2019, which summarised the
evidence to date and identified three areas for urgent action: reducing the waiting list for higher
level home care, the use of chemical restraint, and younger people in residential aged care. On
25 November 2019, the Prime Minister announced actions on these three areas.
17
Key themes
1.42 In the foreword to the interim report, the Commission noted that it had 'heard compelling
evidence that the system designed to care for older Australians is woefully inadequate'.
18
14
Community Affairs References Committee, Australian Senate, Effectiveness of the Aged Care Quality
Assessment and accreditation framework for protecting residents from abuse and poor practices, and ensuring proper
clinical and medical care standards are maintained and practised (2019), p 99.
15
Community Affairs References Committee, Australian Senate, Effectiveness of the Aged Care Quality
Assessment and accreditation framework for protecting residents from abuse and poor practices, and ensuring proper
clinical and medical care standards are maintained and practised (2019), p 99.
16
Australian Government response to the Senate Community Affairs Committee report for the Inquiry
into the effectiveness of the aged care quality assessment and accreditation framework for protecting
residents from abuse and poor practices, and ensuring proper clinical and medical care standards are
maintained and practised, June 2020, p 12.
17
Media release, Hon Scott Morrison MP, Prime Minister, 'Response to Aged Care Royal Commission
interim report', 25 November 2019.
18
Royal Commission into Aged Care Quality and Safety, Interim report (2019), p 12.

SELECT COMMITTEE ON THE PROVISIONS OF THE PUBLIC HEALTH AMENDMENT (REGISTERED NURSES IN
NURSING HOMES) BILL 2020
Discussion paper - February 2021 9
1.43 The key issues and themes that emerged from the evidence include:
how people find out about what aged care is available to them and how to access it
the current regime for establishing and managing the waiting list for home care
the circumstances and challenges involved in providing culturally appropriate, safe and
quality aged care to Aboriginal and Torres Strait Islander people
the use of both physical methods and medications to restrain and pacify people who are
living in residential aged care
problems with recruiting and retaining people to work in aged care
the plight of younger people who have an acute or chronic illness, have suffered a
catastrophic injury or who live with a severe disability, and who are forced into residential
aged care because there is nowhere else for them to go.
19
1.44 The Commission concluded that there are systemic problems with the aged care system in
Australia:
While we have heard a number of examples of specific providers failing to meet existing
standards, the problems in aged care are not just about a series of individual failures.
The flaws of the aged care system as a whole are at the heart of this story. …[T]he
systemic problems with the aged care system include that it:
is designed around transactions, not relationships or care
minimises the voices of people receiving care and their loved ones
is hard to navigate and does not provide the information people need to make
informed choices about their care
relies on a regulatory model that does not provide transparency or an incentive
to improve
has a workforce that is under pressure, under-appreciated and lacks key skills.
20
1.45 In its final submissions, Counsel Assisting also concluded that based on the evidence before the
Commission, 'high quality aged care is not being delivered on a systemic level in our aged care
system and the level of substandard care is unacceptable by any measure'. They also noted that
'at least one in five people receiving residential aged care have experienced substandard care'.
21
Staffing issues
1.46 In its interim report, the Commission noted that it had received 'extensive evidence showing
that aged care workers often experience excessive work demands and time pressure to deliver
care'. The Commission also explained that the 'adequacy and consistency of staffing is an
underlying cause of these pressures and a barrier to the capacity of workers to deliver person-
centred care'.
22
19
Royal Commission into Aged Care Quality and Safety, Interim report (2019), pp 122, 145, 190, 193
and 233.
20
Royal Commission into Aged Care Quality and Safety, Interim report (2019), p 255.
21
Royal Commission into Aged Care Quality and Safety, Counsel Assisting's Final Submissions (2020),
pp 20-21.
22
Royal Commission into Aged Care Quality and Safety, Interim report (2019), pp 230-231.

