
2024
BENEFITS
GUIDE

TABLE OF CONTENTS
2
VENDOR DIRECTORY ............................................................................................................................... 4
ELIGIBILITY, ENROLLMENT, and QUALIFYING LIFE EVENTS ................................................................. 5
2024 BENEFIT RATES ............................................................................................................................... 6
MEDICAL PLAN HIGHLIGHTS .................................................................................................................. 7
MEDICAL PLAN OVERVIEW ...................................................................................................................... 8
PRESCRIPTION PLAN HIGHLIGHTS ........................................................................................................ 9
WELLNESS AND HEALTH MANAGEMENT PROGRAMS ......................................................................... 13
DENTAL INSURANCE ................................................................................................................................ 15
VISION INSURANCE ................................................................................................................................. 17
SPENDING ACCOUNTS ............................................................................................................................ 18
LIFE INSURANCE ...................................................................................................................................... 19
DISABILITY INSURANCE .......................................................................................................................... 20
LONG-TERM CARE INSURANCE ............................................................................................................. 22
EMPLOYEE ASSISTANCE PROGRAM (EAP) ............................................................................................ 23
FACE IT TOGETHER .................................................................................................................................. 24
RETIREMENT ............................................................................................................................................. 25
VOLUNTARY RETIREMENT SAVINGS PLANS .......................................................................................... 26
VACATION BUY, PAID TIME OFF, TUITION ASSISTANCE ........................................................................ 27
EMPLOYEE PERKS ................................................................................................................................... 28
FREQUENTLY ASKED QUESTIONS .......................................................................................................... 30
HELPFUL REMINDERS ............................................................................................................................. 31
HEALTHCARE REFORM ........................................................................................................................... 32
NOTICES ................................................................................................................................................... 33
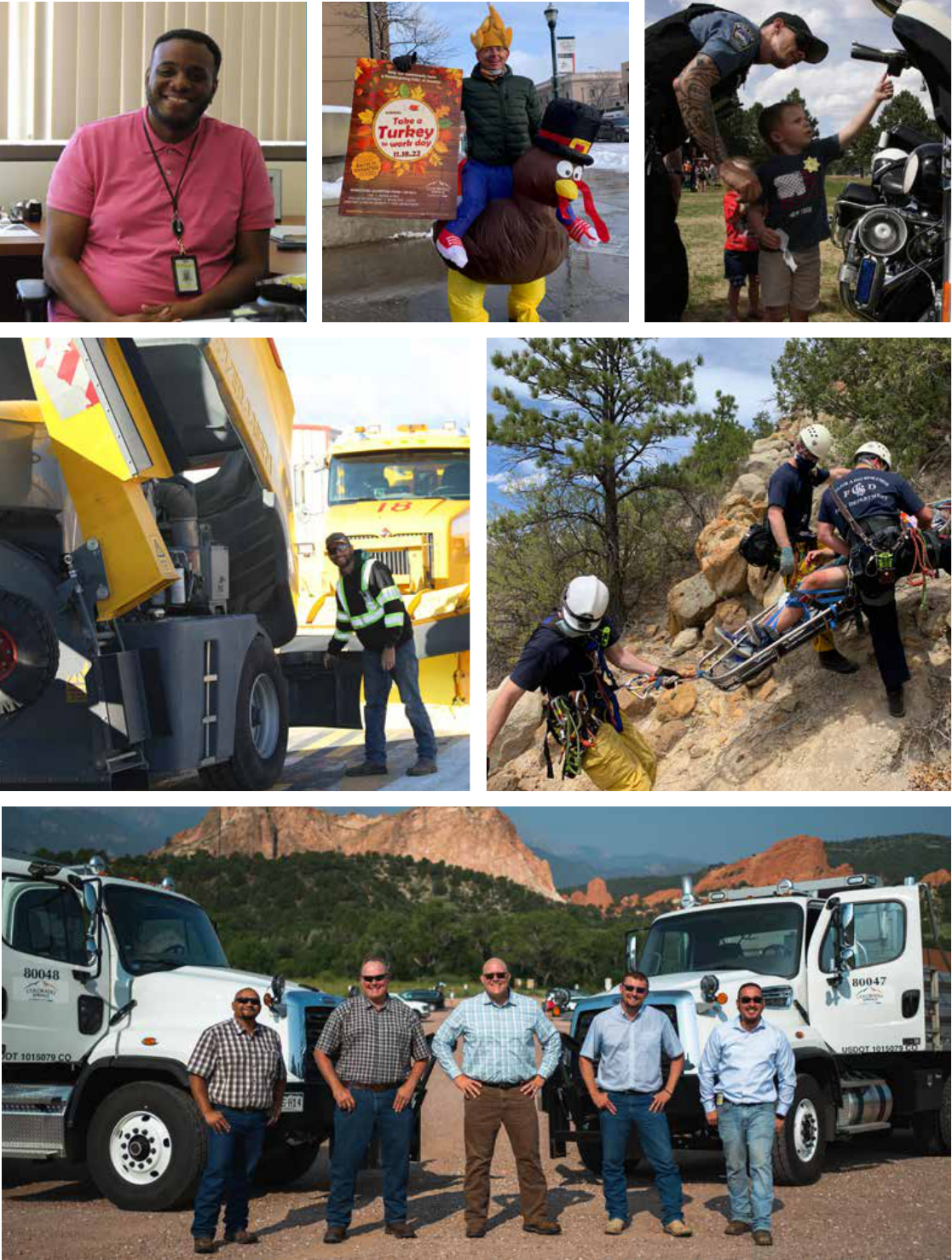
Mayor Yemi Mobolade
Jamie Fabos,
Chief of Staff
Myra Romero,
Acting Chief Human
Resources and Risk Officer
Hello City Team:
Tha
nk you for your passion and hard work providing the
essential services that residents rely on every day. We’ve
seen a lot of great accomplishments in 2023, and it is
because of the dedication and passion each of you bring
to serving our community.
Attracting and retaining a highly skilled and talented
workforce is critical to the success of our organization
and to creating positive impacts for citizens. That is why
we are pleased to offer a competitive Total Rewards
package for City employees. We are committed to
providing a comprehensive benefits package that
supports your physical and mental wellbeing, as well as
your financial security. We are excited to share changes
for 2024 that provide enhanced coverage with robust and
high-quality providers.
We are proud to invest in our employees with a 2024 Benefits
Program that contributes to your overall well-being.
Onward and Upward,
Mayor Yemi Mobolade
Chief of Staff, Jamie Fabos
Acting Chief Human Resources and Risk Officer, Myra Romero
Please visit the Benefits and Wellness
webpage for detailed information.
This benefits guide is not intended to include all benefit details. It is an outline of available coverage and is not intended to be a legal contract.
If a discrepancy exists between this document and the Plan Documents, the Plan Documents govern.
The benefits guide applies to all City of Colorado Springs civilian and sworn employees, unless otherwise noted.
NOTE: ANNUAL APPROPRIATIONS REQUIREMENT: Other than those benefits specifically required by federal or state law, the programs
within the benefits plan provided by the City for employees are subject to annual review and budget appropriations by City Council. The City and
employee contributions toward the cost of the benefits plan, as well as the benefit plan designs, may be changed, or discontinued altogether at
the Mayor’s discretion. Specific details are available at coloradosprings.gov in the Policies and Procedures Manuals (PPM).
3
VENDOR DIRECTORY ............................................................................................................................... 4
ELIGIBILITY, ENROLLMENT, and QUALIFYING LIFE EVENTS ................................................................. 5
2024 BENEFIT RATES ............................................................................................................................... 6
MEDICAL PLAN HIGHLIGHTS .................................................................................................................. 7
MEDICAL PLAN OVERVIEW ...................................................................................................................... 8
PRESCRIPTION PLAN HIGHLIGHTS ........................................................................................................ 9
WELLNESS AND HEALTH MANAGEMENT PROGRAMS ......................................................................... 13
DENTAL INSURANCE ................................................................................................................................ 15
VISION INSURANCE ................................................................................................................................. 17
SPENDING ACCOUNTS ............................................................................................................................ 18
LIFE INSURANCE ...................................................................................................................................... 19
DISABILITY INSURANCE .......................................................................................................................... 20
LONG-TERM CARE INSURANCE ............................................................................................................. 22
EMPLOYEE ASSISTANCE PROGRAM (EAP) ............................................................................................ 23
FACE IT TOGETHER .................................................................................................................................. 24
RETIREMENT ............................................................................................................................................. 25
VOLUNTARY RETIREMENT SAVINGS PLANS .......................................................................................... 26
VACATION BUY, PAID TIME OFF, TUITION ASSISTANCE ........................................................................ 27
EMPLOYEE PERKS ................................................................................................................................... 28
FREQUENTLY ASKED QUESTIONS .......................................................................................................... 30
HELPFUL REMINDERS ............................................................................................................................. 31
HEALTHCARE REFORM ........................................................................................................................... 32
NOTICES ................................................................................................................................................... 33
Medical Benefits
Medical Insurance
Group Number: JCQ003
Premier Plan
Advantage Plan
Anthem Blue
Priority PPO Network
CEMC:
Monday - Friday
7:30 AM - 4:30 PM
Wednesday
9:00 AM - 6:00 PM
Pharmacy:
Monday – Friday
8:30 AM – 5:30 PM
Teladoc
ZERO Health
Hinge Health
Dental Insurance
Vision Insurance
Reach Your Peak
Wellness
UCCS
Life Insurance
Disability Insurance
Long Term Care (LTC)
Spending Accounts
FSA
HRA
Retirement
Profile Employee
Assistance Program
Face It Together
HR Solutions Center
VENDOR DIRECTORY
City Care
AmeriBen Concierge Consumer Support
AmeriBen Medical Management
Case Management, and Prior Authorization
Anthem - Provider Network Access
Castlight
Provider Search, Cost and Quality
Comparisons, and Health Related Resources
City Employee Medical Clinic (CEMC)
Medical Services located at
4863 North Nevada Avenue, 2nd Floor,
Colorado Springs, CO 80918
City Employee Pharmacy
Pharmacy located in the Garden Level of the City
Administration Building (CAB), Suite L04
MaxorPlus
Pharmacy Benefit Manager, In-Network Retail
Pharmacies, and Pharmacy ID Cards
Medical & Behavioral Health Services
Delta Dental
Hi-Option Plan #1512
Standard Option Plan #1844
Vision Service Plan (VSP)
Plan #12061804
HealthYou
UCCS
The Hartford - Policy #804057
The Hartford - Policy #804057
UNUM Life Insurance Company of America
Policy #220508 (Elections prior to 2008)
Policy #127251 (Elections 2008 and forward)
Navia Benefit Solutions
FSA for Health Care & Dependent Care
HRA for Advantage Plan Participants
Public Employees Retirement Association
Fire & Police Protective Association (FPPA)
MissionSquare Retirement, LLC
Gloria Michalko
Profile EAP: Centura Health
Company Code: COSPGS
Addiction & Recovery Coaching
HR/Benefit questions and enrollment support
(866) 955-1482
myameriben.com
(855) 778-9052
myameriben.com
anthem.com
(800) 684-0624
mycastlighthealth.com
(719) 385-5841
Fax: (719) 385-5842
(719) 385-2261
Auto-Refill Line: (800) 573-6214
cityemployeepharmacy.com
(800) 687-0707 • maxor.com
(800) 835-2362 • teladoc.com
(815) 816-0001 • [email protected]
(855) 902-2777 • [email protected]
(800) 610-0201 • deltadentalco.com
(800) 877-7195 • vsp.com
(719) 314-3535
cosreachyourpeak.com
(888) 563-1124 • thehartford.com
(888) 301-5615
Abilityadvantage.thehartford.com
(800) 227-4165 • unum.com
(866) 897-1996
Fax: (866) 831-6222
naviabenefits.com
105@NaviaBenefits.com
(800) 759-7372 • copera.org
(800) 332-3772 • fppaco.org
(202) 759-7178
(800) 645-6571 • profileeap.org
(855) 539-9375 • wefaceittogether.org
(719) 385-5125
4

WHAT IS A QUALIFYING LIFE EVENT (QLE)?