LEGISLATIVE COUNCIL
Provisions of the Public Health Amendment (Registered Nurses in Nursing Homes) Bill 2020
10 Discussion paper - February 2021
1.47 The question of how to ensure adequate staffing levels in residential care settings emerged as a
contested issue in the evidence before the Commission:
During the second Adelaide Hearing, we received evidence from the Australian Nursing
and Midwifery Federation that the Aged Care Act, the former Accreditation Standards
and the current Aged Care Quality Standards are not explicit enough about what
constitutes adequate staffing arrangements. This means that there is no guarantee that
a nurse will be on duty at all times. A number of witnesses have argued forcefully for
the introduction of mandated staffing levels and skill mix to guarantee a minimum level
of care. Other witnesses have raised concerns about the possible risks of staff ratios,
including that of themselves ratios do not guarantee quality, or suggested alternative
means to ensure adequate staffing levels would be more effective.
23
1.48 The Commission's final report will 'give close consideration to options to ensure staffing levels,
and the mix of staffing, are sufficient to ensure quality and safe care'.
24
1.49 Counsel Assisting’s October 2020 final submissions dealt with workforce issues, and made
recommendations on:
aged care workforce planning
the Aged Care Workforce Council
increase in award wages
improved remuneration for aged care workers
education and training
staffing levels.
25
1.50 With respect to staffing levels, Counsel Assisting submitted that 'a recommendation should be
made that the Australian Government implement a minimum staff time quality and safety
standard for residential aged care', noting that staffing levels is one aspect of reform:
We accept that increasing staffing levels on its own is not a guarantee of high quality
care. But it is an important piece of the puzzle—a necessary but not sufficient reform.
The other pieces include the staffing mix (especially ensuring nurses and allied health
professionals are present in greater numbers), the skills of the workers, how well they
are supervised and managed and how well the organisations they work for are
governed.
26
23
Royal Commission into Aged Care Quality and Safety, Interim report (2019), pp 230-231.
24
Royal Commission into Aged Care Quality and Safety, Interim report (2019), p 231.
25
Royal Commission into Aged Care Quality and Safety, Counsel Assisting's Final Submissions (2020),
pp 190-226.
26
Royal Commission into Aged Care Quality and Safety, Counsel Assisting's Final Submissions (2020),
p 210.

SELECT COMMITTEE ON THE PROVISIONS OF THE PUBLIC HEALTH AMENDMENT (REGISTERED NURSES IN
NURSING HOMES) BILL 2020
Discussion paper - February 2021 11
1.51 Accordingly, Counsel Assisting made the following recommendation in relation to staffing
levels and engagement of registered nurses:
Recommendation 47: Minimum staff time standard for residential care
47.1. The Australian Government should require approved providers of residential aged
care facilities to meet a minimum staff time quality and safety standard. This
requirement should take the form of a quality and safety standard for residential aged
care. The minimum staff time standard should allow approved providers to select the
appropriate skills mix for delivering high quality care in accordance with their model of
care.
47.2. From 1 July 2022, the minimum staff time standard should require approved
providers to engage registered nurses, enrolled nurses, and personal care workers for at
least 215 minutes per resident per day for the average resident, with at least 36 minutes
of that staff time provided by a registered nurse.
47.3. In addition, from 1 July 2022, the minimum staff time standard should require at
least one registered nurse on site per residential aged care facility for the morning and
afternoon shifts (16 hours per day).
47.4. From 1 July 2024, the minimum staff time standard should increase to require
approved providers to engage registered nurses, enrolled nurses, and personal care
workers for the average resident for at least: 215 minutes per resident per day for the
average resident, with at least 44 minutes of that staff time provided by a registered
nurse, or 264 minutes per resident per day for the average resident, with at least 36
minutes of that staff time provided by a registered nurse.
47.5. In addition, from 1 July 2024, the minimum staff time standard should require at
least one registered nurse on site per residential aged care facility at all times.
47.6. The minimum staff time standard should be linked to the casemix adjusted activity
based funding model for residential aged care facilities. This means that approved
providers with a higher than average proportion of high needs residents would be
required to engage additional staff, and vice versa.