Note: Newborns are not automatically added to your plan. Do not wait
until you receive the birth certificate and/or Social Security number to
contact the HR Solution Center.
QUALIFYING LIFE EVENTS:
You can review your benefits at the time of a qualifying
life event. If you have a qualified life event change in
status during the plan year, you must:
Contact the HR Solutions Center within 30 days of the
event in writing.
Complete and submit a Benefits Change Form.
Provide documentation of the qualifying event.
Note: Benefit changes occur prospectively on the first of the month after
the HR Solutions Center receives all necessary paperwork.
ELIGIBILITY
All regular, probationary, and special employees
scheduled to work 20 hours or more each week may
participate in the City of Colorado Springs’ Benefits
Programs unless otherwise noted.
Hourly employees may be eligible for medical benefits
as mandated by the Patient Protection and Affordability
Care Act.
Eligible dependents include:
Your legal spouse, common law spouse or civil union.
Your natural, adopted, or stepchildren (up to age 26).
Eligible children of any age who were disabled before
age 26.
Note: Only eligible dependents can be covered under the plan(s).
must provide proof of dependent eligibility
ENROLL & MAKE CHANGES
Carefully review the benefits available to you and choose
the best package for you and your family and budget.
Your enrollment choices remain in place for the plan year
(January 1, 2024 – December 31, 2024)
You can enroll in or make changes to your benefits:
Within 30 days of your hire date.
During the annual Open Enrollment (OE) period.
Within 30 days of a Qualifying Life Event.
ELIGIBILITY, ENROLLMENT, & QUALIFYING LIFE EVENTS
Birth of a newborn, adoption, or placement
or guardianship of a child. This QLE occurs
on the event date.
Family changes, such as marriage, divorce,
legal separation, change in dependent eligibility,
or death of your spouse or dependent.
Change in employment status by you or your
eligible dependents such as termination or
commencement of employment, unpaid leave
status, or change from full-time to part-time.
Enrollment in a Qualified Health Plan through
the Marketplace; Government Health Plan
such as Tricare, Medicare, or Medicaid; or
other Group Health Coverage.
5
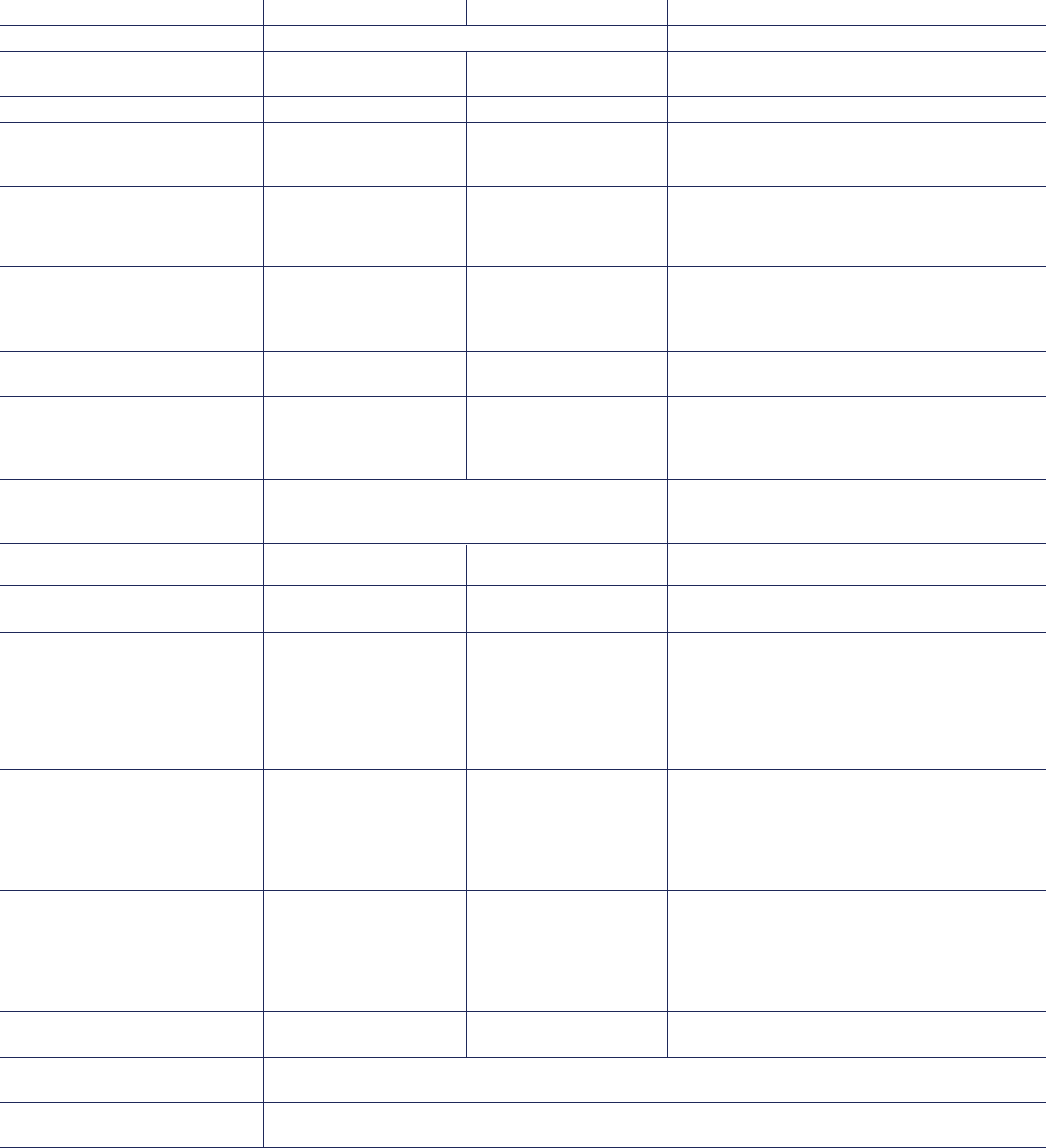
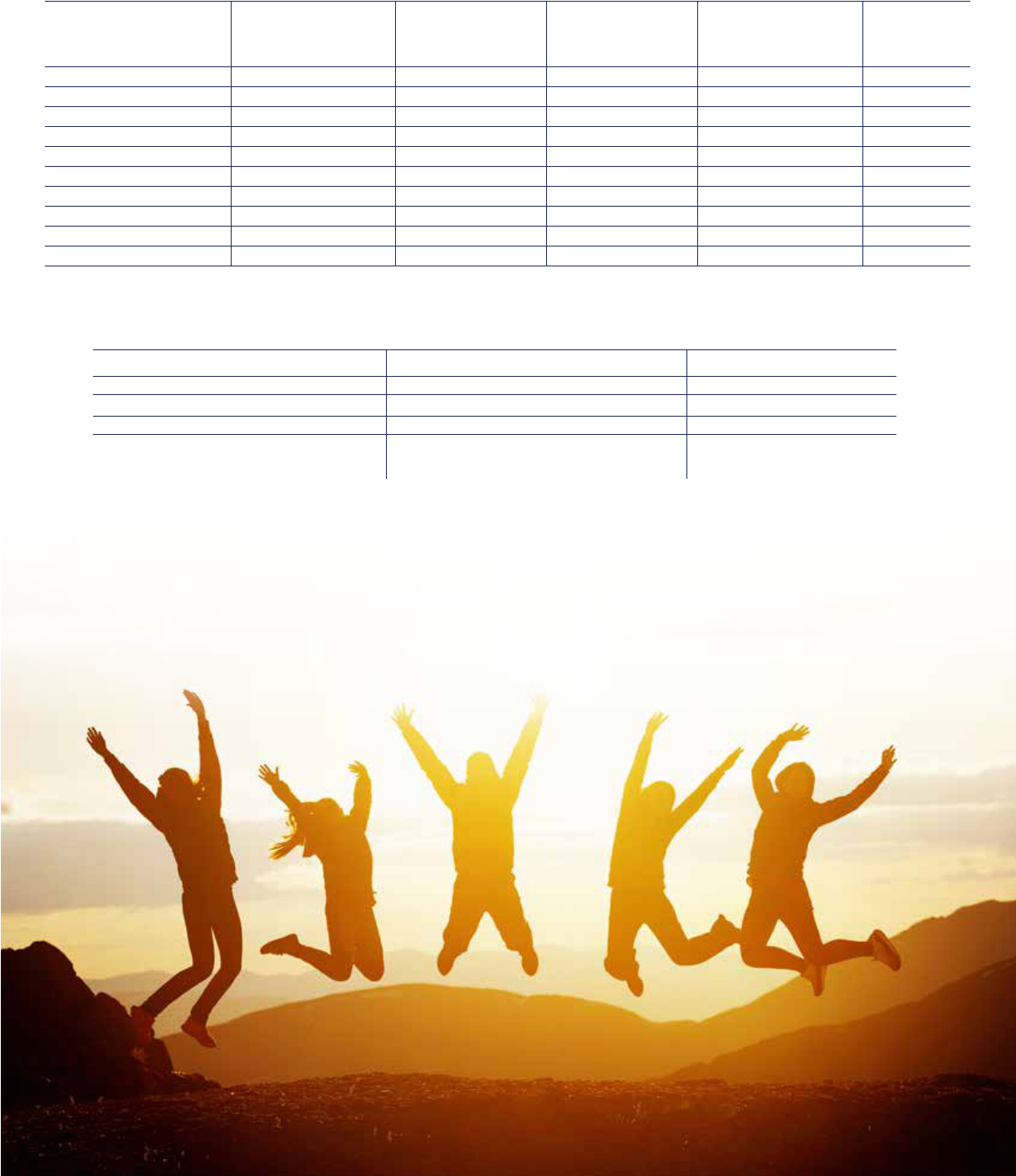
2024 MEDICAL PLAN HIGHLIGHTS BENEFIT RATES
Premier Medical Plan Rates – Monthly
Coverage Level Total Plan Cost Employer Share Employee (EE) Share*
EE Only $947 $699 $248
EE + Spouse $1,879 $1,270 $609
EE + Child $1,767 $1,222 $545
EE + Family $2,674 $1,850 $824
Advantage Medical Plan Rates – Monthly
Coverage Level Total Plan Cost Employer Share Employee Share* Annual Employee
HRA Funding
EE Only $738 $699 $39 $500
EE + Spouse $1,491 $1,270 $221 $750
EE + Child $1,419 $1,222 $197 $750
EE + Family $2,152 $1,850 $302 $750
*Note: There is an additional $50 per month surcharge for employees on the Premier and Advantage medical plan who are tobacco users.
Delta Hi-Option PPO Dental Plan Rates – Monthly
Coverage Level Total Plan Cost Employer Share Employee Share
EE Only $49 $35 $14
EE + Spouse $111 $45 $66
EE + Child $90 $45 $45
EE + Family $136 $45 $91
Delta Standard Option PPO Dental Plan Rates – Monthly
Coverage Level Total Plan Cost Employer Share Employee Share
EE Only $35 $35 $0
EE + Spouse $83 $45 $38
EE + Child $67 $45 $22
EE + Family $101 $45 $56
Vision Service Plan Rates – Monthly
Coverage Level Total Plan Cost Employer Share Employee Share
EE Only $7.72 $0 $7.72
EE + Spouse $15.46 $0 $15.46
EE + Child $16.55 $0 $16.55
EE + Family $26.44 $0 $26.44
To calculate your rates per pay period, divide the Employee Share amount by 2. There are 24 premium payments during
the year. Civil Union cost may have Pre-Tax and Post Tax implications; contact the HR Solutions Center for more details.
6

IMPORTANT PLAN TERMS
Premiums
The amount you and your employer pay each month to be
enrolled in medical, dental, and vision insurance.
Deductible
The amount you must pay each year for certain covered
health services before the insurance plan will begin to pay.
Coinsurance
Your share of the cost of covered health care services,
after you meet your deductible.
Co-pay
A fixed amount you pay for certain covered health services.
Typically, your co-pay is due at the time of service.
Out-of-Pocket Maximum
The most you will pay for covered health services during
the plan year. Co-pays, deductibles, and coinsurance all
apply toward the out-of-pocket maximum.
Covered Services
Services for which benefits are payable. If you receive
care for services not covered under the plan, the amount
you pay for those services will not apply toward your
deductible or out-of-pocket maximum.
Enhanced Personal Health Care (EPHC)
Primary Care Providers. You will pay a lower co-pay, and
have your deductible waived when you see these providers.
Tier I Specialists
Using these specialists will reduce your out-of-pocket
expenses and you will pay a lower co-pay and have your
deductible waived.
Site of Service Program
Save money on advanced imaging and outpatient surgery by
participating in a free-standing, independent imaging provider
or ambulatory surgery center from the Anthem Network.
MEDICAL PLANS
The City offers two self-funded medical plans: the Premier
Plan and the Advantage Plan. The Advantage Plan is paired
with a Health Reimbursement Account (HRA) funded by the
City. Both plans feature an in-network and out-of-network
benefit. Anthem Blue Cross Blue Shield is our preferred
provider organization (PPO) network for both plans and
AmeriBen is the medical claims administrator. Medical
premiums may be paid using pre-tax dollars and both plans
include access to a robust, affordable care delivery model.
Employees and family members on the City’s Medical
Plan are eligible for these services:
• City Employee Medical Clinic
• City Employee Pharmacy
• Alternative Medicine
• Diabetes Ten City Challenge
• CardioRx Program
• Maternal Health Program
• Tobacco Cessation
• Reach Your Peak
(Available only for Employee and Spouse)
7
MEDICAL PLAN HIGHLIGHTS TERMS & MORE
Premier Plan Advantage Plan
Type of service In-Network Benefit Out-of-Network Benefit In-Network Benefit Out-of-Network Benefit
Lifetime Maximum Unlimited Unlimited
Annual Deductible $500 Individual $1,250 Individual $1,500 Individual $4,500 Individual
$1,250 Family $2,500 Family $3,000 Family $9,000 Family
Coinsurance (1) You pay 20% You pay 50% You pay 20% You pay 50%
Annual Out-of-Pocket $2,500 Individual $4,050 Individual $3,500 Individual $9,000 Individual
Maximum $7,500 Family $12,150 Family $8,000 Family $18,000 Family
(OPM)/Coinsurance (1)
Primary Care Office Visit (2) EPHC - $25 co-pay, You pay 50% EPHC - $30 co-pay, You pay 50%
deductible waived; after deductible deductible waived; after deductible
All others - $35 after All others - $40 after
deductible deductible
Specialist Office Visit (2) Tier I - $40 co-pay, You pay 50% Tier I - $60 co-pay, You pay 50%
deductible waived; after deductible deductible waived; after deductible
All others - $60 after All others - $70 after
deductible deductible
Mental Health Office Visit (3) $25 co-pay, You pay 50% $30 co-pay, You pay 50%
deductible waived after deductible deductible waived after deductible
Urgent Care $50 co-pay, deductible You pay 50% You pay 20%, You pay 50%
waived; coinsurance for after deductible deductible coinsurance after deductible
diagnostic & surgical for diagnostic & surgical
services services
Emergency Room Visits $250 co-pay, then you pay 20% for diagnostic You pay 20%, deductible waived
and surgical services, deductible waived
If admitted to the hospital, ER co-pay waived
Diagnostic Services You pay 20% You pay 50% You pay 20% You pay 50%
after deductible after deductible after deductible after deductible
Inpatient Mental Health You pay 20% You pay 50% You pay 20% You pay 50%
after deductible after deductible after deductible after deductible
Inpatient Hospital Services Utilize an UCHealth You pay 50% Utilize an UCHealth You pay 50%
Facility - you pay after deductible Facility - you pay after deductible
15% after deductible 15% after deductible
All hospital services All hospital services
and all other facilities and all other facilities
You pay 20% after You pay 20% after
deductible deductible
Advanced Imaging Freestanding Facility You pay 50% Freestanding Facility You pay 50%
(MRI/CT/PET) - you pay 10% after after deductible - you pay 10% after after deductible
deductible; deductible;
All other facilities - All other facilities -
you pay 20% after you pay 20% after
deductible deductible
Outpatient/Ambulatory Freestanding Facility You pay 50% Freestanding Facility You pay 50%
Surgery - you pay 10% after after deductible - you pay 10% after after deductible
deductible; deductible;
All other facilities - All other facilities -
you pay 20% after you pay 20% after
deductible deductible
Preventive Care (3) You pay $0 You pay 50%; You pay $0 You pay 50%;
deductible waived deductible waived
Alternative Medicine Plan Pays 50% of each claim up to an annual family maximum of $1,000, deductible waived.
Nutritionists & Dieticians – maximum of 16 visits per year per member, 50% coinsurance, deductible waived
Fertility Benefits This plan pays up to a $30,000 lifetime benefit and supports you through your unique fertility challenges,
helping you explore your options and undergo treatment processes.
Notes: (1) The OPM and coinsurance are accounted for separately for in-network and out-of-network services.
(2) Co-pay applies to an office visit only. Deductible and coinsurance apply for diagnostic and surgical
services performed in the office setting.
(3) A Mental Health Screening is a covered benefit under Preventive Care.
This table is not intended to include all benefit details. It is an outline of coverage available and is not intended to be a legal contract.
If a discrepancy exists between this document and the official Plan Documents, the Plan Documents govern.
MEDICAL PLAN OVERVIEW
8
PRESCRIPTION PLAN HIGHLIGHTS
Employees and their eligible dependents
enrolled in a City medical plan can fill their
prescriptions at the City Employee
P
harmacy or through one of the MaxorPlus participating
network pharmacies. You will save money if you fill your
prescription at the City Employee Pharmacy.
MaxorPlus also provides services relating to specialty inject
ables, specialty drugs, and certain respiratory therapies
through its subsidiary, Maxor Specialty Pharmacy. This
Specialty Injectable and Specialty Drug Program will benefit
you and the patient and help contain the costs of expensive
medications. Maxor Specialty Pharmacy will be working in
conjunction with the City Employee Pharmacy to fill medications
through this program.
To access high quality care at the lowest cost, visit the City Employee Pharmacy.
Pharmacy Tier Prescription Type Cost
City Employee Pharmacy 1st Tier Generic $6 co-pay (30-day supply)
$15 co-pay (90-day supply)
2nd Tier Preferred Brand $35 co-pay (30-day supply)
$70 co-pay (90-day supply)
3rd Tier Non-Preferred Brand $60 co-pay (30-day supply)
$120 co-pay (90-day supply)
Specialty Pharmacy 4th Tier* Preferred Chronic Injectables 20% coinsurance with a maximum
(MaxorPlus IV Solutions) and other Specialty Drugs co-pay of $100 (30-day supply)
5th Tier* Non-Preferred Chronic Injectables 20% coinsurance with a maximum
and other Specialty Drugs co-pay of $150 (30-day supply)
MaxorPlus Retail 1st Tier Generic $25 co-pay (30-day supply)
Network Pharmacies 2nd Tier Preferred Brand $55 co-pay (30-day supply)
3rd Tier Non-Preferred Brand $75 co-pay (30-day supply)
4th Tier & 5th Tier Preferred/Non-Preferred N/A – Only available through
Chronic Injectables
Co-insurance and co-pays for prescription drugs do not apply to the deductible but do apply to the out-of-pocket maximum.