47.7. Approved providers should be able to apply to the Australian Aged Care
Commission for an exemption from the quality and safety standard relating to staff
skills mix, but not the standard relating to numbers of staff. Any exemption should be
granted for a limited time, and details of the exemption should be published on My
Aged Care…
The grounds for granting an exemption should include:
a. specific purpose residential aged care facilities, such as specialist homeless facilities,
where the profile of the residents is such that it may be appropriate to substitute a
registered nurse with another qualified health professional
b. residential aged care facilities that are co-located with a health service, such as Multi-
Purpose Services, where registered and enrolled nurses are present at the co-located
health service

LEGISLATIVE COUNCIL
Provisions of the Public Health Amendment (Registered Nurses in Nursing Homes) Bill 2020
12 Discussion paper - February 2021
c. regional, rural and remote residential aged care facilities, where the approved provider
can demonstrate it has been unable to recruit sufficient numbers of staff with the
requisite skills, and
d. innovative residential aged care facilities where an alternative skills mix is being
trialled and it would be appropriate to substitute a registered nurse with another
qualified health professional. There should be a requirement for any such trial to be
comprehensively evaluated and publicly reported.
47.8. The Australian Commission on Safety and Quality in Health and Aged Care should
review and update this standard as appropriate. At a minimum, this should occur in line
with significant revisions of the casemix classification for residential aged care facilities,
or at least every five years.
27
2015 inquiry into registered nurses in nursing homes
1.52 In 2015, General Purpose Standing Committee No. 3 (now referred to as Portfolio Committee
No. 3 – Education) held an inquiry into registered nurses in New South Wales nursing homes.
The committee tabled its report with 17 recommendations on 27 October 2015. The
NSW Government provided its response to the recommendations on 29 April 2016.
1.53 The committee self-referred the inquiry to look into the potential changes at the time to the
federal legislation regarding staffing requirements in nursing homes. The committee considered
the reasons for and concerns about the need for registered nurses in nursing homes at all times;
the adequacy of the federal aged care framework; options for legislative requirements; and
alternative options in the absence of legislation.
1.54 The committee recommended that changes be made to the Public Health Act 2010 (NSW) to
retain the requirement for registered nurses to be on duty in nursing homes at all times:
Recommendation 7:
That the NSW Government:
retain the requirement in section 104(1)(a) of the Public Health Act 2010 for
registered nurses to be on duty in nursing homes at all times, and
amend the definition of ‘nursing home’ under the Act to read:
nursing home means a facility at which residential care (within the meaning of the Aged
Care Act 1997 of the Commonwealth) is provided, being:
(a) a facility at which that care is provided in relation to an allocated place (within the
meaning of that Act) to a care recipient whose classification level:
i. includes the following domain categories or combinations of domain
categories:
1. a high Activities of Daily Living (ADL) domain category; or
2. a high Complex Health Care (CHC) domain category; or
27
Royal Commission into Aged Care Quality and Safety, Counsel Assisting's Final Submissions (2020),
pp 211-212.

SELECT COMMITTEE ON THE PROVISIONS OF THE PUBLIC HEALTH AMENDMENT (REGISTERED NURSES IN
NURSING HOMES) BILL 2020
Discussion paper - February 2021 13
3. a domain category of medium or high in at least two of the three
domain categories; or
4. a high behaviour domain category and either an ADL domain
category other than nil or a CHC domain category other than nil;
or
ii. is a high level resident respite care.
(b) a facility that belongs to a class of facilities prescribed by the regulations.
Recommendation 8:
That the NSW Government allow nursing homes to apply for an exemption from
section 104(1)(a) of the Public Health Act 2010 on a case-by-case basis, and that
exemptions only be granted where the facility can demonstrate that it can still provide
a high level of quality care.
28
1.55 The committee also recognised the importance of mandating safe staffing levels for the range
of skills in the aged care workforce, and recommended:
Recommendation 4:
That the NSW Government, through the Council of Australian Governments, urge the
Commonwealth Government to establish minimum staffing ratios in aged care
facilities.
29
1.56 In its government response, the NSW Government noted that it supported the availability of
registered nurses and recognised the concerns raised before the committee. However, the
government also argued that the retention and expansion of the New South Wales legislation
would create a regulatory duplication without addressing broader issues:
The Government supports availability of registered nurses where appropriate for the
level of care required by residents. The Government also recognises the wide range of
concerns raised in evidence before the Committee. At the same time however, aged care
facilities are regulated under a national system, operating under Commonwealth
legislation. Retention and expansion of the NSW legislation will duplicate regulatory
process without addressing these broader issues. It is also important to highlight that
these recommendations would extend the 24x7 requirement to facilities not previously
caught by the requirement. NSW will therefore pursue concerns about the current
regulatory regime through the COAG Health Council.