Maintenance Prescription Fills - For a complete listing of participating pharmacies go to the Preferred Pharmacy
Information at cityemployeepharmacy.com. Plan participants will progressively pay higher co-pays for maintenance
prescriptions that are filled at a MaxorPlus Retail Network Pharmacy versus the City Employee Pharmacy. Additional
information regarding your pharmacy benefits can be found on MaxorPlus.com.
Engagement in health management programs may allow for waived co-pays. Contact the HR Solutions Center or City
Employee Pharmacy to learn more.
Maintenance prescriptions filled at any MaxorPlus Retail Network Pharmacy:
First fill: Member pays the normal co-pay Second fill: Member pays double the co-pay
Third and subsequent fills: Member pays 100% of the retail cost for the maintenance prescription
Select preventive care medications are covered at 100% and may change in accordance with United States Preventive
Services Taskforce guidelines.
*Maxor Specialty Pharmacy Patient Care Advocates will assist members with enrollment in manufacturer copay assistance
programs if available. Please note that not all specialty medications will have co-pay assistance available. Those medications
that do have assistance available are subject to availability and may be discontinued at any time. Any portion known to have
been paid by a secondary payer (i.e., patient assistance, co-pay cards, discounts, or other insurance) will not be considered
as true out-of-pocket costs and will not apply to your plan deductible and out-of-pocket maximums.
This table is not intended to include all benefit details. It is an outline of coverage available and is not intended to be a legal contract. If a discrepancy exists
between this document and the official Plan Documents, the Plan Documents govern.
9

CASTLIGHT
An informed consumer shops for high quality,
affordable health care using Castlight’s
transparency tool, receives their preventive
care benefits, and uses the correct facility or
provider for services. When you are an engaged consumer
of health care, you do make a difference.
Get peace of mind - Clearly see what is covered by your
plan, how much services will cost, and where you have
spent your healthcare dollars.
Find doctors you will love - Search ratings and reviews
from real people and find high-quality (EPHC and Tier 1)
doctors or specialists in your network and near you.
Feel great about your benefits - Discover your health and
well-being resources and see all your perks in one place.
10
MEDICAL PLAN HIGHLIGHTS
TELADOC
Teladoc gives you access 24 hours a day, 7 days a week
to a U.S. board certified doctor through the convenience
of phone, video, or mobile app visits. Teladoc is accessible
anywhere in the U.S.
Summary of Services:
Treat the flu, allergies, sinus infection, rash, sore throat, and
more. $0 Co-pay
Taking care of your mental health is an important part of
your overall well-being. With Teladoc’s Mental Health,
adults 18 and older can get care for anxiety, depression,
grief, stress, family issues, and more. Choose to see a
psychiatrist, psychologist, social worker, or therapist and
establish an ongoing relationship. $0 Co-pay

11
CITY EMPLOYEE MEDICAL CLINIC
The CEMC partners with UCCS staff nurse practitioners to
provide a multitude of services to meet your health care needs.
They offer on-site lab services and same day appointments
for acute and urgent care concerns, similar services to what
you would see at a primary care provider.
Preventive Care/ Wellness/Labs (Pay $0)
• Annual Physical & Wellness Exams
• Immunizations
• Children Physical Exams (ages 5+)
General Medicine (Pay $15)
• Chronic Care Services
• Acute Care Services (ages 3+)
• Health Diagnostics & Referrals
• Evaluation & Treatment of Injuries
• Smoking Cessation
• Weight Management
• Functional Medicine
• Gut Health
• Lab Services
• And so much more
CITY EMPLOYEE PHARMACY
The City Employee Pharmacy offers convenient, affordable
prescriptions, and excellent customer service.
• Home & Desk Delivery
• Validated Parking
• Text Alerts
• Refills
• Automated Refill Line (800) 573-6214
• Mobile App
• Over-the-Counter Medication
• Vitamins and Many Other Items
CardioRX (Pay $0)
• Cardiovascular health management programs
• Resources for healthy living
• Free cholesterol screenings & blood
pressure checks
• Waived co-pays for generic hypertension and
cholesterol medications, if enrolled and
engaged in the program
Diabetes Ten City Challenge (Pay $0)
• Diabetes management program (diabetic
and pre-diabetic)
• Resources for healthy living
• Co-pays waived for generic diabetes
medications, if enrolled and engaged in the
program
HEALTH SERVICES
pharmacy pic
Refer to the Vendor Directory for convenient hours and locations.
12
HEALTH SERVICES
ZERO HEALTH
Healthcare Simplified to $0 with your ZERO benefit!
We believe healthcare should be affordable, simple, and personalized. If you are enrolled in the medical plan you can get the
care you need for $0 (Yep. ZERO) and you will never have to worry about deductibles or copays.
With ZERO you have access to thousands of medical services and procedures through the Anthem provider network. You
can search for providers at www.zero.health and chat live with a Personal Health Assistant in just one click.
Some examples include:
• Surgeries (Ear Nose & Throat, Orthopedic, Spinal, Women’s Health)
• Preventive Screenings such as Colonoscopies and Mammograms
• Imaging (CT Scans, MRI, Ultrasound, X-Ray)
• Physical Therapy • Sleep Studies • Labs at Quest Diagnostics
Once your doctor recommends you need a procedure scheduled, follow these simple steps to get the care you need for $0!
1. Connect with your Personal Health Assistant to see if the service or procedure you need is covered.
You can call 855-816-0001, chat www.zero.health or email at help@zero.heatlh.
2. Your Personal Health Assistant will help you find the provider that works best for you and sends all
the details to the ZERO provider to get you scheduled for your procedure.
3. You get access to the care you need without having to worry about things like deductibles, copays
or coinsurance - you always pay $0. For real. You always pay ZERO.
ZERO’S Lab Partner is Quest Diagnostics. To pay $0 for all your lab work:
1. Ask your doctor or nurse to send your lab orders to Quest Diagnostics
2. You can go to the closest Quest Diagnostics location - just make sure to show your physical or digital
ZERO Member ID Card when you arrive. Access your digital copy at my.zero.health.
3. Quest Diagnostics will send the lab results to your prescribing physician and you pay $0!
For everything from minor sprains to chronic pain, Hinge Health offers a clinical care team
that uses advanced technology to manage member pain and remove barriers to recovery.
Personalized care from day one:
Integration of prior-authorization, claims, and medical history ensures continuously personalized care.
Ongoing customization:
Ongoing exercise, education, and behavioral plan customizations based on members’ real-time feedback and needs.
High-risk intervention:
Care coordination with in-person providers enables earlier intervention with technology like Enso, surgery decision
support, and more.
No matter where you have pain, Hinge Health has you covered, get the support you need at no cost to you or your
family if they are on the medical plan.

13
WELLNESS & HEALTH MANAGEMENT PROGRAMS
ALTERNATIVE MEDICINE
Medical plan participants can be reimbursed for alternative
medicine by completing and submitting a AmeriBen Claim Form.
Plan pays 50% of claims up to $1,000 annual maximum per
family for the following:
• Massage Therapy
• Rolfing
• Homeopathic
• Naturopathic
Plan pays 100% up to 16 visits (no maximum dollar amount)
per year for each covered member for the following:
• Dietician
• Nutritionists
AMERIBEN MATERNAL HEALTH PROGRAM
Maternal Health Benefit:
Baby Steps, AmeriBen’s Maternal Health program, provides
families with the following before, during, and after your
pregnancy at no additional cost to you:
• Education
• Support
• Specially Trained Maternal Health Nurse
TOBACCO CESSATION
Is it time to Quit using Tobacco? We have free resources to
assist you on this journey.
Tobacco Cessation program with Teladoc at no cost to you.
• Multifaceted program that combines health
coaching support, physician treatment, and
tobacco cessation content to help members
break their tobacco habit.
• 24/7 support when cravings hit.
• Celebrate the milestones at 7,20,90,120,
and 365 days!
• Work with physician and get free over-the-
counter medication with a script: Zyban,
Chantix, Nicotrol, nicotine gum, patches, and
lozenges
Download the app, call (800) 835-2362 or visit Teladoc.com
Tobacco Cessation with City Employee Medical Clinic.
Work with City Employee Medical Clinic staff to help you
kick the tobacco habit and to get free over-the-counter
medication with a script: Zyban, Chantix, Nicotrol, nicotine
gum, patches, and lozenges.
14
REACH YOUR PEAK YEAR 20 (RYP20)
Program Year: January 1, 2024 – November 30, 2024
A fully customized wellness program designed to help you reach your individual life, body, and/or mind goals. RYP20
offers planned wellness tracks or customizable experiences, which help you achieve balanced wellness.
Employee Points Spouse Points
Required: Primary Care 100 Points Required: Primary Care 100 Points
Provider Screening or Provider Screening or
Biometric Screening Biometric Screening
Total Points to earn incentive 400 Points Total Points to earn incentive 100 Points
Incentive $400 Incentive $100
For more information Visit the Benefits & Wellness Intranet
or contact the HR Solutions Center
(719) 385-5125 • [email protected]
15
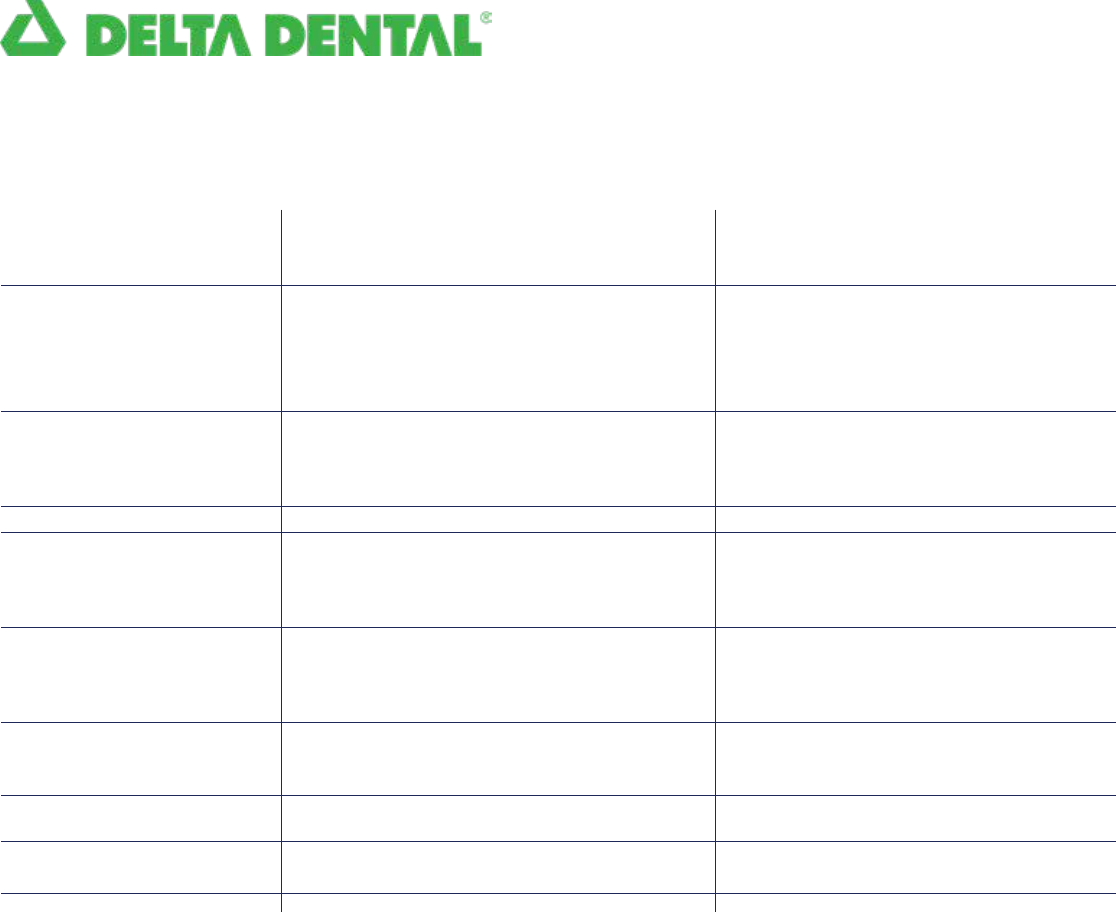
DENTAL INSURANCE
Dental coverage is available through Delta Dental of Colorado and you have two plans from which to choose: Delta Hi-Option
PPO and Delta Standard PPO. Both plans pay 100% for cleanings, oral exams, and x-rays when you use a PPO dentist.
Please refer to the current year’s Dental Plan Comparison and Rate Chart and/or the Delta Dental Plan Document for more
information or visit DeltaDentalCo.com.
Annual Maximum
Plan Will Cover
Annual Deductible
Per Person
Per Family
Routine Dentistry (2)
Cleaning
Oral Exams
X-Rays
Sealants (3)
Basic Dentistry (4)-(6)
Fillings
Extraction
Root Planning/Quadrant
Major Dentistry (6)
Crown (full cast)
Denture Repair
Bridge
Orthodontia
Orthodontic Benefit
Lifetime Maximum
Implant Coverage
Sleep Apnea Appliance
Lifetime Maximum
Prevention First
Type of Benefit Delta Hi-Option PPO (1) Delta Standard-Option PPO (1)
PPO Dentist Premier & Non- PPO Dentist Premier & Non-
Participating Dentists Participating Dentists
$1,500
per individual
$50
$150
(5) (6)
80%
80%
80%
80%
(5) (6)
50%
50%
50%
(5) (6)
50%
50%
50%
(6)
50%
$3,000
Surgical &
Restorative
60%
$3,000
Included
$2,000
per individual
$50
$150
100%
100%
100%
100%
90%
90%
90%
60%
60%
60%
(6)
60%
$3,000
Surgical &
Restorative
60%
$3,000
Included
$1,500
per individual
$50
$150
(5)
80%
80%
80%
80%
(5) (6)
50%
50%
50%
(5) (6)
50%
50%
50%
(6)
Not covered
Not covered
Not covered
50%
$3,000
Included
$1,500
per individual
$50
$150
100%
100%
100%
100%
80%
80%
80%
50%
50%
50%
(6)
Not covered
Not covered
Not covered
60%
$3,000
Included
Notes:
(1) Member and plan receive discounted contract pricing if a PPO & In-Network provider is utilized. The Non-Participating % of benefits is limited to the
non-participating Maximum Plan Allowance. You will be responsible for the difference between the non-participation Maximum plan Allowance and
the full fee charged by the dentist.
(2) Deductible does not apply to routine dentistry services.
(3) Sealants for permanent teeth for children through age 14 are a covered benefit on all plans as a routine dentistry service. Sealants for pre-molars are covered.
(4) Resin or composite filling will be covered at the same benefit as amalgam filling.
(5) Services received by a non-Participating dentist are reimbursed at the allowable Maximum Plan Allowance (MPA) for non-contracted dentist.
Members will be responsible for the difference between the allowable fee for non-contracted provider and the billed amount. By using a Delta Dental
contracted PPO or Premier provider, the member will not be balanced billed for the difference between the allowable Maximum Plan Allowance fee
and the billed amount, must be written off by provider. You will see the most savings with a PPO provider.
(6) The deductible applies to these services.
The plan will pay 60% PPO / 50% Premier & Non-Participating Dentists coinsurance for one occlusal mouth guard every 3 years to prevent grinding
when services are rendered by a covered dentist. Over the counter (OTC) mouth guards are excluded under the dental plans.
The coinsurance will apply towards the Annual Plan Maximum.
This table is not intended to include all benefit details. It is an outline of coverage available and is not intended to be a legal contract. If a discrepancy
exists between this document and the official Plan Documents, the Plan Documents govern.
17
VISION INSURANCE
Vision coverage is offered through VSP. This plan provides coverage once per plan year for routine eye exams, frames,
lenses, and contact lenses and provides other services such as preferred member pricing on contact lenses and direct
delivery to the home. Please refer to the current year Plan Summary and Rate Chart and/or Vision Plan Document for more
information. For the lowest cost visit a VSP provider. You can find in-network providers at vsp.com.
NEW: $0 exam copay and $0 Anti-reflective lenses when you visit a Premier Edge Provider.
Visit www.vsp.com/eye-doctor and select All Premier Edge Locations.
Well Vision Exam
Prescription Glasses
Frames
Lenses
Lens Enhancements
Average savings of 30% on
other lens enhancements
Contacts
(Instead of glasses)
You are not eligible for
eyeglasses and contact
lenses in the same benefit
period.
Diabetic Eyecare
Plus Program
Extra Savings
Your Coverage with
Out-of-Network Providers
Benefit Description Co-pay Frequency
Focuses on your eyes and overall wellness
$175 allowance for a wideselection of frames
$225 allowance for featuredframe brands
$95 allowance at Walmart/Costco 20%
savings on the amount over your allowance
Single vision, lined bifocal,and lined trifocal
lenses Polycarbonate lenses for dependent
children
Standard progressive lenses
Premium progressive lenses
Custom progressive lenses
Anti-Reflective lenses
$175 allowance for contacts;
co-pay does not apply
Contact lens exam (fitting and evaluation)
Retinal screening for members with diabetes
Additional exams and services for members
with glaucoma, or age-related macular
degeneration. Limitations and coordination
with your medical coverage may apply. Ask
your VSP doctor for details.
$20 or $0 Exam at
Premier Edge Provider
$15
$10
$0
$95 - $105
$150 - $175
$40 or $0 Premier Edge
Provider Up to $60
$0
$20 per exam
Every
calendar year
Every
calendar year
Every
calendar year
As Needed
As Needed
$0 copay and $0 antireflective coating if you see a Premiere Edge Provider!
Glasses and Sunglasses Extra $20 to spend on featured frame brands.
20% savings on additional glasses and sunglasses, including lens enhancements,
from any VSP provider within 12 months of your last Well Vision Exam.
Retinal Screening No more than a $39 co-pay on routine screening as an enhancement to
a Well Vision Exam.
Laser Vision Correction Average 15% off the regular price or 5% off the promotional
price; discounts only available from contracted facilities
Get the most out of your benefits and greater savings with a VSP network provider.
Call Member Services for out-of-network plan details.
Coverage with a participating retail chain may be different. Once your benefit is effective,
visit vsp.com for details.
This table is not intended to include all benefit details. It is an outline of coverage available and is not intended to be a legal contract.
If a discrepancy exists between this document and the official Plan Documents, the Plan Documents govern.

18
SPENDING ACCOUNTS
Spending accounts administered by Navia Benefit Solutions, offer a smart way to
stretch your paycheck by setting aside pre-tax dollars to pay for eligible health
and dependent care expenses. Each plan year (January 1 – December 31), you must
elect the annual amount you want to contribute to each account.
HEALTH REIMBURSEMENT ACCOUNT (HRA)
Employees enrolled in the Advantage Plan are eligible to
receive an employer-funded Health Reimbursement Account
(HRA). The annual funding level is based on your coverage
tier and prorated for new enrollees during the year. Annual
employer funding as of January 1:
Employees $500*
Employee + All other Tiers $750*
enrollments during the year.
*These amounts are pro-rated for mid-year plan
enrollments.
T
his account allows you to pay for certain medical, dental,
and vision expenses with tax free dollars funded by the City.
If you enroll in a pre-tax Flexible Spending Account (FSA) for
Health Care, you must first exhaust the balance in your FSA
before you can be reimbursed from your employer funded
HRA. The maximum HRA balance you may accrue is $8,000.
Submit claims by March 31 of the following plan year.
FLEXIBLE SPENDING ACCOUNTS (FSAs)
A Flexible Spending Account (FSA) for Health Care allows you
to allocate money on a pre-tax basis to reimburse yourself
for qualified medical, dental, and vision expenses for you and
your family. Qualified expenses include co-pays, deductibles,
prescriptions, and much more. You may rollover unused
monies into the following year, with a maximum allowed per
IRS regulations (see below).
An FSA for Dependent Care allows you to allocate money
on a pre-tax basis to reimburse yourself for dependent
care services. There is a “use it or lose it” rule with FSA for
Dependent Care meaning that, any contributions remaining
in your account that cannot be applied toward current year
dependent care expenses are not refundable.
Eligibility
Annual Contribution
Eligible Expenses
Availability of Funds
Payment or
Reimbursement Options
Rollover Amount
Service Deadline
Submission Deadline
for Reimbursement
Health Care FSA Dependent Care FSA
Eligible employees who are not enrolled in an
HSA on their spouse’s insurance
Minimum of $120 up to $3,050
Visit NaviaBenefits.com for a complete list
The full annual amount you elect is available
on your plan effective date
Debit card or reimbursement
Up to $610 (adjusted for inflation),
of unused funds
Services must be incurred by 12/31/2024
Claims must be submitted by 3/31/2025
All eligible employees
Up to $5,000
($2,500 if married and filing separately)
Care for children aged 12 and under,
disabled children and dependent adults
You can be reimbursed up to the amount
you have contributed
Debit card or reimbursement
Unused funds do not rollover
Services must be incurred by 12/31/2024
Claims must be submitted by 3/31/2025
For more information Visit the Benefits & Wellness Intranet
or contact the HR Solutions Center
(719) 385-5125 • [email protected]
19
LIFE INSURANCE
Life insurance offers financial protection for you and your loved ones when
experiencing loss through death. You are provided Basic Life and Accidental Death
and Dismemberment (AD&D) coverage by the City at no extra cost and can enroll in
supplemental Voluntary Term Life Insurance for yourself and dependents through
The Hartford.