30
1.57 A full list of recommendations and the government response is available at Appendix 1.
1.58 On 12 May 2016, the Hon Robert Brown MLC introduced the Public Health Amendment (Registered
Nurses in Nursing Homes) Bill 2016 in the NSW Legislative Council. The intention of the Bill was
28
General Purpose Standing Committee No. 3, NSW Legislative Council, Registered nurses in New South
Wales nursing homes (2015), pp 78-79.
29
General Purpose Standing Committee No. 3, NSW Legislative Council, Registered nurses in New South
Wales nursing homes (2015), p 64.
30
NSW Government response to the recommendation made by the Legislative Council inquiry into
registered nurses in New South Wales nursing homes, April 2016, pp 2-3.

LEGISLATIVE COUNCIL
Provisions of the Public Health Amendment (Registered Nurses in Nursing Homes) Bill 2020
14 Discussion paper - February 2021
‘to amend the Public Health Act 2010 to bring the definition of a nursing home into line with
relevant Commonwealth legislation so as to ensure that the requirement for a registered nurse
to be on duty at all times at a nursing home is continued’.
31
Whilst it passed in the Legislative
Council, the Bill did not pass the Legislative Assembly.
31
Public Health Amendment (Registered Nurses in Nursing Homes) Bill 2016.
SELECT COMMITTEE ON THE PROVISIONS OF THE PUBLIC HEALTH AMENDMENT (REGISTERED NURSES IN
NURSING HOMES) BILL 2020
Discussion paper - February 2021 15
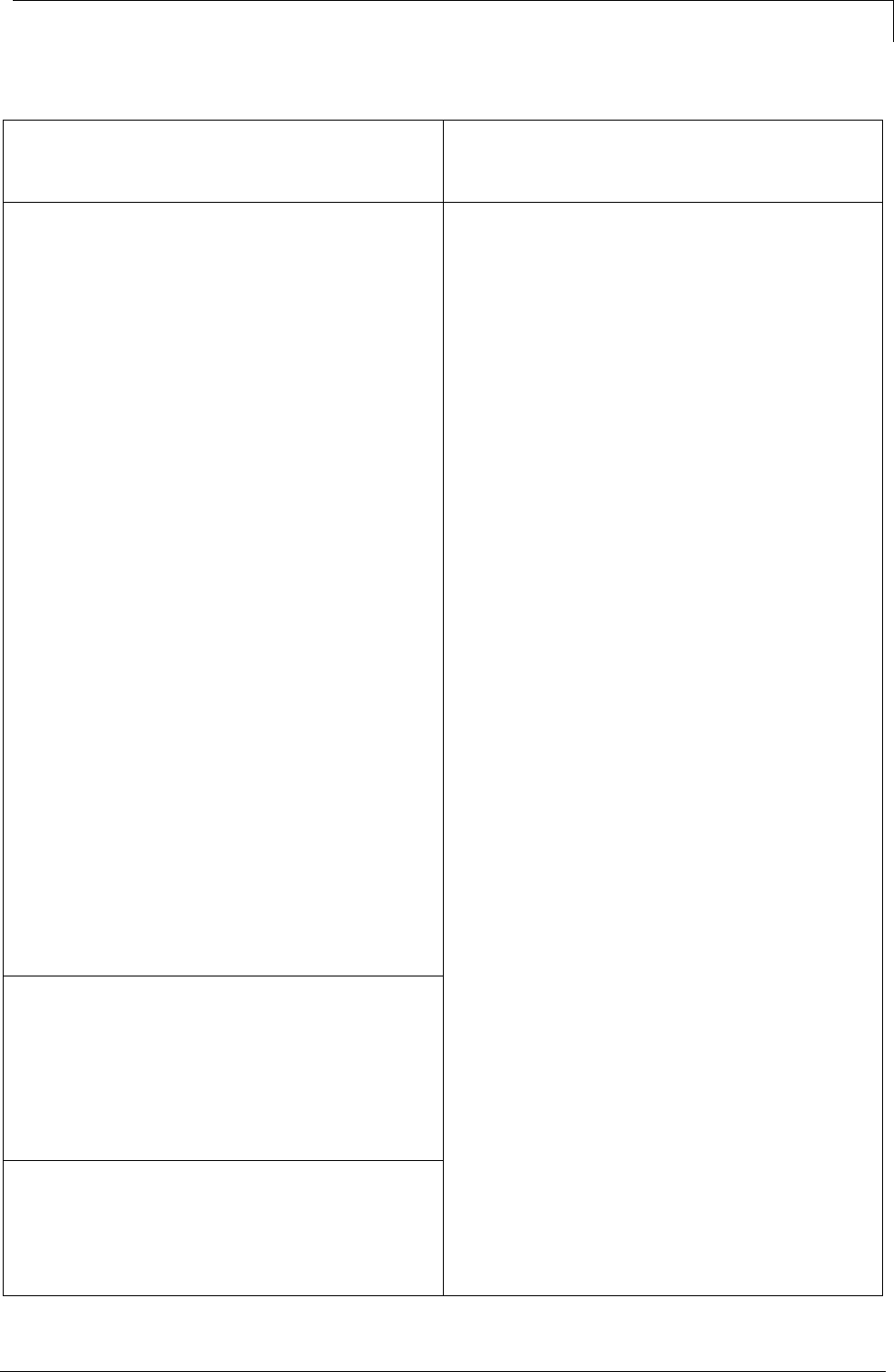
Appendix 1 2015 inquiry into registered nurses in
nursing homes recommendations and
government response
Recommendation
Government response
Recommendation 1:
That the NSW Government:
establish a consistent and compatible collection
and analysis of data regarding the transfer of
residents from aged care facilities to emergency
departments, including reasons for admissions,
to determine if this represents a cost shifting, and
that this information be provided in NSW
Health annual reports to identify if further action
is required.
Recommendation 1 arises from the Committee's
concern that there is a lack of readily available
information about residents transferring from
aged care facilities to public hospitals. Data is
collected on a local level, as are initiatives
developed to prevent unnecessary transportation
of residents from aged care facilities to hospitals:
for example the GRACE program at Hornsby
and the Geriatric Flying Squad operating out of
Sutherland Hospital. The best way to address
these issues is for local health districts to
continue to work in their local communities with
local aged care providers, rather than additional
state wide data collections. This recommendation
is therefore not supported.
Recommendation 2
That the NSW Government review the
requirements for Advance Care Directives to be
recognised when residents are transferred from
aged care facilities to hospitals, and determine
whether a legislative framework is required.
The NSW Government is committed ensuring
advanced care planning is an integral element of
health care planning for patients and in the
community, including in aged care facilities. To
this end, in 2013 the Advanced Planning for Quality
of Care at End of Life: Action Plan 2013-2018
was released. The Action Plan was the result of
extensive work on advanced care planning and
end of life care, including looking at the need for
legislation. As noted in the Action Plan,
Advance Care Directives are already lawful in
NSW under a series of landmark cases in the
Supreme Court, and as such there is a legislation
framework is not proposed. The Action Plan
is also designed to address the situation of
residents of aged care facilities, promoting
routine use of advance care planning for
residents. The Plan provides for progressing
changes to routine admission and discharge
procedures so that prior Advance Care Plans are
recognised, used and transferred between acute
community and aged care settings.
LEGISLATIVE COUNCIL
Provisions of the Public Health Amendment (Registered Nurses in Nursing Homes) Bill 2020
16 Discussion paper - February 2021
Recommendation 3
That the NSW Government, through the
Council of Australian Governments, urge the
Commonwealth Government to ensure that its
new single quality aged care framework includes:
genuinely unannounced visits that occur at any
time of the day on any day of the week,
assessment of all 44 expected outcomes under
the Accreditation Standards during each
unannounced visit,
greater emphasis on resident experience, and
a requirement to communicate non-compliance
with residents and their advocates.
The Australian Aged Care Quality Agency
Accreditation Standards and other aged care
standards are currently being reviewed with a
view to consolidating them into a single set of
standards. This is occurring as part of an
initiative under the 2015 Federal Budget. The
NSW Minister for Health will include these
recommendations in the Paper to be prepared
for COAG Health Council, as set out in
response to Recommendations 7, 8 and 9.
Recommendation 4
That the NSW Government, through the
Council of Australian Governments, urge the
Commonwealth Government to establish
minimum staffing ratios in aged care facilities.
Whether minimum staffing levels would be
appropriate in an aged care setting is primarily a
matter for the relevant Commonwealth agency,
rather than COAG. The NSW Minister for
Health will refer the Parliamentary Committee
Report, including this Recommendation to the
federal Minister for Health and Minister for
Aged Care for consideration.