New: Line of Duty benefit for Sworn employees includes an additional $50,000 death benefit.
Basic Life and AD&D = 1.5 X Annual Employee Salary
(Imputed income applies for benefit greater than $50K)
Voluntary Term Life Insurance (VTL)
New:
increased Guaranteed Issued Amount for employees is now $300,000.
Voluntary Term Life (VTL) Insurance can be purchased for yourself, spouse, and/or child(ren). Coverage is
available in increments of $25,000 for yourself and spouse and $5,000 for your child(ren).
No person may be insured as a dependent of more than one active employee under the policy.
Portable and convertible coverage available.
Tobacco rates apply for employee coverage. Must be tobacco-free for one year for non-tobacco user rate.
Insured Minimum Maximum Guarantee Issue
Employee $ 25,000 $ 500,000* $ 300,000
Spouse $ 25,000 $ 250,000 $ 50,000
Child(ren) $ 5,000 $ 25,000 $ 25,000
*You may not elect more than 10 times your annual
An Evidence of Insurability (EOI) is required
for employee coverage greater than $300,000
and for any new spouse coverage during
Open Enrollment. For spouse coverage,
you may increase VTL coverage by one
increment up to Guarantee Issue without an
EOI. Spouse coverage cannot be greater than
employee coverage.
Cost Example:
Desired Coverage Amount: $150,000
Age on January 1st: 35
Smoking Status: Non-Tobacco User
$150,000 / 1,000 = 150
150 x .07 = $10.50/Month
$10.50/Month / 2 = $5.25
Semi-monthly cost = $5.25
VTL Rate Structure Employee and Spouse
Age Bracket
Under 30
30-34
35-39
40-44
45-49
50-54
55-59
60-64
65-69
70-74
Over 74
Child(ren) per $5,000 = $0.72 per month
Non-Tobacco Tobacco User
User Per $1,000 Per $1,000
.04 .07
.06 .10
.07 .11
.08 .15
.11 .23
.17 .34
.32 .57
.50 .83
.97 1.37
1.64 2.79
2.06 2.85
These tables are not intended to include all benefit details. It
is an outline of coverage available and is not intended to be a
legal contract. If a discrepancy exists between this document
and the official Plan Documents, the Plan Documents govern.
20
DISABILITY INSURANCE
If you experience an injury or illness that prevents you from working, The Hartford disability insurance provides partial income
replacement to assist you financially. All benefit eligible employees may enroll in voluntary disability insurance. Premiums are
determined by Class (1,2,3, or 4), age, salary, and disability plan(s) elected. Disability Class is determined by PERA or FPPA
eligibility status.
SHORT-TERM DISABILITY (STD)
Short-Term Disability coverage provides you with partial income replacement if you are unable to work due to an illness,
including pregnancy, or injury that is non-work related.
NEW: Maximum weekly Gross Benefit is $1,500
*If vested with PERA (5 service years), including prior employment, you should notify the HR Solutions Center.
LONG-TERM DISABILITY (LTD)
Long-Term Disability coverage provides you with partial income replacement if you are unable to work for an extended
period due to an illness or injury.
PARTICIPANT DISABILITY CLASS SUMMARY (and examples)
Review Plan Documents for Complete Class Definitions
Voluntary STD (Accident or Illness)
Percent of Earnings Maximum Weekly Gross Benefit Waiting Period Maximum Benefit Duration
60% $1,500 7 days Class 1, 3, & 4: 25 Weeks
Class 2: 8 Weeks
Voluntary LTD (Accident or Illness)
Percent of Earnings Maximum Monthly Gross Benefit Waiting Period Maximum Duration
66.67% $7,500 180 days Varies see Plan Document
Class 1: PERA Defined
Benefit, not vested
Brett joined the City
as a Police Service
Representative in 2021.
Brett is enrolled in the PERA
Defined Benefit Plan but is
not vested under PERA.
Brett’s premiums are
calculated using Class 1
disability rates.
Class 2: PERA Defined
Benefit, vested
Tammy joined the
Accounting team in 2008.
Tammy is enrolled and
vested in the PERA Defined
Benefit Plan.
Tammy’s premiums are
calculated using Class 2
disability rates.
Class 3: Sworn,
covered under FPPA
John joined the City as a
Firefighter in 2021.
John is a member of the
FPPA.
John’s premiums are
calculated using Class 3
disability rates.
Class 4: PERA Defined
Contribution (DC)
Lilly joined the City in 2023
and works in Public Works.
Lilly is enrolled in the PERA
Defined Contribution Plan.
Lilly’s premiums are
calculated using Class 5
disability rates.
21
DISABILITY INSURANCE & FAMILY MEDICAL LEAVE
STD Rates LTD Rates
Age Bracket
18 – 24
25 – 29
30 – 34
35 – 39
40 – 44
45 – 49
50 – 54
55 – 59
60 – 64
65 Plus
Civilian & Sworn
Employees
(Classes 1, 3 & 4)
.094
.094
.084
.094
.105
.126
.147
.188
.230
.230
Civilian PERA
Vested/DB
(Class 2)
.044
.045
.045
.052
.056
.068
.080
.094
.100
.100
Civilian
Employees
(Classes 1 & 4)
.118
.144
.210
.288
.575
.930
1.213
1.336
1.218
1.218
CivilianPERA
Vested/DB
(Class 2)
.036
.047
.082
.113
.196
.349
.534
.637
.611
.611
Sworn
Employees
(Class 3)
.082
.108
.160
.241
.390
.683
1.074
1.290
1.203
1.203
STD Cost Formula: Cost Example: LTD Cost Formula:
$45,000 / 52 = $865.39 Annual Base Salary $45,000 $3,750 / 100 = $37.50
$865.39 *.6 = $519.23 Monthly Base Earnings $3,750 $37.50 x .683 = $25.61
$519.23 / $10 = $51.92 Retirement Plan FPPA $25.61 / 2 = $12.80
$51.92 x .126 = $6.54
$6.54 / 2 = $3.27 Age on January 1 45
Semi-monthly cost $3.27 Disability Class 3 Semi-monthly cost $12.80
Disability tables and summaries are not intended to include all benefit details. It is an outline of coverage available and is not intended to be a legal
contract. If a discrepancy exists between this document and the official Plan Documents, the Plan Documents govern.
22
LONG-TERM CARE INSURANCE
UNUM’s voluntary Long-Term Care (LTC) Insurance offers
peace of mind and financial assistance to support you, your
spouse, parents, or grandparents during a major life event
that limits one’s ability to perform at least two activities of
daily living: eating, bathing, continence, dressing, toileting,
and transferring.
Various coverage options are available and includes optional
inflation protection. Your premium depends on the insured’s
age when entering the plan, the plan elected, and if you elect
the inflation protection option
LTC provides benefits to help you pay
for care and facilities associated with:
• Home Health • Alzheimer’s
• Homemaker Services • Nursing
• Hospice • Personal Care
• Respite Care • Residential
• Rehabilitation
To enroll in coverage, unuminfo.com/coloradosprings/index.aspx. Fax, email, or mail
your enrollment to the address on the form. If you have questions about your coverage,
please contact UNUM Customer Service.
23
EMPLOYEE ASSISTANCE PROGRAM (EAP)
This FREE and confidential program through Profile EAP is available to all benefits-eligible employees and their eligible
dependents. EAP is a professional and completely confidential counseling service designed to help employees and
dependents resolve personal and/or work-related issues. EAP provides up to six (6) counseling visits for each problem
area, each year, at no charge. Participation in a City medical plan may help cover additional treatment if needed.
NEW: Same great service under a new name, Profile EAP is changing to CommonSpirit Health.
YOUR EAP PROVIDES SPECIALIZED SERVICES COUNSELING BENEFITS:
COUNSELING BENEFITS: Licensed, professional counselors to support with relationship
issues, family concerns, grief, stress, depression, or anxiety, substance abuse, and
workplace difficulties.
24/7 CRISIS SERVICE: Individual or group support with crisis situations, available 24
hours a day.
DEPRESSION CARE PROGRAM AND SLEEP CARE PROGRAM: Support with
exhaustion, sense of emptiness, loss of interest, trouble sleeping, and changes to mood
or appetite.
LIFE CYCLE SERVICES: Online platform to support with a wide array of work and life
topics (child/elder care, finances, legal, and so much more) of interest to you and your
family. Contact a Life Expert for additional support.
Visit: Profileeap.org
Company Code: COSPGS

FACE IT TOGETHER
Face It TOGETHER provides all benefit-eligible employees and their dependents access to
free, confidential peer coaching. Peer coaches have lived experience with alcohol and other
drugs – either personally or as impacted loved ones. There’s no judgment because they know
how it feels. Coaches provide professional, compassionate care at no cost to participants. All
services are kept private and adaptable to your individual or family needs. Sobriety isn’t
required and support is non-clinical.
Peer Coach: Your coach is your wellness partner, providing knowledge, support, and practical tools or accountability –
depending on your needs. Flexible, personalized approach means that you get the support you need in a way that is convenient
to your schedule.
Focused on improving every aspect of your life – not just the part that involves drugs or alcohol.
RETIREMENT
CIVILIAN PERACHOICE
City civilian employees and elected officials are members of the State of Colorado
pension system administered under State law by the Public Employees’ Retirement
Association (PERA) in lieu of Social Security. Participation is mandatory for eligible
employees and employees currently contribute 9% of PERA-includable salary to
their account. The City’s contribution for 2024 will be 14.78% (to include amortization
Equalization Disbursement (AED) & Supplemental Amortization Equalization Disbursement (SAED) of the same earnings to
the local government division. Employees hired after December 31, 2018, have the PERAChoice option and can choose to
be part of the PERA Defined Benefit (DB) Plan or the Defined Contribution (DC) Plan.
DEFINED BENEFIT (DB) PLAN
The PERA DB Plan is a hybrid defined benefit plan. It is
designed to attract and retain employees who are interested
in working in PERA-covered employment for a large part
of their careers, while providing greater portability than a
traditional defined benefit plan.
The PERA DB Plan offers a lifetime retirement benefit after
meeting age and service requirements and is sometimes
referred to as a pension.
DEFINED CONTRIBUTION (DC) PLAN
The PERA DC Plan is based on the money you have
contributed, and the investment earnings or losses incurred,
minus expenses. The PERA DC Plan may be attractive if
working in PERA- covered employment for only a small
portion of a career.
The amount of your retirement benefit depends on the
success of your investment decisions, when you begin
withdrawals, and your life expectancy - you bear the risk of
outliving your investments.
SWORN FIRE AND POLICE EMPLOYEES
All Sworn (Fire and Police) employees hired after 2006 are part of the FPPA
Statewide Defined Benefit (SWDB) Plan through the Fire and Police Pension
Association (FPPA) of Colorado in lieu of Social Security. Participation is mandatory
for eligible employees. To fund future pension benefits, employees contribute 12%
of FPPA-includable salary and the City contributes 10% of the same earnings. These
contribution rates are as of January 1, 2024.
The following types of retirement are available under the SWDB plan: normal, early, vested or deferred. If a member
terminates service before retirement eligibility, the member may qualify for a refund of contributions. Additional information
about FPPA benefits is available through FPPA.

26
VOLUNTARY RETIREMENT SAVINGS PLANS
In addition to your PERA and FPPA retirement benefits,
all City employees are eligible to participate in the voluntary
457 Deferred Compensation Plan, Roth 457, and/or Roth IRA.
457 DEFERRED COMPENSATION PLAN
The City of Colorado Springs encourages all employees to
actively participate in their retirement planning. New Hire
paperwork includes an automatic enrollment at a rate of 3%
into the 457 Deferred Compensation Plan. Participation in this
plan is not mandatory and employees may opt-out at any time.
Additionally, employees may enroll or make changes to their
retirement contribution anytime throughout the year.
Automatic 3% enrollment at hire
All employees can participate
Less restrictive than a 401(k)
Diversified Investment Options
Tax- Deferred Contributions
ROTH IRA
Employees have an additional retirement savings option
by investing in a Roth IRA. Roth IRA contributions can
start anytime with any dollar amount and contributions
are withheld directly from your paycheck as an after-
tax deduction. Investment earnings are tax-free at the
time of distribution and are accessible anytime, usually
without penalty.
ROTH 457
Employees also can participate in a Roth 457 plan
through MissionSquare in place of a traditional 457 plan.
In a traditional 457 plan, participants can make pre-tax
contributions that are then taxed along with the earnings
in retirement. Roth 457 contributions differ because they
are made after-tax and are not taxed when the assets are
withdrawn. Earnings may also be withdrawn tax-free if
certain criteria are met.

27
VACATION BUY, PAID TIME OFF, TUITION ASSISTANCE
VACATION BUY
Benefits eligible employees may purchase up to 40 hours of
vacation time pre-tax, based upon their hourly rate of pay
on January 1 of each benefit year. Vacation Buy can only
be elected during Open Enrollment, Qualifying Life Event,
or when newly hired with the City. Full-time employees may
purchase Vacation Buy in one-hour increments and the
minimum purchase amount is eight (8) hours. Vacation Buy
is calculated by multiplying the number of hours purchased
by your hourly rate and then divided by 24 (the amount
of benefit deducted paychecks in the year). Vacation Buy
purchased by new employees during the year use the
remaining number of paychecks (2 per month) during
the year. Vacation Buy hours purchased are available on
January 1 or upon election at the time of hire and must be
repaid if the employee uses Vacation Buy hours and then
separates employment before those hours are paid for. Any
unused Vacation Buy is paid back to employees annually in
December. Unused Vacation Buy hours do not roll over into
the next year.
TUITION ASSISTANCE
The City of Colorado Springs educational assistance program
provides financial support for job-related coursework. Regular
employees are eligible to receive tuition reimbursement for up
to two (2) classes per semester for undergraduate or graduate
coursework. Visit the Organizational Development Intranet
Site for more information.
PAID TIME OFF
The City offers work-life balance through its paid time
off benefits, which includes vacation leave, sick leave, a
personal day, and holidays. Information on paid time off
accruals and personal day eligibility are detailed in the
Civilian and Sworn Policies and Procedure Manuals (PPM).
City recognized holidays for 2024 are:
• New Year’s Day (01/01/2024)
• Martin Luther King, Jr. Day (01/15/2024)
• President’s Day (02/19/2024)
• Memorial Day (05/27/2024)
• Juneteenth (06/19/2024)
• Independence Day (07/04/2024)
• Labor Day (09/02/2024)
• Veteran’s Day (11/11/2024)
• Thanksgiving Day (11/28/2024)
• Day after Thanksgiving (11/29/2024)
• Christmas Eve (Civilian only) (12/24/2024)
• Christmas Day (12/25/2024)
Civilian employee: All benefit-eligible employees, non-shift
civilian employees will receive 8 hours of paid holiday time
on observed holidays, and one 8-hour personal day each
year after six (6) months of employment.
Sworn and shift employees: Please refer to the appropriate
Policies & Procedures Manual for details on how holidays
and personal days are paid.

28
EMPLOYEE PERKS
Nationwide® pet insurance is available for dogs,
cats, birds, and exotic pets. Plans include coverage for your
pet’s injuries and illnesses. Extra features include access
24/7 to a veterinary professional, emergency boarding, lost
pet assistance, and multi-pet discounts.
Call (877) 738-7874 or visit:
benefits.petinsurance.com/city-of-colorado-springs
UCCS Programs
We have partnered with UCCS to bring you a variety of
opportunities for wellness. Benefit-eligible employees and
their spouses can participate in up to 16 UCCS personal
training and/or 4 cooking classes per year at no cost. In
addition, you can participate in unlimited group fitness
classes and wellness workshops at no cost.
Email [email protected] for additional information.
Parking System Enterprises
City employees are eligible to receive a discounted monthly
parking card once they obtain a parking space if they park at
one of the City parking garages.
There are three (3) parking garages:
One is located on the southwest corner of Nevada and
Colorado Avenues (130 North Nevada) across the street from
the City Administration Building; another is located near the
current downtown City bus station at 127 East Kiowa Avenue;
the third is located at 201 North Cascade.
Exclusive discounts, special offers, and preferred seating to
top attractions, travel, shopping, tickets and so much more…
Visit: Ticketsatwork.com
Company Code: coloradosprings
Mountain Metropolitan Transit
City employees, on City business, can ride FREE. Simply
show your City ID badge. City employees also receive
generous discounts on bus passes. A bus pass can be
purchased at the Transit Administration Office, 1015 Transit
Drive, or through interoffice mail at MC 1449.
Call Transit Services at (719) 385-5974 or email
[email protected] for additional
information.
Note: Discounted bus passes are only available to employees
who are not receiving a discounted parking card.
Gym Discounts
We are currently partnered with VASA, Orangetheory, 9
Round, Barre Forte, YogaShield, Blitz45, Anytime Fitness,
LesMills on Demand, Progressive Fitness, Corepower Yoga,
Planet Fitness, and Yogashield to provide discounts on gym
memberships to all City employees.
For discounted tickets and special offers for
City of Colorado Springs Employees.
Visit www.broadmoorworldarena.com/Supergroup
Promo Code: Community 24
or Call (719) 477-2102 when purchasing 10+ tickets.
Additional discounts for Microsoft products, cell phone
services, and more are available. Visit the Employee Perks
section of the Benefits and Wellness intranet for more
information. Work Life Balance, including gym discounts, are
subject to change at any time and without notice.
DISCLAIMER OF ENDORSEMENT. Reference to any specific product or service on this section does not constitute an implied or express recommendation,
endorsement, or favoring by the City of Colorado Springs or its enterprises. Certain links lead to information and resources on servers maintained by third
parties and are provided as a convenience only. Neither the City of Colorado Springs nor its enterprises have control over these outside vendors or their
websites and are, therefore, not responsible, or legally liable for their web content or product or service offerings.

29
30
FAQ
s
Will I receive a Medical ID card? Yes! You will
receive a unique medical member ID number and medical
insurance card. If a medical ID card is not received, or to request a
replacement or additional medical ID card(s), contact AmeriBen.
Be sure to share your member ID card with your providers. To
request a replacement or additional medical ID cards, contact
AmeriBen at (866) 955-1482. You may also view your medical
ID card on www.myameriben.com or mobile app.
Will I receive a Prescription ID card? Yes!
You will prescription member ID card with the same
medical ID number. If a prescription ID card received, or to
request a replacement or additional prescription ID cards,
Contact Maxor Plus. To request a replacement or additional
prescription cards contact MaxorPlus at (806) 324-5430.
You may also view your prescription ID card on
www.maxorplus.com or mobile app.
Will I receive a Dental ID card? Yes! You
will receive Delta Dental ID cards. Members can also access
their dental ID card through the Delta Dental of Colorado
online member portal www.deltadentalco.com or the mobile
app. When you visit your dental provider, provide your 6-digit
employee ID with three leading zeros (five if Sworn) in place of
your social security number. (Example of 9-digit ID: 000XXXXXX)
Will I receive a Vision ID card? No - VSP does not
issue vision ID cards. You may view your member ID card
on the VSP member portal www.vsp.com or mobile app.
When you visit your vision provider, provide your 6-digit
employee ID number with three leading zeros (five if Sworn) in
place of your social security number. (Example of 9- digit ID:
000XXXXXX)
How do I access ZERO Health and receive $0
plan member cost for select services?
Contact
ZERO Health at (855) 816-0001, www.zero.health, or email
at [email protected]. You MUST contact ZERO Health PRIOR
to receiving care to have your plan member responsibility of
$0 for the service(s) rendered.
How do I access Hinge Health and receive $0
plan member cost for select services?
Contact
Hinge Health at (855) 902-2777.
Will member co-pays apply towards my annual
deductible and out-of-pocket maximum?
Member
co-pays do not apply towards your annual deductible;
however, co-pays do apply towards your out-of- pocket
maximum. This includes prescription and CEMC co-pays.
How do I find out information about the
tobacco premium surcharge?
Refer to the Tobacco
Surcharge FAQ, available on the Benefits and Wellness,
Medical Intranet page.
What can be treated through Teladoc?
• General Medicine • Behavioral Health
• Cold & flu symptoms • Stress
• Allergies • Addiction
• Bronchitis • Anxiety
• Respiratory Infection • Depression
• Tobacco cessation
Covered medical plan members have access to Teladoc
services at $0 member co-pay. The above list of services is
for illustrations, and additional services may be available.
Who is the Health Reimbursement Account
(HRA) and Flexible Spending Account (FSA)
Administrator for 2024?
Navia Benefit Solutions
(Navia) is our current provider.