Recommendation 5
That the NSW Government develop a Working
with Older People and/or Vulnerable Adults
Check, modelled on the Working with Children
Check.
The NSW Government supports robust
mechanisms and checks to protect vulnerable
groups in the community, which can include
residents of aged care facilities as well as
children. The Government also notes however
that "working with children check" processes are
generally state based, and that the
Commonwealth, as part of its regulatory regime
for aged care facilities, already has a national
system for criminal record checking of aged care
workers. The Government will therefore include
this Recommendation in the issues to be raised
with the COAG Health Council.
Recommendation 6
That the NSW Government, through the
Council of Australian Governments, urge the
Commonwealth Government to establish a
licensing body for aged care workers.
The Government does not support further
extending occupational licensing to include
assistants in nursing or other aged care workers.
In relation to the issue of standards for non-
registered health workers, in April 2015 the
COAG Health Council released the "National
Code of Conduct for Health Care Workers". The Code
establishes a series of standards non-registered
health workers must comply with, and is based
on the current NSW Code for Non-Registered
Health
SELECT COMMITTEE ON THE PROVISIONS OF THE PUBLIC HEALTH AMENDMENT (REGISTERED NURSES IN
NURSING HOMES) BILL 2020
Discussion paper - February 2021 17
Practitioners. National adoption of the Code will
strengthen governance in health related fields
without further formal regulation.
Recommendation 7
That the NSW Government:
retain the requirement in section 104(1)(a) of
the Public Health Act 2010 for registered nurses
to be on duty in nursing homes at all times, and
amend the definition of ‘nursing home’ under
the Act to read:
nursing home means a facility at which
residential care (within the meaning of the Aged
Care Act 1997 of the Commonwealth) is
provided, being:
(a) a facility at which that care is provided in
relation to an allocated place (within the meaning
of that Act) to a care recipient whose
classification level:
(i) includes the following domain categories or
combinations of domain categories:
(1) a high Activities of Daily Living (ADL)
domain category; or
(2) a high Complex Health Care (CHC) domain
category; or
(3) a domain category of medium or high in at
least two of the three domain categories; or
(4) a high behaviour domain category and either
an ADL domain category other than nil or a
CHC domain category other than nil; or
(ii) is a high level resident respite care.
(b) a facility that belongs to a class of facilities
prescribed by the regulations.
The Government supports availability of
registered nurses where appropriate for the level
of care required by residents. The Government
also recognises the wide range of concerns raised
in evidence before the Committee. At the same
time however, aged care facilities are regulated
under a national system, operating under
Commonwealth legislation. Retention and
expansion of the NSW legislation will duplicate
regulatory process without addressing these
broader issues.
It is also important to highlight that these
recommendations would extend the 24x7
requirement to facilities not previously caught by
the requirement.
NSW will therefore pursue concerns about the
current regulatory regime through the COAG
Health Council.
Recommendation 8
That the NSW Government allow nursing
homes to apply for an exemption from section
104(1)(a) of the Public Health Act 2010 on a
case-by-case basis, and that exemptions only be
granted where the facility can demonstrate that it
can still provide a high level of quality care.
Recommendation 9
That the NSW Government establish a system to
monitor, regulate and enforce section 104(1)(a)
of the Public Health Act 2010.
LEGISLATIVE COUNCIL
Provisions of the Public Health Amendment (Registered Nurses in Nursing Homes) Bill 2020
18 Discussion paper - February 2021
Recommendation 10
That the NSW Government, through the
Council of Australian Governments, urge the
Commonwealth Government to require aged
care facilities to make information about their
staffing skill sets publicly available, including for
it to be published on the ‘My Aged Care’ website.
The Committee's rationale for supporting this
recommendation went to the need for increased
transparency to ensure residents and their
families can make better, and more informed
decisions about aged care options. This
recommendation will be included in the issues to
be raised with the COAG Health Council.
Recommendation 11
That the NSW Government, through the
Council of Australian Governments, urge the
Commonwealth Government to require aged
care facilities to make information about their
staffing skill sets publicly available, including for
it to be published on the ‘My Aged Care’ website.
The Government accepts that the evidence
before the Committee indicates there are
grounds for more work to be undertaken at both
the State and Federal level to ensure residents
have better information on the complaints
processes available to them.
NSW residents of aged care facilities should have
ready access to complaints processes in
NSW relating to health care - such as for
example, the Health Care Complaints
Commission. To this end, NSW will develop
information packages on the options available
under NSW laws for dissemination through aged
care facilities. The information will be most
effective if it covers all options available to
residents, including processes available through
the Commonwealth. NSW will work with
relevant Commonwealth agencies to develop the
information, and establish processes to ensure its
dissemination to residents, carers and advocates.
Recommendation 12
That the NSW Government establish a clear
process for the lodgement and resolution of
complaints about section 104(1)(a) of the Public
Health Act 2010 as part of the new system at
recommendation 9, and that information about
the complaints process be widely publicised
throughout aged care facilities in New South
Wales.
Recommendation 13
That the NSW Government report on existing
programs and incentives and investigate
additional programs and incentives to support
registered nurses to train and work in regional,
rural and remote areas.
NSW Health has a range of programs and
incentives in place to support nurses working
and training in regional, rural and remote
locations, primarily managed through the local
health districts. It is important to note that in
2016 over a quarter of new graduates employed
by NSW Health will be working in rural and
regional NSW. NSW Health will continue to
monitor supply and develop and evaluate
programs on a needs basis. The current
initiatives are also, necessarily confined to the
NSW public health system workforce, while aged
care services are primarily provided by the
private sector. Recommendation 14 and 15 go
directly the Commonwealth's role and functions
in respect of aged care. As already indicated it is
proposed that the NSW Minister for Health refer
the report and these recommendations to the
Federal Minister for Heath and Aged Care.
Recommendation 14
That the NSW Government, through the
Council of Australian Governments, seek
Commonwealth support to provide funding
assistance for the training and engagement of
registered nurses, particularly at rural and
regional universities, and graduate placement
opportunities in rural, regional and remote areas.
Recommendation 15
That the NSW Government, through the
Council of Australian Governments, urge the
Commonwealth Government to take active
measures to address the wage disparity between
SELECT COMMITTEE ON THE PROVISIONS OF THE PUBLIC HEALTH AMENDMENT (REGISTERED NURSES IN
NURSING HOMES) BILL 2020
Discussion paper - February 2021 19
registered nurses in aged care facilities and
registered nurses in the public health care system.
Recommendation 16
That the NSW Government consider rolling out
the Telehealth model of care provided by the
Hunter-New England Medical Local across New
South Wales.
The Government supports rollout of Telehealth
models of care in appropriate settings, including
in aged care facilities. Reflecting this, a range of
initiatives are already underway across the
public health system, helping to embed telehealth
into clinical practice in a number of settings.
Local health districts are actively engaging with
their key external stakeholders and service
providers to establish arrangements for patients
to access care through telehealth. Partnerships
are being cultivated with local GPs, Primary
Health Networks (PHNs) and Residential Aged
Care Facilities (RACFs) amongst others. For
example Murrumbidgee LHD is working closely
with Primary Health Networks and NSW
Ambulance to develop telehealth enabled inreach
and outreach models of care. Outreach to Aged
Care Facilities is also a priority, as part of
hospital avoidance strategies. Mid North Coast,
North Sydney and Northern NSW LHDs are
also developing Telehealth models of care with
key Aged Care Facilities within their boundaries
to reduce avoidable hospital admissions.
Recommendation 17
That the NSW Government:
review alternative models of housing for older
persons other than aged care facilities, including
cooperatives and communal living that provide
an on-site caretaker, and
investigate models in other jurisdictions,
including the Netherlands and Scandinavia, that
could be trialled in New South Wales.
The Commonwealth aged care system already
includes Home Care Packages designed to
provide services to support older people to
continue to live in their own homes, as well as
residential aged care services. Both Home Care
Packages and residential aged care services
are intended to provide services from low care to
high care. The Commonwealth also provides
the Commonwealth Home Support Program
(CHSP) offering a range of low level support
services with the intention of supporting older
people to live independently in the community
for longer. While the need to consider new and
alternative models is supported, this should
occur through the Commonwealth.
Recommendation 17 is therefore noted and will
be forwarded the Commonwealth Minister for
consideration.