How do I get reimbursed from my HRA and FSA?
You may submit claims to Navia via mail, fax, mobile app, or
online.
What is the timeline to request reimbursement
for my HRA and FSAs (Claim Run-Out Period)?
The HRA and FSAs are administered per plan year.
Participants can request reimbursement through the claim
run-out period for services incurred January 1 – December
31. The claim run-out period is 90 days, or January 1 – March
31, of the following year. Claims for 2024, therefore, must be
submitted for reimbursement by March 31, 2025.
How quickly will I receive my FSA or HRA
reimbursements?
Claims are processed daily. If you set
up a direct deposit with Navia, you will receive your money
faster than if they need to mail a check to your home. Visit the
Navia Benefits member portal to set up your direct deposit.
Debit cards are also available for immediate use.
What is an eligible expense for the HRA and
Health Care FSA?
Most allowable medical expenses
include co-pays for services or prescriptions, deductible
payments, dental work, frames, contact lenses, over-the-
counter medication, personal protection equipment (PPE),
feminine products, sunscreen and more. Contact Navia for
more information.
Who is eligible for the HRA? All employees who
enroll in the Advantage Plan will be covered under the HRA
unless they elect to opt out of the HRA benefit. Each year
the employer will contribute (tax free) $500 if enrolled in
employee only coverage and $750 if enrolled in any other
coverage tier. These amounts are pro-rated for new plan
enrollments during the year.
31
How does the HRA interact with my Health
Care FSA?
If you are enrolled in the Health Care FSA,
claims will be paid from the FSA first and then any remainder
paid from the HRA. Note: You cannot change this order of
payment.
Will I receive a debit card automatically if I
have an HRA or FSA?
Yes. Navia will automatically
send a debit card to HRA and Health Care FSA participants.
Debit cards are also available for Dependent Care FSA
participants, upon request through Navia. You can access
your HRA, and FSAs using one, convenient debit card. To
request additional or replacement debit cards free of charge,
contact Navia.
If you currently have a debit card, please keep this card for
use in 2024.
FAQs (cont) & HELPFUL REMINDERS
HELPFUL REMINDERS
Benefits Information
Learn all about your benefits by visiting the Benefits and
Wellness Intranet page. Let us help!
If you need help with your benefits, please contact the
HR Solutions Center at:
(719) 385-5125 or [email protected]
Coordination of Benefits
You must submit your Coordination of Benefits form to
AmeriBen on an annual basis. You may complete the COB
form and mail to AmeriBen, call the customer care center
at (866) 955-1482 or log into myameriben.com to update
your information.
Will I have to provide documentation when I
use my debit card?
You might. If documentation is
required to substantiate your claim, you will need to submit
the documentation to Navia as soon as possible to avoid
suspension of your debit card.
What happens if I do not provide substantiation
for debit card transactions?
Your debit card will
be deactivated, and the amount becomes taxable income
to you. Always remember to submit proper documentation
when required to substantiate your claims to Navia via fax,
mobile app, mail, or online.
Debit Card Documentation
If you are required to provide documentation that a debit card
was used for an eligible reimbursable expense – be sure to
follow through. Otherwise, your card will be deactivated, and
the expenses will be considered taxable to you.
Health Reimbursement Account (HRA)
Your entire Health Reimbursement Account (HRA) balance
(up to a max of $8,000) will carry over each year as long as
you remain enrolled in the Advantage plan. Remember to
submit for 2024 expenses by March 31, 2025. If you submit
for a reimbursement from your HRA for a dependent, you
will need to certify that the dependent is covered by a group
health plan.
Over-the-Counter Medications
Want to save money on your over-the-counter medications?
The City Employee Pharmacy offers a wide variety of items
at a great discount. Over-the-counter medications are
reimbursable under the HRA and Health Care FSA and are
available to all employees.
32
HEALTHCARE REFORM
The Patient Protection and Affordable Care Act (commonly referred to as ACA or Health Care Reform) is a federal law
passed in March of 2010 with the goal of improving the availability, affordability, and quality of health care coverage
in the United States. In its current form, the law has produced a steady stream of regulations and guidance by federal
agencies charged with clarifying employer requirements under the law. As your employer, we continue to implement
provisions to comply with the requirements of the health care reform law.
HEALTH CARE REFORM FAQS
Am I required to have health insurance? Health Care Reform required most U.S. citizens and legal immigrants to
have a basic level of health coverage (called “minimum essential coverage”) starting January 1, 2014, or else face a tax
penalty. This requirement under the law is called the individual mandate. In December 2017, Congress passed a new
law (the Tax Cuts and Jobs Act) that reduced the individual mandate penalty to zero starting in 2019. This means that
starting in 2019, there is no longer a federal individual mandate penalty for failure to maintain medical plan coverage.
What is the Health Insurance Marketplace? The Marketplace is comprised of state and federal run websites (called
Exchanges) where people can compare and buy individual policies for health care coverage. Plans on the Marketplace
may also be eligible for a tax credit that lowers monthly premiums. Anyone can purchase coverage through the
Marketplace and the plans may not deny coverage to those with pre-existing medical conditions. However, if you have
coverage through the City, you may not qualify for a premium tax credit or other savings. In Colorado, our Marketplace
is called “Connect for Health Colorado” where coverage can be purchased available at connectforhealthco.com. The
federal Marketplace website is healthcare.gov. People may only enroll in a Health Insurance Marketplace during the
Marketplace’s open enrollment period or if they have a special enrollment event permitted by the Marketplace.
What if I do not have any health care coverage in 2024? In December 2017, Congress passed a law (the Tax Cuts
and Jobs Act) that reduced the federal Individual Mandate penalty to zero starting in 2019. This means that starting in
2019 there is no longer a federal individual mandate penalty for failure to maintain medical plan coverage. Note that if
you are a resident of the District of Columbia or certain states, such as Massachusetts, New Jersey, California, Rhode
Island, or Vermont, you may be subject to a state income tax penalty if you fail to maintain medical plan coverage that
meets that state’s minimum coverage requirements. Currently, Colorado has not adopted any form of a state individual
mandate penalty.
NON-GRANDFATHER STATUS
The City medical plan is a “non-grandfathered” health care plan under the Patient Protection and Affordable Care Act
(Health Care Reform). Being a non-grandfathered plan means the plan must comply with certain consumer protections,
as outlined under Health Care Reform, which have been incorporated within this document. Questions regarding these
Health Care Reform provisions can be directed to the HR Solutions Center, or you may contact the U.S. Department of
Health and Human Services at healthcare.gov.
For more information Visit the Benefits & Wellness Intranet
or contact the HR Solutions Center
(719) 385-5125 • [email protected]
33
NOTICES
Notices are available on coloradosprings.gov for you to review during anytime.
You have the right to request and receive a paper copy of documents that have been provided electronically. You may
obtain these copies free of charge by contacting HR Solutions Center, at (719) 385-5125 or [email protected].
Please visit coloradosprings.gov/totalrewards/notices to review all notices listed below:
IMPORTANT REMINDER TO PROVIDE THE PLAN WITH THE TAXPAYER IDENTIFICATION NUMBER (TIN) OR SOCIAL
SECURITY NUMBER (SSN) - Employers are required by law to collect the taxpayer identification number (TIN) or social security
number (SSN) of each medical plan participant and provide that number on reports that will be provided to the IRS each year.
PRIVACY NOTICE REMINDER - The Health Insurance Portability and Accountability Act (HIPAA) of 1996 requires health
plans to comply with privacy rules.
AVAILABILITY OF SUMMARY OF BENEFIT AND COVERAGE (SBC) DOCUMENTS - The health benefits available to you
represent a significant component of your compensation package.
THE WOMEN’S HEALTH AND CANCER RIGHTS ACT OF 1998 ANNUAL NOTIFICATION - This act
requires health plans to provide coverage for reconstructive surgery and related services that may follow a mastectomy.
HIPAA SPECIAL ENROLLMENT NOTICE - After the open enrollment period is completed, (or, if you are a new hire, after your initial
enrollment election period is over), generally you will not be allowed to change your benefit elections or add/delete dependents
until next years’ open enrollment, unless you have a Special Enrollment Event, or a Mid-year Permitted Election Change Event.
NOTICE OF NEWBORN & MOTHERS HEALTH PROTECTION ACT - The Plan may not restrict benefits for any hospital
length of stay in connection with childbirth for the mother or newborn child to less than 48-hours following a vaginal
delivery, or less than 96-hours following a delivery by cesarean section.
NOTICE OF PRIVACY PRACTICES FOR PROTECTED HEALTH INFORMATION - It describes how
medical information about you may be used and disclosed and how you can get access to this information.
PATIENT PROTECTION RIGHTS OF THE AFFORDABLE CARE ACT – Designation of a Primary
Care Provider (PCP). The medical plans offered by the City of Colorado Springs do not require you to select a primary
care physician (PCP). You do not need prior authorization (pre-approval) from the Plan, the Claims Administrator, or
from any other person (including a primary care provider) in order to obtain access to obstetrical or gynecological (OB/
GYN) care from a health care professional in the network who specializes in obstetrics and/or gynecology.
NOTICES REGARDING THE “REACH YOUR PEAK” EMPLOYEE WELLNESS PROGRAM –
Describes the voluntary wellness program available to all City of Colorado Springs employees enrolled in the medical plan.
MEDICARE PART D NOTICE OF CREDITABLE COVERAGE - This notice has information about your current prescription
drug coverage with City of Colorado Springs and about your options under Medicare’s prescription drug coverage.
YOUR RIGHTS AND PROTECTIONS AGAINST SURPRISE MEDICAL BILLS - When you get emergency care or get treated
by an out-of-network provider at an in-network hospital or ambulatory surgical center, you are protected from balance billing.
In these cases, you should not be charged more than your plan’s copays, coinsurance and/or deductible.
PAID FAMLI MEDICAL LEAVE INSURANCE - The City of Colorado Springs (“City”) has decided NOT to participate in the
Colorado FAMLI program, per a vote of our governing body on September 27, 2022. This notice explains how the vote
affects City employees’ rights and benefits. You can learn more about the FAMLI program by contacting the Division at
CDLE_F[email protected] or by visiting famli.colorado.gov.
PREMIUM ASSISTANCE UNDER MEDICAID AND THE CHILDREN’S HEALTH INSURANCE PROGRAM (CHIP) - If you
or your children are eligible for Medicaid or CHIP and you are eligible for health coverage from your employer, your
state may have a premium assistance program that can help pay for coverage, using funds from their Medicaid or CHIP
programs.

YOUR BENEFITS INFORMATION FOR 2024!
